Abstract
Background: There is a strong demand for remote monitoring systems to gather health data. This study investigated the safety, usefulness, and patient satisfaction in outpatient care using telehealth with real-time electrocardiogram (ECG) monitoring after catheter ablation.
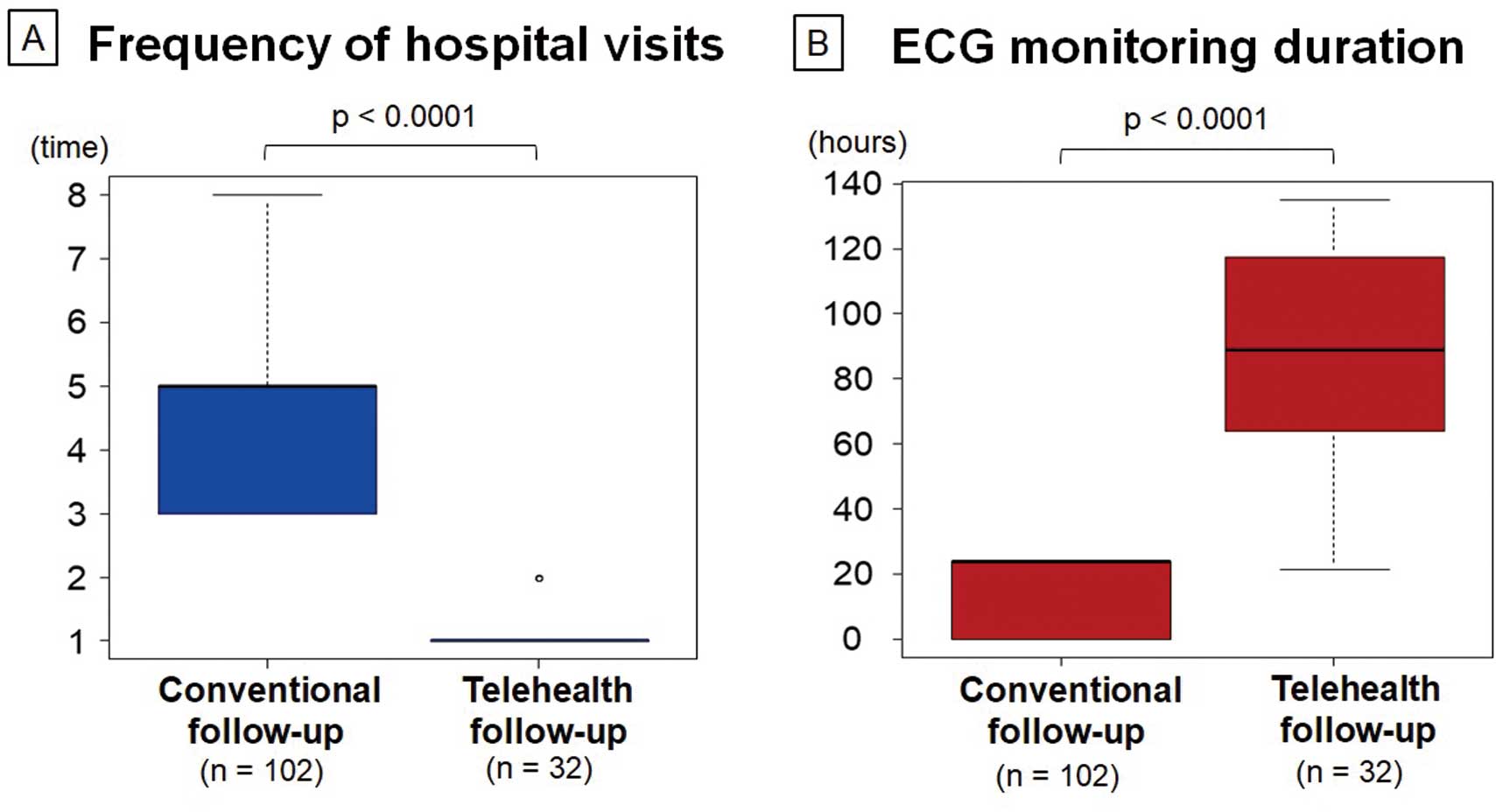
Methods and Results: In all, 38 patients who underwent catheter ablation were followed up using telehealth. At the 3- and 6-month follow-up, a self-fitted Duranta ECG monitoring device was sent to the patient’s home before the online consultation. Patients attached the devices themselves, and the doctors viewed the patients by video chat and performed real-time ECG monitoring. The frequency of hospital visits and the ECG monitoring duration were compared with conventional in-person follow-up data (n=102). The completion rate for telehealth follow-up was 32 of 38 patients (84%). The number of hospital visits during the 6 months was significantly lower with telehealth follow-up than with conventional follow-up (median [interquartile range] 1 [1–1] vs. 5 [3–5]; P<0.0001). However, the ECG monitoring duration was approximately 4-fold longer for the telehealth follow-up (median [interquartile range] 89 [64–117] vs. 24 [0.1–24] h; P<0.0001). No major adverse events were observed during the telehealth follow-up. Patient surveys showed high satisfaction with telehealth follow-up due to reduced hospital visits.
Conclusions: A combination of telehealth follow-up with real-time ECG monitoring increased the ECG monitoring duration and patient satisfaction without any adverse events.
The use of telehealth has been growing worldwide since the COVID-19 pandemic.1,2 However, one of the shortcomings of telehealth is the lack of access to a patient’s physical information during online consultations. In particular, the use of telehealth in patients with arrhythmias requires access to real-time electrocardiogram (ECG) data to understand the patient’s condition. Consequently, a strong demand has emerged for a remote monitoring system that would gather health data with a reduced or no need for in-person contact.
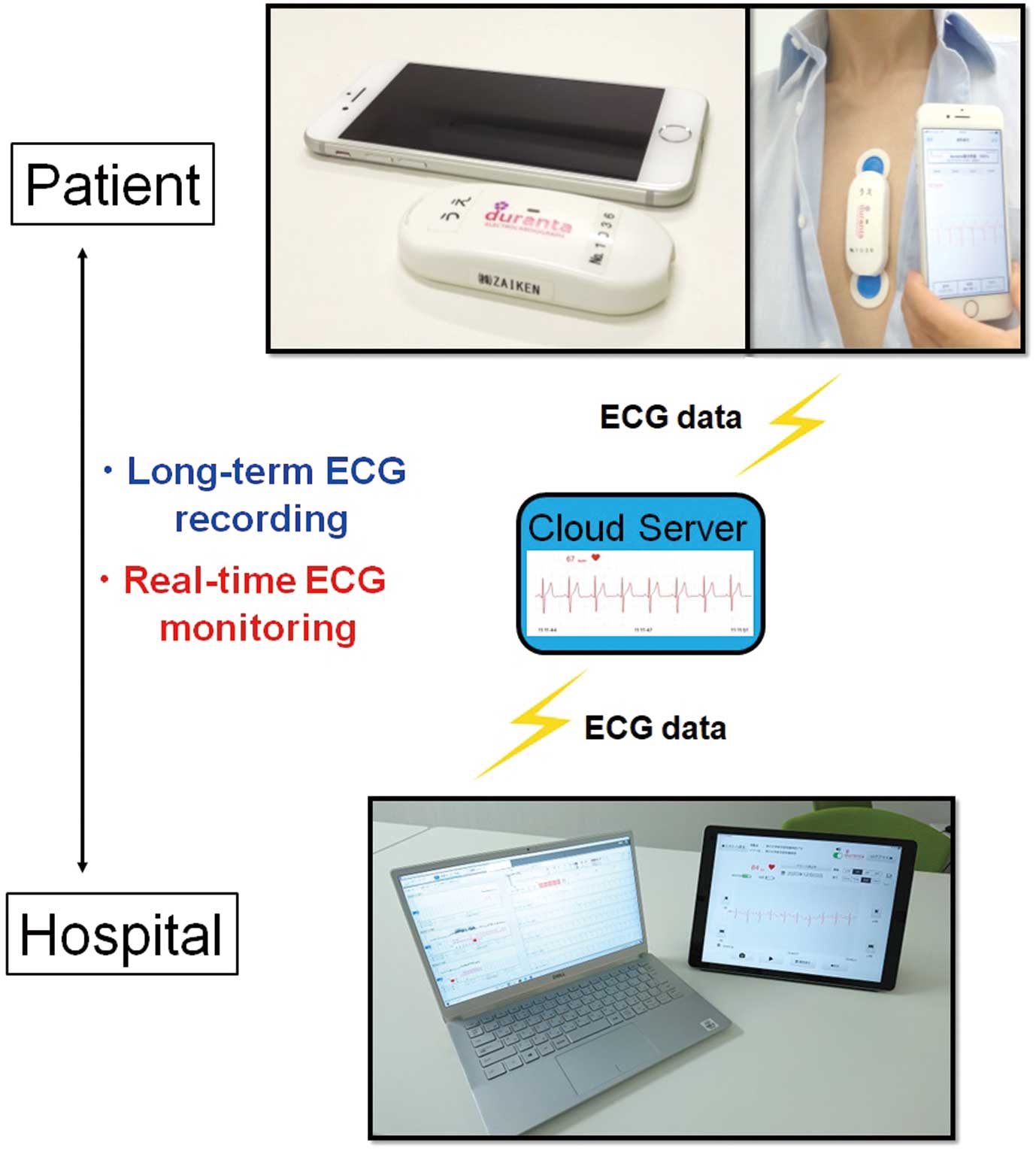
Catheter ablation therapy for arrhythmias has markedly developed in recent years, and the number of catheter ablations is rapidly increasing in Japan;3 however, this procedure carries a risk of recurrence of arrhythmia. Consequently, ECG monitoring and its duration are crucial factors for detecting arrhythmia after catheter ablation.1,4–6 We previously reported the practical utility of using the postal service for the delivery of patch-type, self-fitted, wearable ECG monitoring devices (Duranta; ZAIKEN, Tokyo, Japan) for the long-term ECG recording in outpatient care.7 The postal service safely delivered the ECG devices between the patients’ homes and the hospital, allowing the patients to perform long-term ECG recording themselves without needing to visit the hospital.
An as yet unexploited benefit of the Duranta ECG system is that it can transmit real-time ECG data to a cloud server. This raises the possibility that doctors in the hospital could remotely view real-time patient ECG data. We hypothesized that the combination of Duranta device delivery between patients and the hospital and the ability of the patients themselves to perform real-time ECG monitoring at home could be useful in online telehealth consultations. The aim of the present study was to investigate the safety, usefulness, and patient satisfaction generated by this novel style of telehealth follow-up for real-time ECG monitoring of outpatients after catheter ablation.
Methods
This was a prospective single-center cohort study. After undergoing catheter ablation for arrhythmias, the patients were informed about the details of the proposed online telehealth consultations. Patients who expressed willingness to participate in the study were enrolled from August 2021 to November 2022 at Kobe University Hospital, and all provided written informed consent. The study complied with the principles of the Declaration of Helsinki and was approved by the Ethics Committee of Kobe University Hospital (No. B200292).
Combination of Online Consultation and Real-Time ECG Monitoring
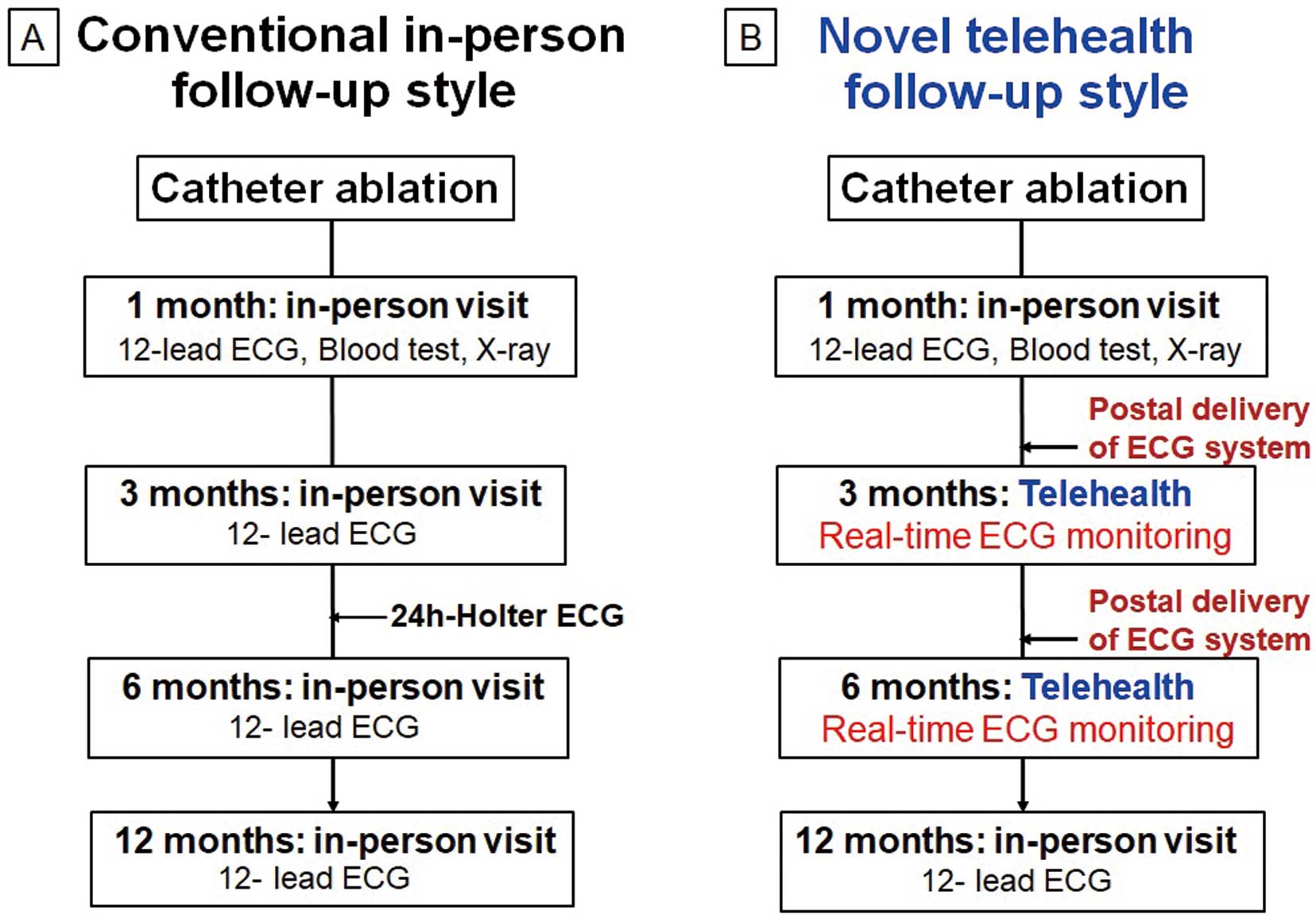
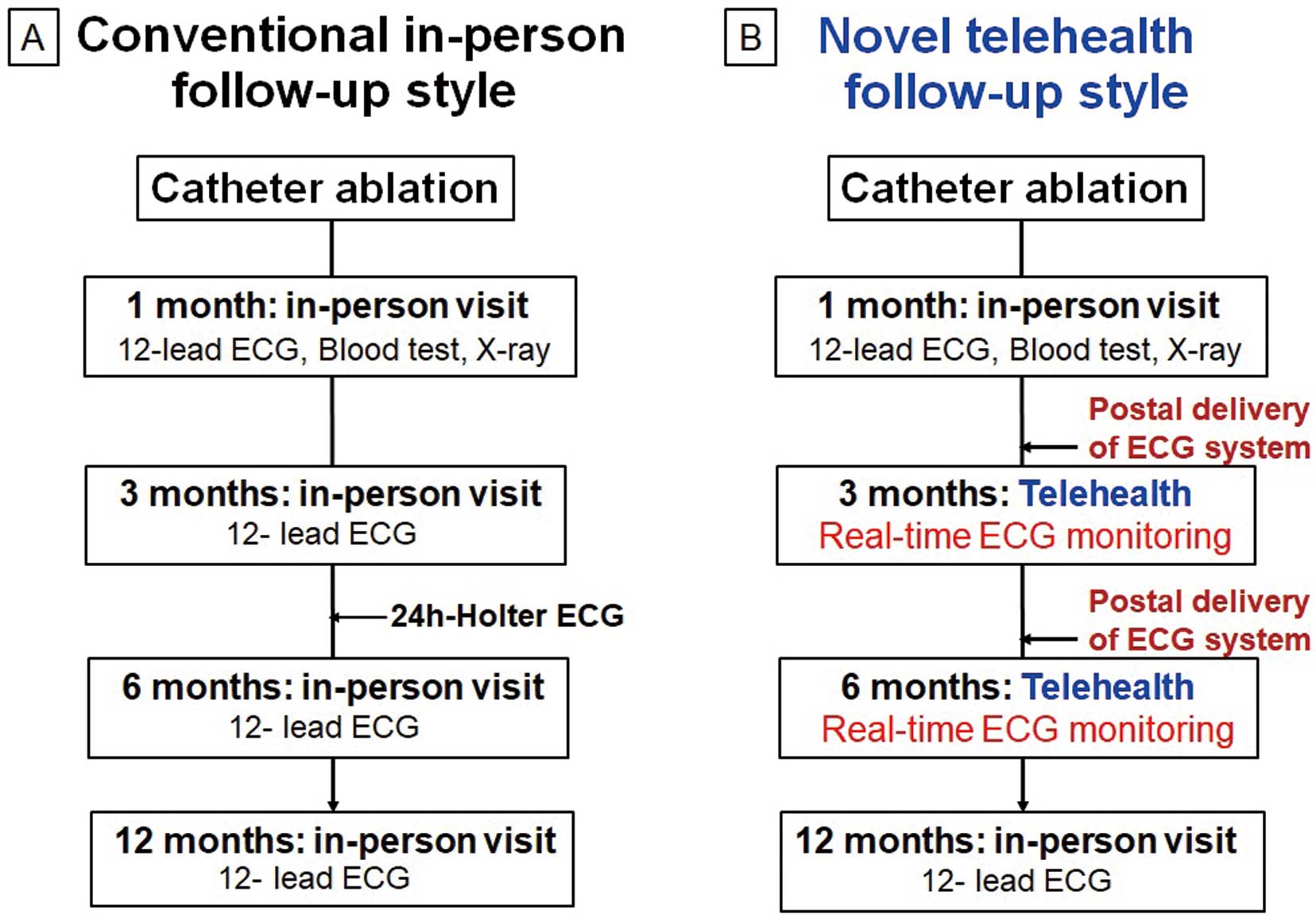
Overview Differences between the conventional in-person follow-up and the novel telehealth follow-up are shown in Figure 1. In the conventional in-person follow-up, patients visited the hospital at 1, 3, 6, and 12 months after catheter ablation and underwent a 12-lead ECG at each visit. A 24-h Holter ECG recording was also performed between the 3- and 6-month follow-up to detect any arrhythmia recurrence (Figure 1A). In contrast, patients enrolled in the novel telehealth follow-up used in the present study visited the hospital only at 1 month after catheter ablation. They then participated in the telehealth follow-up at 3 and 6 months, thereby eliminating the need for hospital visits at those times. At the 12-month follow-up, the patients again visited the hospital (Figure 1B). Data for the conventional in-person follow-up were obtained from 102 consecutive patients who underwent catheter ablation for arrhythmia at Kobe University Hospital between August 2020 and August 2021 (historical data).
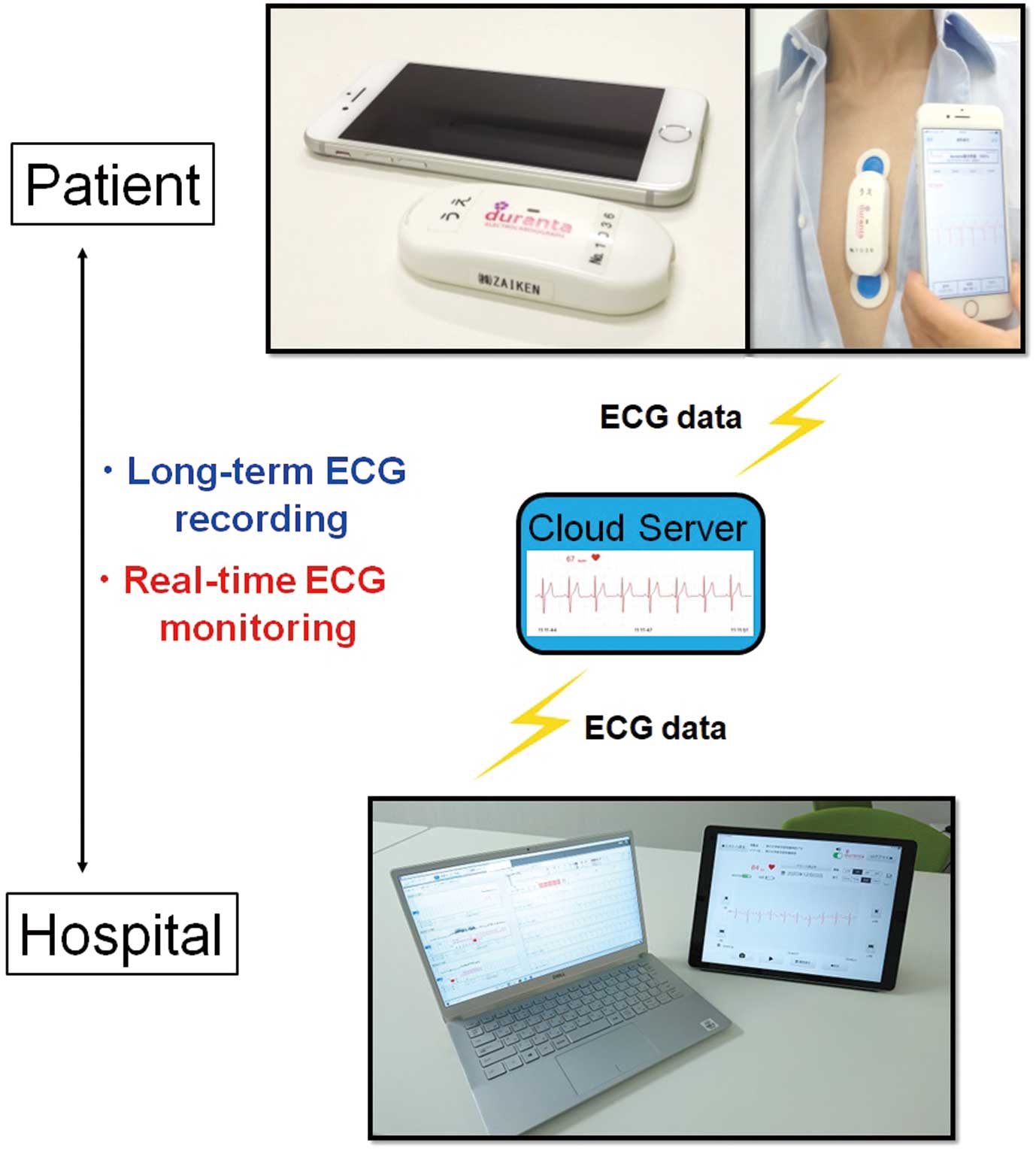
Duranta ECG Monitoring Device The details of the Duranta patch-type ECG monitoring device have been described previously.7–9 Figure 2 shows the characteristics of the Duranta ECG system. The Duranta is a small ECG device, measuring 78.4 mm wide, 35.1 mm deep, and 14.7 mm thick. It is lightweight, just 35 g, and easily attached to the chest with 2 patch electrodes. Its battery lasts 7 days before needing to be recharged. ECG data are sent automatically to a cloud server via an iPhone application. The Duranta works as both a long-term ECG recorder and a real-time ECG monitor. Medical staff access the cloud server with a personal ID and password, downloading ECG data to a hospital computer for analysis. Medical staff can also see real-time ECG data on an iPad. An analysis report of the long-term ECG data was uploaded as a PDF to the Duranta website, with the PDF of the report then printed and scanned into the hospital’s electronic health records.
In our previous paper,7 we described the utility and safety of postal delivery of ECG devices between patients’ homes and our hospital. We placed the ECG devices in prepaid Letter Pack Light envelopes (Japan Post), which can be put in any postbox in Japan. The Letter Pack Light envelope typically arrives at its destination within 1–2 days. The delivery status can be tracked on the Japan Post website.
Pocket Doctor Telehealth Application The Pocket Doctor telehealth application (OPTiM Corporation, Tokyo, Japan) was used for patients and doctors to communicate. The application was downloaded onto patients’ smartphones during their hospitalization for the catheter ablation. On the day of the online consultation, the patients and doctors were able to use the application to talk remotely, face to face. Video chats were handled as follows:
1. The doctor initiated the video call with the patient through Pocket Doctor, starting the video conversation.
2. Both the patient and physician confirmed each other’s identity.
3. Patients were asked about their recent well-being, symptoms, any ongoing issues, and medication adherence.
4. The doctor explained the results of the long-term ECG recordings and real-time ECG. In the event of arrhythmia recurrence, the doctor decided whether to change to an in-person visit.
5. At the end of the session, patients were briefed on the scheduling of upcoming appointments.
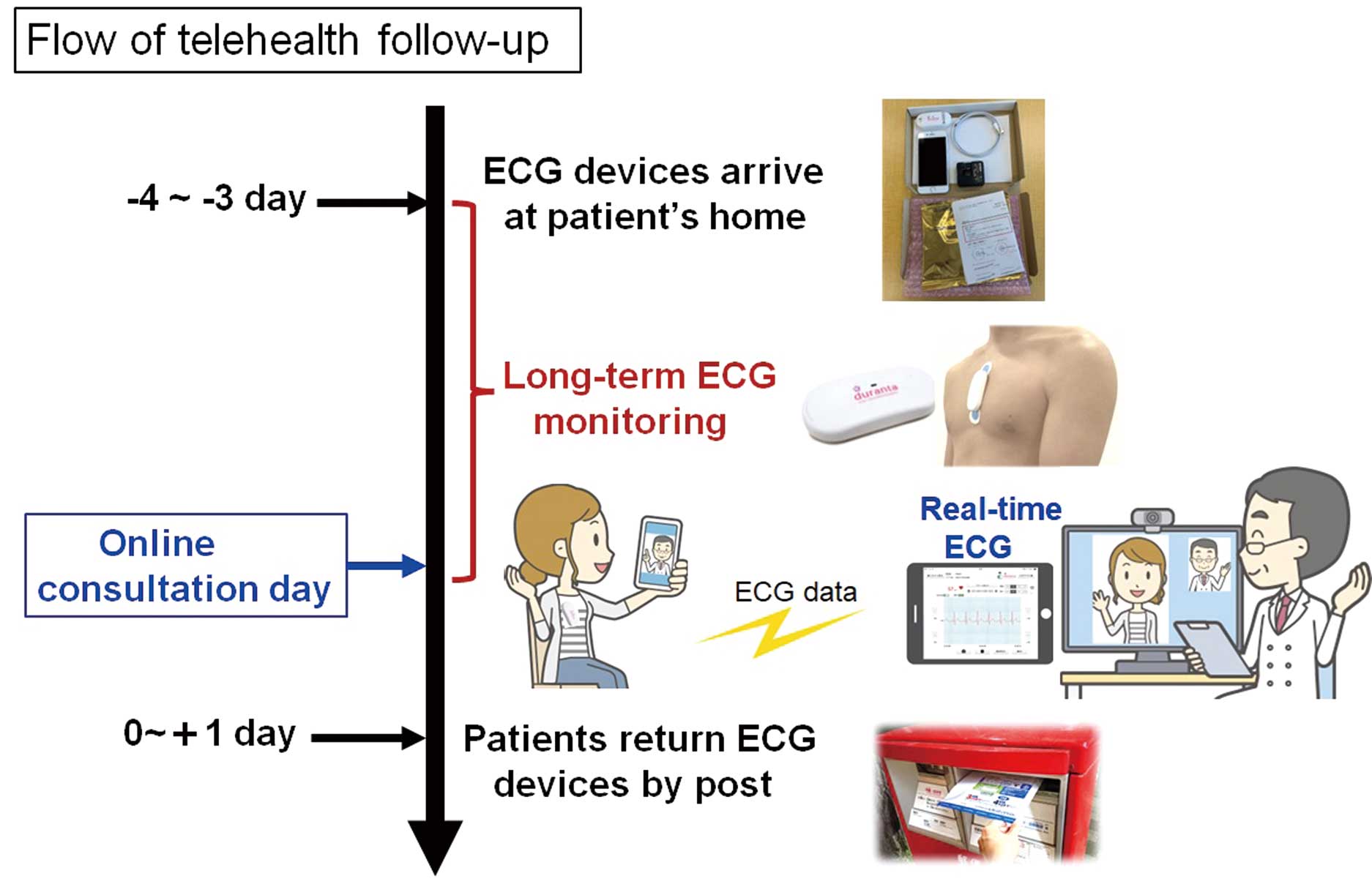
Online Consultation With Real-Time ECG Monitoring The process used for telehealth with real-time ECG monitoring is shown in Figure 3.
1. The Duranta ECG system arrived at patients’ homes 3–4 days before the telehealth consultation day. The patients attached the device themselves to initiate long-term ECG monitoring. Continuous ECG recordings were made for a duration of 2–4 days, with the exception of bathing times. Then, the patient participated in an online consultation while the continuous ECG monitoring was in operation, allowing for real-time ECG monitoring during the video chats.
2. Before the online consultation, the doctors accessed the Duranta cloud server to view the long-term ECG recording data to check for arrhythmia recurrence.
3. The doctors and patients participated in the online consultation using the Pocket Doctor application. The doctors conducted video chats with the patients while viewing the real-time ECG data transmitted by the patients’ Duranta devices.
4. The attending physician documented the examination findings and the conversation with the patient during the video chat in the patient’s electronic health record.
5. After the online appointment, the patients returned the Duranta ECG devices to the hospital by post.
Patient Satisfaction Survey A survey was conducted of patients who completed telehealth follow-up. The satisfaction survey questionnaires were sent to patients’ homes by mail and collected by return of post after they had been completed. The survey included the following questions:
• What is the overall level of satisfaction regarding telehealth with real-time ECG?
• Do you think ECG monitoring by mailing small ECG devices is convenient?
• What types of burdens can be reduced through the telehealth follow-up?
Items for Evaluation
The present study evaluated the following: (1) the completion rate for the telehealth follow-up after catheter ablation; (2) the frequency of hospital visits during follow-up; (3) the duration of ECG monitoring during follow-up; (4) the occurrence of adverse events (death, ischemic stroke, major bleeding, syncope, and unexpected hospitalization); and (5) the survey results for patient satisfaction with the telehealth follow-up.
The frequency of hospital visits and the ECG monitoring duration were compared between the conventional in-person follow-up (historical data) and the novel telehealth follow-up groups.
Statistical Analysis
The distribution of continuous variables was examined using the Shapiro-Wilk test for normality. For continuous variables with a normal distribution, data are presented as the mean±SD, whereas those without a normal distribution are presented as the median with interquartile range (IQR).
The 2 groups were compared using the Mann-Whitney U test. Two-sided P<0.05 was considered statistically significant, and all statistical analyses were conducted using R version 2.13.0 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Patient Characteristics and Follow-up Completion Rate
In all, 38 patients were enrolled and followed up with telehealth after catheter ablation. Table 1 presents characteristics of patients in the telehealth follow-up (n=38) and conventional in-person follow-up (n=102) groups. Mean patient age was significantly lower in the telehealth follow-up group than in the conventional in-person follow-up group (60±14 vs. 67±10 years; P<0.001).
Table 1.
Patient Characteristics
| |
Telehealth follow-up
(n=38) |
Conventional in-person
follow-up (n=102) |
P value |
| Age (years) |
|
|
<0.001 |
| Mean±SD |
60±14 |
67±10 |
|
| Range |
17–76 |
31–82 |
|
| Male sex (%) |
33 (87) |
77 (75) |
0.171 |
| BMI (kg/m2) |
24±3 |
24±3 |
0.715 |
| LVEF (%) |
63±7 |
61±10 |
0.349 |
| Arrhythmia type |
| Atrial fibrillation (%) |
26 (68) |
72 (71) |
0.837 |
| Atrial tachycardia, PSVT (%) |
9 (24) |
20 (20) |
0.642 |
| PVC, ventricular tachycardia (%) |
3 (8) |
10 (10) |
1.000 |
Unless indicated otherwise, data are given as the mean±SD or n (%). BMI, body mass index; LVEF, left ventricular ejection fraction; PSVT, paroxysmal supraventricular tachycardia; PVC, premature ventricular complex.
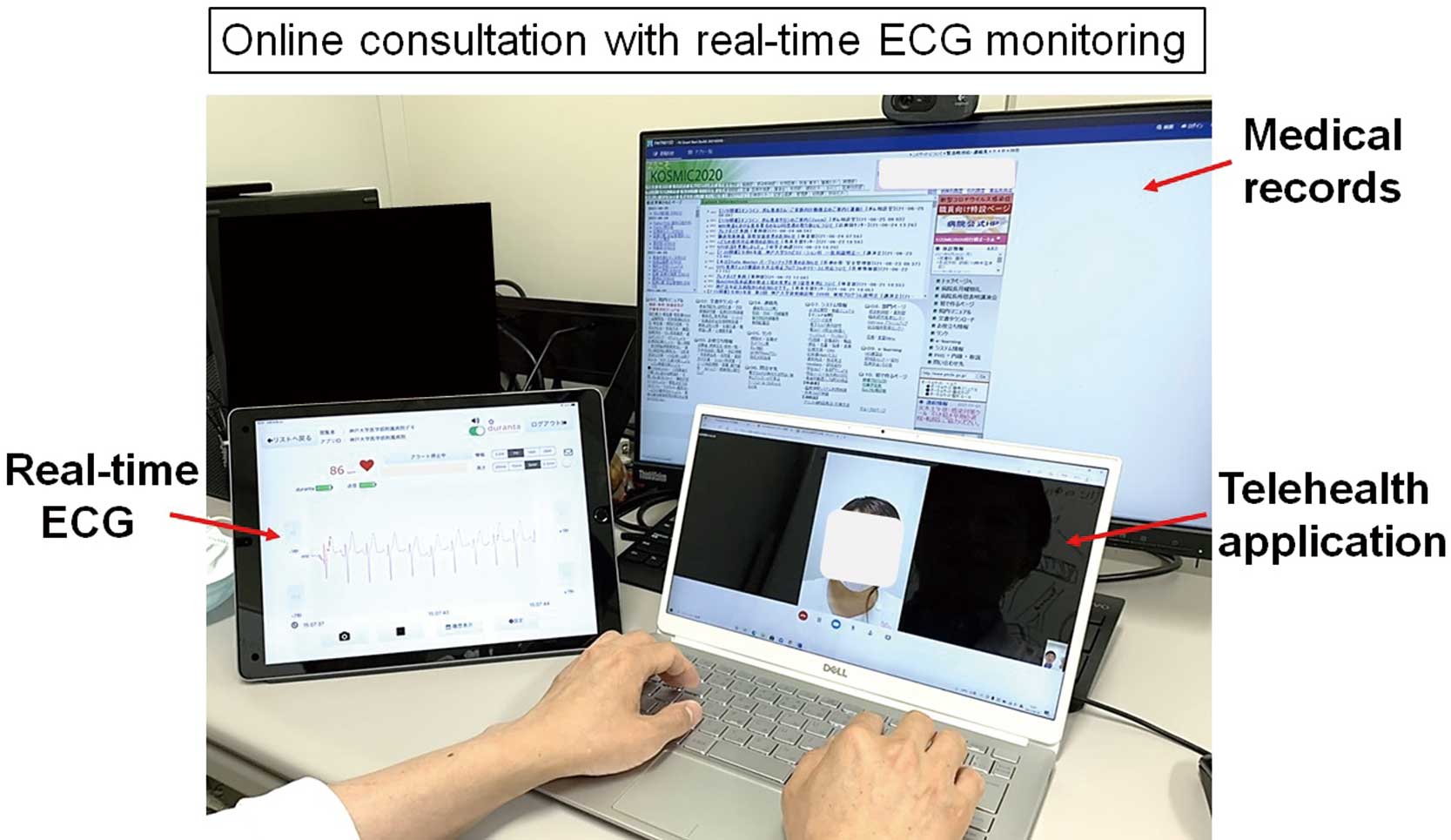
Figure 4 shows an image of an online consultation in the outpatient clinic. The real-time ECG monitoring movies of sinus rhythm and atrial tachycardia are shown in the Supplementary Movies 1 (sinus rhythm) and 2 (atrial tachycardia).
Table 2 presents follow-up data for the telehealth follow-up group. During the 6 months of follow-up, 32 of 38 patients (84%) completed the novel follow-up that used telehealth and real-time ECG monitoring. The reasons for not completing the novel follow-up were symptomatic recurrence of their arrhythmia in 4 patients, who were then changed to in-person visits because of the initiation of or change in their antiarrhythmic drugs or a scheduled cardioversion; and a request to change to in-person visits in 2 patients. These 2 patients agreed to participate in the study at first, but then wanted to change to an in-person visit before the first online consultation.
Table 2.
Follow-up Data in the Telehealth Follow-up Group (n=38)
| Follow-up completion rate |
32 (84) |
| Reasons for not completing telehealth follow-up |
| Recurrence of arrhythmia |
4 (11) |
| Change requested by patient |
2 (5) |
| Postal delivery troubles |
0 (0) |
| Mechanical trouble with ECG devices |
0 (0) |
| Network problems with telehealth application |
3 (8) |
| Adverse events during follow-up |
| Death |
0 (0) |
| Ischemic stroke |
0 (0) |
| Major bleeding |
0 (0) |
| Syncope |
0 (0) |
| Unexpected hospitalization |
0 (0) |
Data are presented as n (%). ECG, electrocardiogram.
ECG Devices and Telehealth Application
ECG monitoring was conducted for a median of 48 h (IQR 26–57 h) before every online consultation. Further, a median of 7 min (IQR 6–9 min) real-time ECG monitoring was conducted during the video chats.
No postal delivery troubles or mechanical troubles were encountered with the ECG devices. Network problems with the telehealth application during the online consultation occurred in 3 of 38 (8%) patients due to unstable Internet connections at the patients’ homes. This problem could be resolved by changing the patient’s location or by changing to a telephone.
Frequency of Hospital Visits and the Duration of ECG Monitoring
Figure 5 shows a comparison of the frequency of hospital visits and the duration of ECG monitoring during the 6-month follow-up between the conventional in-person follow-up and telehealth follow-up groups. There were significantly fewer hospital visits during the 6 months after catheter ablation in the telehealth follow-up group (median 1 [IQR 1–1] vs. 5 [IQR 3–5]; P<0.0001). However, the ECG monitoring duration during the 6 months was significantly longer in the telehealth than conventional in-person follow-up group (89 h [IQR 64–117 h] vs. 24 h [IQR 0.1–24 h]; P<0.0001).
Safety
No major adverse events (death, ischemic stroke, major bleeding, syncope, or unexpected hospitalization) were observed during the telehealth follow-up.
The system proposed in the present study has so far encountered no problems with regard to personal information protection and information security.
Patient Survey
In all, 32 patients who completed the telehealth follow-up answered the patient survey. The questionnaire items and results are shown in Figure 6. The overall level of satisfaction regarding telehealth with real-time ECG was “Extremely satisfied” in 75% of patients and “Somewhat satisfied” in 25% of patients. All patients agreed that “ECG monitoring by mailing ECG devices is convenient”. Most patients answered that the “time burden” could be reduced using telehealth follow-up.
Discussion
Nomura2 has reviewed the various digital health technologies currently in use in cardiovascular medicine. The review indicated that telehealth has gained particular recognition since the outbreak of the COVID-19 pandemic.2 However, the number of doctors conducting telehealth remains considerably lower in Japan than in European and North American countries.2
Telehealth offers several benefits, such as reduced expenses, increased flexibility, and an improved ability to serve individuals who are immobile or reside in remote regions without access to local healthcare facilities. However, telehealth has the disadvantage of being unable to conduct a physical examination, and this has been one of the factors hindering the widespread adoption of online healthcare in Japan. In the present study, we have provided evidence for the benefits of a new approach to telehealth in patients with arrhythmias while also offering several insights that could lead to the resolution of some of the disadvantages of using telehealth.
ECG Monitoring Device and Duration of Monitoring
Previous studies have shown that the duration of ECG monitoring and the use of monitoring devices greatly improved the detection of arrhythmia recurrence after catheter ablation.1,4–6 Generally, a 24-h Holter ECG examination is most often used to identify arrhythmia recurrence after catheter ablation. However, this procedure requires that patients visit the hospital several times to undergo the examination. The detection rate of arrhythmia was significantly lower with the 24-h Holter ECG than with 7-day ECG monitoring in patients after catheter ablation.6
Remote ECG monitoring systems using cardiac implantable electronic devices (CIEDs) are also in common use in clinical practice, because these devices can provide early detection of arrhythmias and device-related complications.10 However, the implantation is an invasive and costly procedure, and remote ECG monitoring using CIEDs is only possible in a limited number of patients with heart disease. An insertable cardiac monitor (ICM) has been reported to reveal a higher incidence of atrial fibrillation (AF) compared with other ECG monitoring devices.11 In Japan, however, medical insurance does not cover ICMs intended to confirm the recurrence of AF after catheter ablation therapy.
In the present study, postal delivery of ECG devices and self-recording of continuous ECG recordings enabled an approximately 4-fold longer duration of ECG monitoring compared with the conventional in-person outpatient care with the 24-h Holter ECG. Recently, Senoo et al5 showed the usefulness of daily home ECG measurements for device pairing ECG and blood pressure monitoring in patients who underwent catheter ablation. They reported that the use of an at-home ECG self-recording device provided better and faster detection of arrhythmia recurrence.5 Their approach to detecting arrhythmias differed from the approach we used in the present study; however, their results indicated that at-home ECG self-recording could work to detect arrhythmia recurrence.
Arrhythmia Type
In this study, we performed telehealth follow-up with real-time ECG monitoring in patients with various type of arrhythmias. It was difficult to determine the usefulness and efficacy for each type using this approach given our limited sample size. From our perspective, this approach would be well-suited for outpatient follow-up after AF ablation because postablation recurrence of AF is not uncommon. Moreover, the presence of recurrence detected through long ECG monitoring could impact decisions on discontinuing anticoagulation therapy and contribute to the prevention of stroke and/or heart failure.
Safety of Telehealth Follow-up
Telehealth follow-up was not a complete substitute for in-person visits. Late complications after catheter ablation, such as vascular troubles (arteriovenous fistula, pseudo aneurysm), periesophageal vagal nerve injury, and atrioesophageal fistula, were reported following catheter ablations.11 Therefore, in the present study, all patients underwent in-person visits 1 month after catheter ablation to check for these potential complications. Telehealth follow-up was then conducted at 3 and 6 months after ablation. Upon discovery of arrhythmia recurrence during a telehealth follow-up, the doctors determined whether the patient should change to in-person visits depending on their symptoms and the arrhythmia type. Consequently, no major adverse events occurred during the telehealth follow-up.
Protection of personal information is another matter of great significance in today’s digital age. In the present study, several measures were taken to ensure the security of patient information: (1) the Duranta ECG devices do not require input of patients’ personal information, thereby negating the possibility of any personal data breaches occurring during the delivery process; (2) the medical staff gain access to the Duranta cloud server using their personal ID and password, and access to any patient’s ECG data is restricted to authorized personnel only; (3) before an online consultation, both the patient and physician must confirm each other’s identities; and (4) the Pocket Doctor telehealth application is already in use in many medical institutions. Information security and privacy protection have been verified by the manufacuture of the telehealth application. No personal data leaks occurred in the present study.
Patient Satisfaction
At the beginning of the COVID-19 pandemic in 2020 in Japan, patients tended to avoid visiting hospitals/clinics due to fear of infection. Patient demand for telehealth therefore grew at that time. Since then, patients’ tendency to refrain from visiting hospitals has declined. The survey of patient satisfaction regarding the use of telehealth in the present study was conducted from 2022 to early 2023, and the survey results indicate that patients were highly satisfied with the telehealth follow-up, regardless of the COVID-19 pandemic. Most patients answered that their “time burden” could be reduced by telehealth.
The number of catheter ablations is increasing in Japan,3 and many patients undergoing ablation therapy are in their active working phase or are students. Therefore, frequent hospital visits after catheter ablation represent a significant time burden for patients and their families. Thus, online healthcare consultations, with their ability to reduce this burden, would increase patient satisfaction.
Study Limitations
This study has several limitations. First, this study was a single-center prospective study with a small sample size. In addition, the comparison between the telehealth follow-up group and the conventional in-person follow-up group was not conducted through a prospective randomized design, potentially introducing selection bias and differences in patient backgrounds that could have affected the results. Therefore, validation of the accuracy of our results will require a multicenter prospective study with a larger sample size. Second, the study enrolled only those patients who were capable of using a smartphone and accessing the Internet. This may have introduced selection bias and could have impacted the outcomes of the study. Third, telehealth visits are not a complete substitute for in-person visits. Therefore, patients with life-threatening arrhythmias or severe heart failure were not included in this study. Fourth, this study was not designed to investigate the cost, economic benefit, or burden on healthcare providers related to telehealth follow-up. If this novel style of telehealth follow-up was to be introduced in a hospital, creating an appropriate workflow tailored to the specific hospital and facilitating collaborative tasks among its medical staff would be desirable. Further studies are needed to investigate the influence of telehealth follow-up on the economic benefits and burdens to medical institutions.
Conclusions
After catheter ablation, a combination of telehealth follow-up with real-time ECG monitoring provided a longer ECG monitoring duration and high patient satisfaction without any adverse events in patients who were in a stable condition.
Sources of Funding
This work was supported by the Japan Society for the Promotion of Science KAKENHI Grants 22K08183. In addition, the study was supported by ZAIKEN and OPTiM. ZAIKEN loaned the ECG devices, and OPTiM loaned the telehealth application for this study.
Disclosures
The Section of Arrhythmia is supported by endowments from Abbott JAPAN, Medtronic JAPAN, and Boston Scientific JAPAN. The Section of Arrhythmia has received a scholarship fund from Biotronik JAPAN. K.H. chairs the Section, and K.F. and K.I. belong to the Section. However, none of the authors declare any conflicts of interest regarding this manuscript’s contents.
IRB Information
The protocol for this research project was approved by the suitably constituted ethics committee of Kobe University Hospital, and the project conformed to the provisions of the Declaration of Helsinki (Approval no. B200292).
Data Availability
The deidentified participant data will not be shared.
Supplementary Files
Supplementary Movie 1. Sinus rhythm.
Supplementary Movie 2. Atrial tachycardia.
Please find supplementary file(s);
https://doi.org/10.1253/circrep.CR-23-0083
References
- 1.
Varma N, Marrouche NF, Aguinaga L, Albert CM, Arbelo E, Choi JI, et al. HRS/EHRA/APHRS/LAHRS/ACC/AHA worldwide practice update for telehealth and arrhythmia monitoring during and after a pandemic. J Arrhythm 2020; 36: 813–826.
- 2.
Nomura A. Digital health, digital medicine, and digital therapeutics in cardiology: Current evidence and future perspective in Japan. Hypertens Res 2023; 46: 2126–2134.
- 3.
Kusano K, Yamane T, Inoue K, Takegami M, Nakao YM, Nakai M, et al. The Japanese Catheter Ablation Registry (J-AB): Annual report in 2020. J Arrhythm 2022; 38: 675–681.
- 4.
Kottkamp H, Tanner H, Kobza R, Schirdewahn P, Dorszewski A, Gerds-Li JH, et al. Time courses and quantitative analysis of atrial fibrillation episode number and duration after circular plus linear left atrial lesions: Trigger elimination or substrate modification: Early or delayed cure? J Am Coll Cardiol 2004; 44: 869–877.
- 5.
Senoo K, Yukawa A, Ohkura T, Iwakoshi H, Nishimura T, Shimoo S, et al. The impact of home electrocardiograph measurement rate on the detection of atrial fibrillation recurrence after ablation: A prospective multicenter observational study. Int J Cardiol Heart Vasc 2023; 44: 101177.
- 6.
Kim JY, Oh IY, Lee H, Lee JH, Cho Y, Gil Y, et al. The efficacy of detecting arrhythmia is higher with 7-day continuous electrocardiographic patch monitoring than with 24-h Holter monitoring. J Arrhythm 2023; 39: 422–429.
- 7.
Takami M, Fukuzawa K, Kiuchi K, Takemoto M, Nakamura T, Sakai J, et al. Practical utility of the postal service in delivering a self-fitted, wearable, long-term electrocardiogram monitoring device for outpatient care. Circ Rep 2021; 3: 294–299.
- 8.
Akiyama H, Nukui S, Araga T, Hoshino M, Tanaka K, Kashima S, et al. Utility of Duranta, a wireless patch-type electrocardiographic monitoring system developed in Japan, in detecting covert atrial fibrillation in patients with cryptogenic stroke: A case report. Medicine (Baltimore) 2017; 96: e5995.
- 9.
Hamada S, Sasaki K, Kito H, Tooyama Y, Ihara K, Aoyagi E, et al. Effect of the recording condition on the quality of a single-lead electrocardiogram. Heart Vessels 2022; 37: 1010–1026.
- 10.
Watanabe E, Yamazaki F, Goto T, Asai T, Yamamoto T, Hirooka K, et al. Remote management of pacemaker patients with biennial in-clinic evaluation: Continuous home monitoring in the Japanese At-Home Study: A randomized clinical trial. Circ Arrhythm Electrophysiol 2020; 13: e007734.
- 11.
Nogami A, Kurita T, Abe H, Ando K, Ishikawa T, Imai K, et al. JCS/JHRS 2019 guideline on non-pharmacotherapy of cardiac arrhythmias. Circ J 2021; 85: 1104–1244.