論文ID: CR-24-0042
論文ID: CR-24-0042
Background: Factor Xa inhibitors, such as rivaroxaban, are increasing the convenience of treatment for deep vein thrombosis (DVT). Limited evidence exists regarding clot evaluation at 3 months after treatment for DVT.
Methods and Results: We retrospectively analyzed the clinical course of symptomatic proximal DVT in patients who received 3 months of anticoagulation treatment at our hospital. Patients treated with the rivaroxaban single-drug approach were classified as group A (n=42). Patients treated with unfractionated heparin (UFH) or subcutaneous fondaparinux followed by vitamin K antagonist comprised group B (n=60) as an historical cohort. The quantitative ultrasound thrombosis (QUT) score was used to quantify clot burden before and after treatment. No significant differences were observed in patient characteristics between the groups. Serum D-dimer levels in both groups significantly improved after treatment. Clot volume assessed using QUT also reduced significantly in both groups. The QUT score in groups A and B improved from 7.5 [4.8, 12.0] to 3.0 [1.8, 5.0; P=0.000] and 7.0 [4.0, 9.8] to 3.0 [2.0, 5.0; P=0.000], respectively. The change in QUT (∆QUT) was significantly greater in group A compared with group B (−4.5 [−8.25, −2.0] vs. −2.0 [−6.0, 0.0]; P=0.005).
Conclusions: We were able to demonstrate the effectiveness of DVT treatment using rivaroxaban over a period of 3 months from onset, in terms of clot regression evaluated using the QUT score.
Venous thromboembolism (VTE), encompassing deep vein thrombosis (DVT) and pulmonary embolism (PE), necessitates prompt initiation of optimal anticoagulation for effective management.
Conventional bridging therapy for VTE involves intravenous unfractionated heparin (UFH), subcutaneous low-molecular-weight heparin (LMWH), or subcutaneous fondaparinux followed by a vitamin K antagonist (VKA) therapy. However, this approach requires frequent laboratory monitoring and dose adjustments, often leading to difficulties in achieving optimal dosing.1 In Japan, fondaparinux was approved for VTE treatment in 2011. Fondaparinux has become the primary therapeutic drug, partly because of the complexities associated with UFH. However, VKA therapy still necessitates frequent monitoring to maintain a therapeutic range.2
Direct oral anticoagulants (DOACs) emerged as a convenient alternative to bridging therapy, eliminating the need for routine monitoring. Their efficacy has been established through studies evaluating VTE recurrence rates, while safety assessments focused on bleeding events.3–5 Consequently, DOACs haves become the mainstay of VTE treatment worldwide. For treatment with rivaroxaban, a 3-week initial intensification therapy method is recommended: 15 mg twice daily for 21 days, followed by 20 mg once daily (15 mg once daily in Japan).3 Management of lower extremity DVT consists of two phases: the acute phase (encompassing the first 3–6 months after diagnosis), and the chronic phase (extending from 6 months to the rest of the patient’s life).6 However, limited evidence exists regarding the quantified assessment of DVT pathology at 3 months after onset. Recently, the concept of quantitative ultrasound thrombosis (QUT) score was proposed for DVT clot evaluation from Toho University.7,8 This study aimed to evaluate the effectiveness of a 3-month single-drug rivaroxaban regimen for VTE treatment compared with an historical cohort treated with VKA, using the QUT score for assessment.
This retrospective cohort study reviewed medical records of patients diagnosed and treated for symptomatic proximal DVT at the Division of Cardiovascular Medicine, Toho University Sakura Medical Center. DVT was diagnosed using venous ultrasonography and/or helical computed tomography. As shown in Figure 1, 77 patients with symptomatic proximal DVT treated using a single-drug approach with rivaroxaban were included in group A. Contrarily, 107 patients who had been treated with VKA since 2011 were included in group B as an historical cohort. In total, 184 patients with symptomatic proximal DVT and/or PE at the first event were retrospectively investigated. As shown in Figure 2, exclusion criteria were inadequate venous ultrasonography or blood test assessment after 3 months of treatment and a QUT score of <3, potentially indicating a minor case. Finally, 102 patients (42 in group A and 60 in group B) were included in the present study. In group B, 23 patients were treated with intravenous UFH followed by VKA, and 37 with subcutaneous fondaparinux followed by VKA. UFH or fondaparinux was administered until VKA control could be achieved at an international normalized ratio (INR) ≥2. Fondaparinux (7.5 mg) was administered by subcutaneous injection once daily (to adjust for weight differences, in place of 7.5 mg, 5 mg was administered for body weights below 50 kg, and 10 mg for body weights above 100 kg). The time in the therapeutic range (TTR) was 52% in group B.
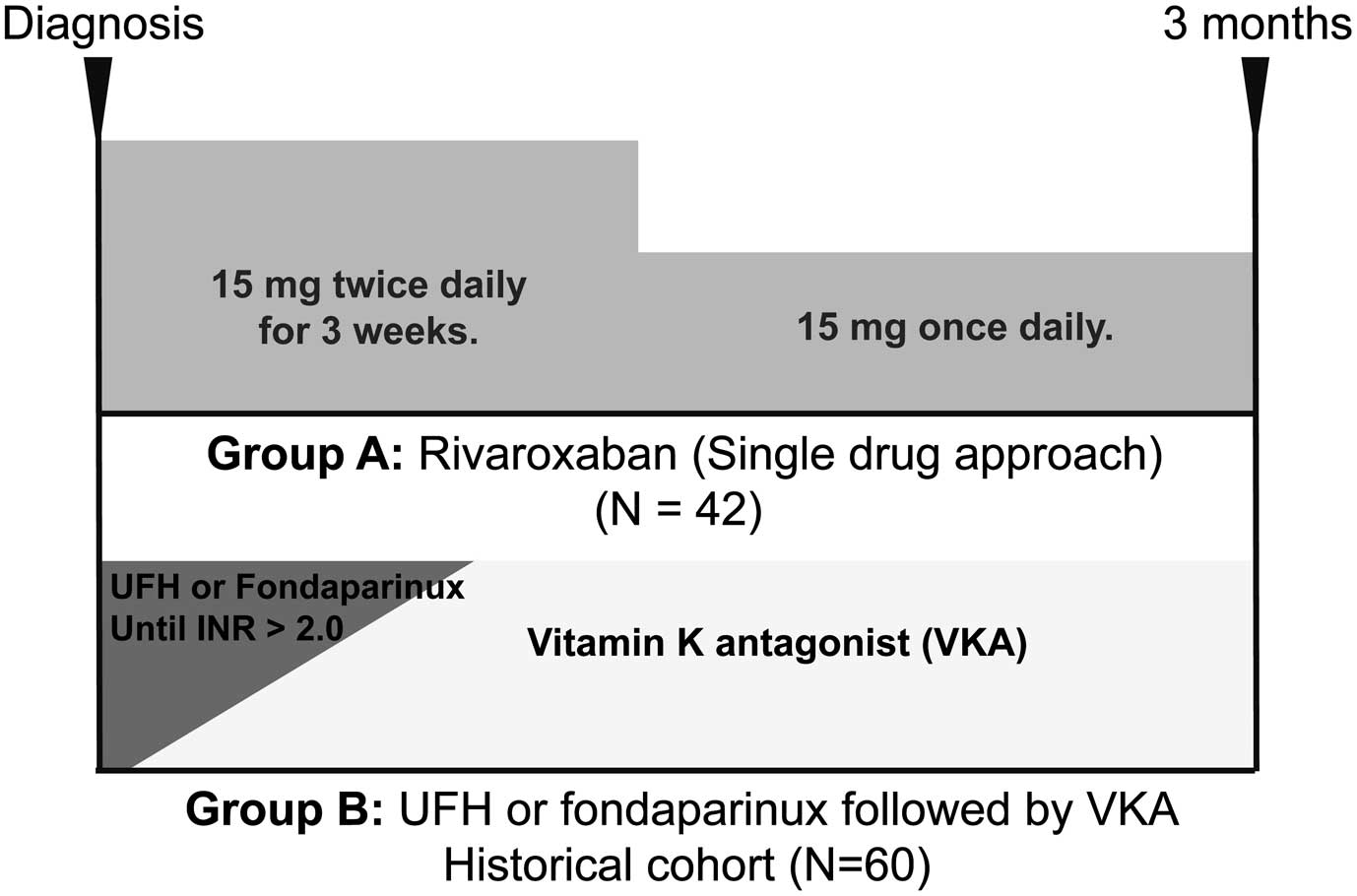
Course of anticoagulant treatment regimens for deep vein thrombosis. Group A received a single-drug approach with rivaroxaban. Group B received initial treatment with either unfractionated heparin or subcutaneous fondaparinux, followed by vitamin K antagonist therapy.

Selection process for the study sample. The study was selected according to the flow chart. Group B was an historical cohort of patients previously treated at our hospital (since 2011).
Venous Ultrasonography in Lower Limbs and QUT Score Measurement
Venous ultrasonography was performed by well trained sonographers following the recommendations of the Japan Society of Ultrasonics. Patients were positioned supine for iliac and femoral vein evaluations and sitting for popliteal and calf vein assessment. Full venous congestion was ensured before scanning. The sonographers confirmed a non-collapsed vein using B-mode ultrasound transverse imaging and probe compression.
We evaluated DVT clot volume using the QUT score as described previously.7,8 In the QUT scoring system, the deep veins were separated into 11 segments: inferior vena cava, right pelvic vein, left pelvic vein, right and left femoral veins, and right and left below-knee veins. When multiple below-knee vein thromboses were present, each thrombosis was evaluated separately. A score of 2 was assigned to complete vein occlusion by a clot, and 1 point for the presence of partial occlusion or non-occlusive clots. The sum of points across all segments determined the final QUT score.
Statistical AnalysisAll data are expressed as mean (±SD) or median with interquartile range (IQR), or number (%) as appropriate. The Mann-Whitney U test and chi-square test were used to compare patient characteristics and clinical parameters. Normality tests were conducted using the Shapiro-Wilk test. The Spearman’s correlation coefficient was used to determine the correlation between D-dimer levels and QUT scores. Wilcoxon’s signed-rank test assessed changes in QUT scores and D-dimer levels before and after treatment. The comparison of the difference in QUT scores before and after treatment between Group A and Group B was conducted using the Mann-Whitney U test. Statistical significance was set at P<0.05. Statistical analyses were performed using SPSS software (version 22.0; IBM Corp., Chicago, IL, USA).
EthicsThis retrospective, single-center study was approved by the ethics committee of Toho University Sakura Medical Center (approval number: S22036). The study adhered to the principles of the Declaration of Helsinki. Information about the study was disclosed on the institutional website and the potential participants were given the opportunity to opt-out.
Baseline characteristics of the 102 patients (42 in group A and 60 in group B) are summarized in Table 1. No significant differences were observed between the groups in terms of age, sex, anthropometric measures (height, body weight, body mass index [BMI]), obesity (defined as BMI >25 kg/m2), medical history (i.e., steroid use, current smoking, hormonal contraceptive use, chronic obstructive pulmonary disease, infection, recent surgery, cancer, chemotherapy, fragility), diabetes mellitus, or hypertension. Additionally, no significant differences were observed in serum creatinine, hemoglobin, and D-dimer levels at baseline. There was one unprovoked patient (62-year-old man) in group A and none in group B. No bleeding event was observed in either group. In group B (VKA), during the treatment period, worsening of DVT and development of symptomatic PE were observed in 1 patient (25-year-old woman) who was receiving chemotherapy for ovarian cancer. In that patient, prothrombin time-INR was 2.08 and D-dimer was 28.72 μg/mL at the last assessment before the onset of the event.
Patient Characteristics
| Variable | Group A: Rivaroxaban (single-drug approach) (n=42) |
Group B: UFH or fondaparinux followed by VKA (n=60) |
P value |
|---|---|---|---|
| Age (years) | 71 [63, 75] | 69 [56, 77] | 0.681 |
| Male sex | 22 (52) | 28 (47) | 0.681 |
| Height (cm) | 162 (±9) | 160 (±10) | 0.410 |
| Body weight (kg) | 64.0 (±12.3) | 61.4 (±14.4) | 0.384 |
| BMI (kg/m2) | 24.2 (±3.5) | 23.6 (±4.1) | 0.333 |
| BMI >25 kg/m2 | 18 (43) | 20 (33) | 0.406 |
| Steroids user | 4 (10) | 8 (13) | 0.757 |
| Current smoking | 8 (19) | 18 (30) | 0.253 |
| Hormonal contraceptives | 1 (2) | 2 (3) | 1.000 |
| COPD | 2 (5) | 4 (7) | 1.000 |
| Infection | 3 (7) | 7 (12) | 0.519 |
| Recent surgery | 3 (7) | 10 (17) | 0.329 |
| Cancer | 15 (36) | 20 (33) | 0.835 |
| Chemotherapy | 6 (14) | 11 (18) | 0.788 |
| Fragility | 14 (33) | 30 (50) | 0.108 |
| Diabetes | 6 (14) | 18 (30) | 0.096 |
| Hypertension | 13 (31) | 21 (35) | 0.831 |
| Creatinine (mg/dL) | 0.75 [0.60, 0.90] | 0.77 [0.60, 0.98] | 0.822 |
| Hemoglobin (mg/dL) | 13.0 [11.7, 14.2] | 11.8 [10.3, 14.2] | 0.090 |
| D-dimer (μg/mL) | 10.0 [5.6, 16.8] | 10.8 [5.0, 25.3] | 0.620 |
Data presented as mean(±SD), number (%), or median [IQR]. Fragility was defined as one or more of the following criteria: calculated creatinine clearance (CCR) <50 mL/min, body weight <50 kg, or age >75 years. BMI, body mass index; COPD, chronic obstructive pulmonary disease; UFH, unfractionated heparin; VKA, vitamin K antagonist.
The distribution of DVT location within the lower limb was comparable between both groups (Table 2).
Presence of Deep Vein Thrombosis
| Group A: Rivaroxaban (n=42) |
Group B: UFH or fondaparinux followed by VKA (n=60) |
P value | |
|---|---|---|---|
| Right femoral vein and/or more proximal | 18 (43) | 25 (42) | 1.000 |
| Right popliteal vein | 15 (36) | 22 (37) | 1.000 |
| Right calf vein | 17 (40) | 30 (50) | 0.421 |
| Left femoral vein and/or more proximal | 21 (50) | 39 (65) | 0.155 |
| Left popliteal vein | 21 (50) | 29 (48) | 1.000 |
| Left calf vein | 27 (64) | 35 (58) | 0.681 |
Data presented as number (%). UFH, unfractionated heparin; VKA, vitamin K antagonist.
In both groups, serum D-dimer levels significantly improved after 3 months of anticoagulant therapy (P=0.000 for both groups A and B). In group A, D-dimer levels decreased from 10.0 [5.6, 16.8] to 0.5 [0.5, 1.0] μg/mL. In group B, D-dimer levels decreased from 10.8 [5.0, 25.3] to 0.5 [0.5, 2.3] μg/mL. However, the change in D-dimer levels (∆D-dimer) between baseline and follow-up did not differ significantly between the groups (P=0.741). The values were −9.1 [−14.9, −5.0] to −9.7 [−19.6, −3.1] μg/mL.
A statistically significant positive correlation was observed between serum D-dimer levels and QUT scores in the entire sample (n=102) at baseline (r=0.339; P=0.000) and after 3 months of treatment (r=0.252; P=0.012).
The clinical course of DVT after 3 months of anticoagulant treatment is shown in Figure 3. The clot volume, as assessed using the QUT score, was significantly reduced in both groups (P=0.000). The median QUT score in group A improved from 7.5 [4.8, 12.0] to 3.0 [1.8, 5.0], while the median QUT score in group B improved from 7.0 [4.0, 9.8] to 3.0 [2.0, 5.0]. The change in QUT score (∆QUT) was significantly greater in group A than in Group B (P=0.005; Figure 4). Furthermore, the ∆QUT score in group A improved from −4.5 [−8.25, −2.0] to −2.0 [−6.0, 0.0], while the ∆QUT score in group B improved from −7.0 [−11.0, −2.0] to −2.0 [−6.0, 0.0].

Quantitative ultrasound thrombosis (QUT) scores in patients with deep vein thrombosis before and after treatment. A statistically significant decrease was observed after anticoagulant treatment in both groups.

Comparison of change in quantitative ultrasound thrombosis (∆QUT) score between groups A and B. Group A was statistically improved compared with group B.
Large clinical trials typically assess the outcomes of VTE anticoagulant therapy based on all-cause mortality or symptomatic VTE recurrence. This approach is preferred owing to the difficulty of performing detailed, high-quality ultrasound evaluation in such large studies.
Recent guidelines from America, Europe, and Japan recommend 3 months of anticoagulant treatment in patients with VTE secondary to recent surgery or transient non-surgical risk factors. Extended treatment is advised for patients with active cancer or unprovoked VTE. However, limited evidence exists regarding the clinical course of thrombi at 3-months post-intervention due to the lack of objective, quantitative evaluation indicators. Since the publication of the QUT score by Hisatake et al,7,8 our institution has incorporated it into the standard assessment of lower-limb DVT ultrasounds. Continuous numerical evaluation is particularly useful for monitoring the progress of individual patients. In Japan, the open-label, randomized J-EINSTEIN DVT and PE program reported that rivaroxaban (n=47) significantly reduced DVT compared with the control treatment with UFH and VKA (n=12).9 However, this assessment relied on a categorical scale (improved, normalized, unchanged, deteriorated) rather than continuous variables. Additionally, the VKA sample size was very small.
Yamashita et al recently reported a retrospective study using the QUT score to compare the efficacy of fondaparinux in patients with and without cancer (n=80 and n=180, respectively).10 Traditionally, DVT treatment outcomes were solely evaluated by considering all-cause mortality, recurrent DVT, and bleeding events requiring transfusion. The QUT score has made it possible to examine the course of DVT treatment as a continuous numerical value. Furthermore, its application does not require specialized ultrasound equipment once healthcare providers understand the concept.
Clinicians treating DVT empirically observe clot regression with appropriate anticoagulation therapy. However, even with specialist care, maintaining the time in therapeutic range (TTR) can be challenging, as demonstrated in clinical trials such as the Einstein DVT Study (TTR 58%), AMPLIFY VTE (61%), and Hokusai VTE Study (TTR 64%).3–5 DVT treatment aims to prevent clot extension, acute PE occurrence, DVT recurrence, and post-thrombotic syndromes. Therefore, prompt initiation of effective anticoagulation is crucial after diagnosis.
In the present study, as shown in Figure 4, the effect of clot regression using the single-drug approach with rivaroxaban showed excellent potential despite its easier management compared with VKA management.
Study LimitationsThis study has several limitations. First, it was a single-center, retrospective observational study. Unlike in the prospective study, the number of cases available for analysis was limited to 42 of 77 (77%) cases in group A, and 60 of 107 (56%) cases in group B. Second, the TTR was slightly lower (52%) than that in previous large clinical trials. This survey revealed that in actual clinical practice, even in a specialized outpatient clinic, it is difficult to ensure that VKAs are administered properly from the onset of VTE to 3 months thereafter. Third, VKAs are almost no longer used in the DOAC era. In Japan, three DOACs can be used for VTE: rivaroxaban, apixaban and edoxaban. There are no clear criteria for which DOAC to use, it is at the discretion of the physician in charge. Therefore, the present study may be subject to selection bias.
This study investigated the use of a single-drug approach with rivaroxaban compared with traditional VKA therapy for treating DVT. While the retrospective design and limited sample size limit the generalizability of our findings, the results suggest promising potential for rivaroxaban in achieving clot regression as assessed using the QUT score. The ability of the QUT score to provide a continuous, quantitative evaluation of clot burden may be a valuable tool for monitoring treatment efficacy. Further well designed, prospective studies with larger patient populations are warranted to confirm these findings.
The authors appreciate the members of the Clinical Functional Physiology department at Toho University Sakura Medical Center for their contributions to ultrasonography.
None declared.
The studies and data collection were conducted according to protocols approved by the ethics committee of Toho University Sakura Medical Center (approval number: S22036).
The deidentified participant data will not be shared.
Please find supplementary file(s);
https://doi.org/10.1253/circrep.CR-24-0042