2015 Volume 61 Issue 1 Pages 32-37
2015 Volume 61 Issue 1 Pages 32-37
The present study investigated the role of intensive care units (ICU) during disasters, including the responses of our ICU following the Great East Japan Earthquake on March 11, 2011. Our ICU comprises 8 beds for postoperative inpatients and those with rapidly deteriorating conditions; 20 beds in an emergency unit for critically ill patients; and 17 beds for neonates. It is important to secure empty beds when a major disaster occurs, as was the case after the Great Hanshin Earthquake, due to the resulting large numbers of trauma patients. Therefore, each ICU section cooperated to ensure sufficient space for admissions following the Great East Japan Earthquake. However, unlike the Great Hanshin Earthquake, securing beds was ultimately unnecessary due to the nature of the recent disaster, which also consisted of a subsequent tsunami and nuclear accident. Therefore, air quality monitoring was required on this occasion due to the risk of environmental radioactive pollution from the nuclear disaster causing problems with artificial respiration management involving atmospheric air. The variability in damage arising during different disasters thus requires a flexible response from ICUs that handle seriously ill patients.
The magnitude 9.0 earthquakes known as the Great East Japan Earthquake occurred at 14: 46 on March 11, 2011. The earthquake generated a massive tsunami that took numerous lives, and resulted in partial nuclear meltdowns at Fukushima Daiichi Nuclear Power Plant, the consequences of which have yet to be fully resolved. As a major base hospital of this region, we conducted a medical response, such as severe trauma patients, exposure patients and patients from hospital evacuation, in unprecedented complex disaster. In this study, based on these experiences, we examined how ICUs should respond during a disaster by retrospectively reviewing the responses of our ICU department in the acute disaster phase.
Fukushima Medical University Hospital is a general hospital in a 10-story building with 778 beds and 30 departments, which was completed in 1987. The intensive care units (ICUs) consist of a general ICU with 8 beds for inpatients needing postoperative management and those with sudden deterioration; emergency medical care center ICUs (4 ICUs, 4 coronary care units [CCUs], 12 high care units [HCUs]) with 20 beds for severely ill or trauma patients. Our hospital also has neonatal ICUs and maternal fetal ICUs, although these were excluded from this study.
Our hospital functions as the core disaster key hospital1) in Fukushima Prefecture, and it is the secondary radiation emergency hospital2). It is located in the northern middle of Fukushima Prefecture, 57 km from the Fukushima Daiichi Nuclear Power Plant. The numbers of outpatients and inpatients on the day of the earthquake were 1,345 and 642, respectively.
Although a strong quake was felt, there was almost no building damage; the water supply stopped but the electricity and medical gas supplies were maintained. While it is not certain how many outpatients were still in the hospital when the earthquake occurred, outpatient medical examinations were suspended after confirming that no outpatients had been injured, after which outpatients were urged to return home. Furthermore, we had inpatients return to their own rooms and confirmed their safety. Because the elevators had stopped, some of the inpatients being examined on lower floors were transported to upper floors by stretchers using the stairs. These initial responses were based on the judgments of department managers, and were completed without major disturbance. All staff members were confirmed to be safe by the managers of each department. Thereafter, the disaster headquarters was established in the hospital director's room to consolidate information from hospital departments and to establish a reporting line.
Although there were 6 inpatients when the earthquake occurred, routine medical care continued because the lifeline was maintained. As the ICUs were adjacent to the operating rooms, 2 patients were admitted to each booth, so that an additional 9 patients undergoing operation could be accommodated. After admitting postoperative patients, there were no more admissions of patients that day, making it unnecessary to change the work shifts of physicians and nurses.
Emergency ICUsAt the time of the earthquake, there were two patients in the ICUs, three in the CCUs, and seven in the HCUs; however, to prepare for the transportation of numerous injured people, patients with relatively mild conditions, and who could be transported, were transferred to hospital wards with secure empty beds. The work shifts of physicians and nurses were substantially changed because many of them were allocated to the Disaster Medical Assistant Team (DMAT)3) in the area.
Few patients admitted to our hospital had crush syndrome, which was a more common ailment during the Great Hanshin Earthquake. Instead, the most frequently observed ailments requiring intensive care were tsunami lung and hypothermia. While many patients with such diseases were admitted to hospitals located on the coastal front line, some were transported to our hospital, including those from the coastal area. We received 33 red triage patients, (i.e., patients who were judged to be in a severe condition within 4 days after the earthquake) and seven of them required intensive care.
Evacuation from hospitals5,6)In evacuating patients from hospitals in the surrounding area because of the nuclear accident, our hospital primarily acted as a relay point for transport to distant locations. Most of the evacuating patients were those with chronic disease, and none of them required intensive care. In addition, because of the suspension of scheduled surgeries, there were few patients in the general ICUs; therefore, nursing staff could be dispatched to manage patients who were admitted temporarily.
Responses associated with the nuclear disaster7,8)The explosion in Reactor No. 3 at the Fukushima Daiichi Nuclear Power Plant resulted in an increase in environmental radioactive substance concentration—that is, the ambient dose—in the area surrounding the hospital (Fig. 1). Although the dose rate within the building was approximately one tenth of that outside the building, the main concerns were pollution of the mechanical ventilators that compressed air from the external environment, which would in turn pollute the ICU department. However, the ambient doses in each department were low (Fig. 2), and investigation at a later date showed that many of the radioactive substances had been captured in the air conditioner filters (Fig. 3, Table 1). In addition, we measured the thyroid radiation dose in the staff of the ICU department and, to alleviate their anxiety, showed them the results, which were essentially equivalent to the background radiation and showed no radiation exposure.
As a secondary radiation emergency hospital, our hospital is a highly clean, positive pressure facility with two beds in the General ICU devoted to managing patients exposed to radiation. Although we cared for the injured and ill patients who had been exposed to the radiation emitted from the explosion in Reactor No. 3, the exposed dose was fortunately small, and we could smoothly conduct routine intensive care management by providing reeducation on secondary radiation exposure to staff. While the number of injured and ill patients exposed to radiation was small and we could manage them without panic, the staff had considerable anxiety during the several months after the disaster, when the nuclear reactors were still unstable. Thus, simulations were performed to prepare for the possible occurrence of a large number of injured and ill patients exposed to radiation (Fig. 4). Staff anxiety was gradually alleviated as they learned more about radiation exposure through the hospital-wide education programs.

Transition of the Ambient dose around Fukushima Medical University
The explosion in Reactor No. 3 at the Fukushima Daiichi Nuclear Power Plant resulted in an increase in environmental radioactive substance concentration—that is, the ambient dose—in the area surrounding our hospital.

Ambient dose of each ward
The main concerns were pollution of the mechanical ventilators that compressed air from the external environment, which would in turn pollute the ICU department. However, the ambient doses in both ICU were approximately one tenth of that outside the building. Those doses were almost the same as the doses of a ward where artificial respiration is not performed.

Radiation survey at air conditioning room and air filter
Radiation survey showed that many of the radioactive substances had been captured in the air conditioner filters.
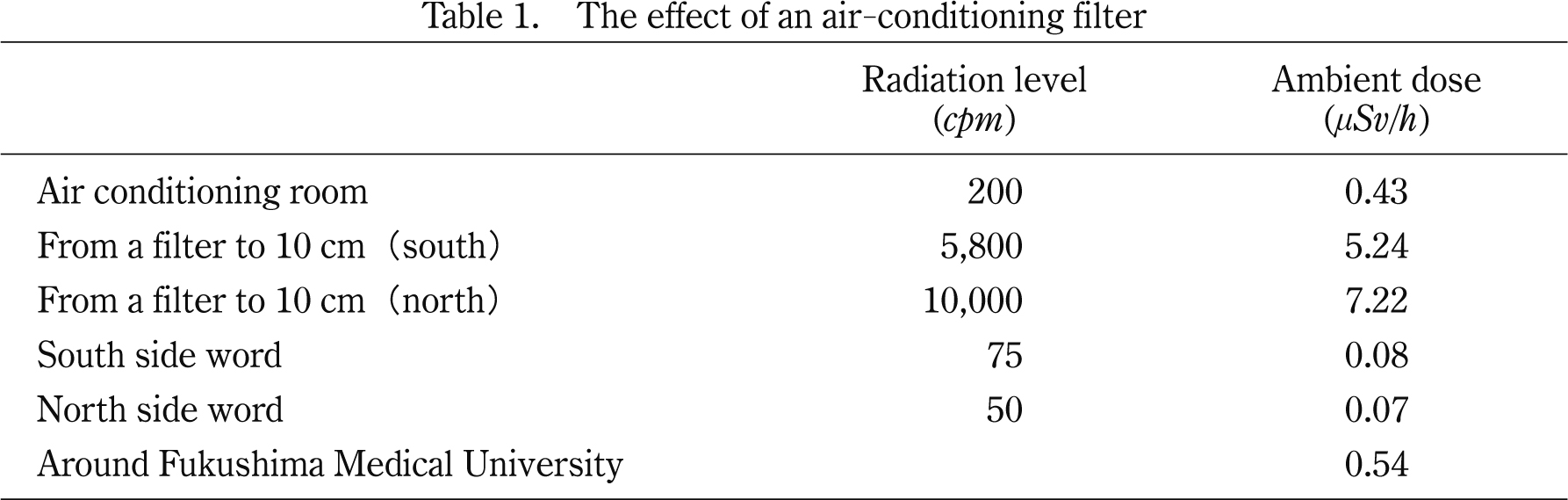
The effect of an air-conditioning filter
Air conditioning room had clearly high radiation level and rich ambient dose compared with general word. Especially, the high dose was measured around air conditioner filters.

Illustration shows the overview of training that assumes a large number exposure victim correspondence. Training took place on the assumption that many exposure pollution victims were transported to our athletic field by the Self-Defense Forces helicopter. The blue line is patient transport line to the pre-decontamination triage area (photo below right). Red, yellow, green line shows the flow line of the patient after pre-contamination triage. Mild (Self-decontamination possible) and moderate patient (Self-decontamination impossible but vital signs stable) was transported to the treatment area after passing the decontamination area (portion enveloped with green and yellow dotted line). On the other hand, critically ill patients were treated with the decontamination at the same time. More than 100 staff members participated in this training.
On the basis of these experiences, we try to discuss about role of ICUs during disasters.
During disasters, the ICU department is required to provide medical care to severely ill patients, which is no different from usual. However, the balance of supply and demand of medical resources is far different from usual. Countless injured and sick people need care in response to area-wide disasters such as earthquakes and tsunami, as well as more localized incidents such as bus accidents and terrorist attacks. Under such circumstances, the demand for ICUs will dramatically increase. Meanwhile, the ability of ICUs to supply care may be substantially reduced due to many restrictions. Particularity in wide-area disasters, an enormous supply-and-demand imbalance can be caused by shortage of medical equipment and materials due to lifeline failure and distribution system suspension, along with a decrease in human medical resources because the medical professionals themselves are affected by the disaster. Therefore, ICU departments must determine what can and cannot be done when a disaster occurs. Immediately after a disaster, it is necessary to determine whether the hospital can continue to provide medical care, whether it can accommodate large numbers of injured and sick people, and whether severely ill patients can be accepted from other hospitals. Important to these questions are the establishment of a reporting line, securing the safety of the institution and those within, and collecting and analyzing relevant information. All of these principles of action and systematic priority responses are essential parts of the disaster response course of the Major Incident Medical Management and Support (MIMMS)9) system in the United Kingdom. This system is based on the principles of “CSCATTT” that means command and control, safety, communication, assessment, triage, treatment, and transport.
Information lines should be established before a disaster takes place; furthermore, it takes time for the system to become operational during nights and on holidays. Therefore, it is necessary to train the people who will serve as leaders to recognize the role of ICU departments during disasters and give precise instructions. Once these leaders are determined, the next action would be to collect information. It is often impossible to collect sufficient information just by waiting. Information on safety and lifelines should be made priorities; however, when it has been determined that safety has been secured and patients can be admitted, it is necessary to proactively contact the operating room and emergency departments to obtain information, without waiting to be approached for patient admission. The obtained information would then be analyzed and the role of the department reexamined to determine the triage levels of patients who will be accepted and the number of patients requiring intensive care after admission; subsequently, hospital transfers can be coordinated depending on the situation. When there are large numbers of injured and sick patients, it is sometimes impossible to admit all severely ill patients within the area. Under such circumstances, the hospital should be able to coordinate transport to transfer patients to other hospitals, by utilizing the network of ICU departments. In particular, measures must be taken for patients requiring mechanical ventilators, including those receiving home medical care, and it is thought that ICU departments should assume that responsibility. Suspensions in the water supply have enormous impacts on the ability to perform blood purification therapy, which is an important intensive care therapy. In the aftermath of the Great East Japan Earthquake, it became impossible to accept patients on dialysis because of the restricted use of tap water; moreover, securing circuits for filtration dialysis and dialysis solutions were difficult because of a gasoline shortage and a disturbance in the distribution system resulting from the spread of harmful rumors. Because it takes enormous effort to transport severely ill patients requiring intensive care under such circumstances, one might easily imagine that staff in the affected area would have considerable difficulty in managing this by themselves. In the early stage after the earthquake, the Japanese Society of Intensive Care Medicine issued a statement on its website10), and posted a list of hospitals where severely ill patients could be accepted11). However, few intensive care physicians in the affected areas, including the authors, noticed this information. Furthermore, even if we had noticed it, it is obvious that preparing transport methods to those hospitals would have become a great burden in the affected areas. Information transmission is meaningless unless it is effectively utilized. It should be recognized that hospitals must notify staff that there is such a system before a disaster occurs, and moreover, to proactively approach affected areas with suitable transport measures when a disaster occurs.
Fortunately, our hospital suffered no damage from the earthquake or tsunami, and did not require a hospital evacuation. In hospital evacuations along the coastline of Fukushima, hospitals were unable to transport patients with severe respiratory failure, such as those wearing a mechanical ventilator or those in shock requiring extracorporeal circulation. However, if our hospital had required a hospital evacuation, it would have been necessary to transport such severely ill patients. It is expected to be exceedingly difficult to transport severely ill patients in the turmoil surrounding a major disaster. Although it is no doubt indispensable to presume how best to evacuate hospitals during disasters12), it must be noted that transport measures cannot be created by a single hospital, even if it is a large-scale university hospital like ours. We believe that it requires a national strategy, and urgent measures are necessary. In the case of a tsunami, there is no time to transport severely ill patients. We believe that medical professionals must discuss how to respond under such circumstances and obtain the consensus of citizens, as in the case of issues of organ transplantation and death with dignity.
Many of the medical problems in Fukushima Prefecture in the aftermath of the disaster were attributable to the nuclear accidents. Patients exposed to radiation are highly likely to require treatment in emergency ICU department. Furthermore, many of the medical staff fulfilled their responsibilities while also feeling concerned about themselves and their families being exposed to radiation. Medical institutions treating patients who have been exposed to radiation require not only education on a regular basis along with practical training for staff, but also the establishment of a system ensuring that staff involved in treating radiation-exposed patients retain their mental health13). Moreover, medical care for radiation-exposed patients was often unexpected, and the emergency ICU department was requested to respond to such unexpected circumstances. Because damage conditions vary between disasters, flexible responses, in other words, corresponding in consideration of the priority according to the time phase of disaster, are required in emergency ICUs when they are admitting severely ill patients.
The summary of this paper was reported at the 39th annual Meeting of the Japanese Society of Intensive Care Medicine (2012, Makuhari).
All authors declare no conflict of interest regarding the contents of this article.