2015 年 61 巻 2 号 p. 131-140
2015 年 61 巻 2 号 p. 131-140
Background and Objective: Skull base chordomas are clinically malignant because of the difficulty of total removal, high recurrence rate, and occasional drop metastasis. Although aggressive surgical resection and postoperative radiation have been recommended, the long-term outcome remains unsatisfactory. Methods: From 1992 to 2011, we treated 24 patients with skull base chordoma using aggressive surgical removal as a principal strategy. Skull base approaches were selected according to tumor extension to remove the tumor and surrounding bone as completely as possible. After surgery, all patients were closely observed with MRI to find small and localized recurrent tumors, which were treated with gamma-knife radiosurgery or surgical resection. The mean postoperative follow-up duration was 10.2 years (range, 1-17.2 years). Results: The 5-, 10-, and 15-year overall survival rates were 86%, 72%, and 72%, respectively. The 5- and 10-year progression-free survival rates were 47% and 35%, respectively. Tumor extension to the brainstem and partial tumor removal were the factors related to poor survival. Conclusions: Our results suggest that aggressive surgical removal improves the long-term outcome of patients with skull base chordoma. We would like to emphasize that skull base chordomas should be aggressively removed using various skull base approaches.
Chordoma is a rare tumor, presumably originating from remnants of the primitive notochord. The incidence of chordomas ranges from 0.8 to 5 cases per million individuals per year. Approximately 50% of chordomas develop in the sacrococcygeal region, 35% in the spheno-occipital region, and 15% in the vertebrae. Skull base chordomas arise in and around the upper and middle clivus as well as the spheno-occipital synchondrosis. Although they are considered to be slowly growing low-grade malignancies, their behavior is more aggressive because of infiltration to local bone, extension to adjacent soft tissue, high recurrence rate, and occasional metastasis1).
Clival chordomas are difficult to treat because of their deep location and the invasive nature of the tumor. An aggressive surgical approach to attempt radical resection and subsequent postoperative radiation therapy is recommended as the current therapeutic algorithm1-3). The degree of tumor resection has proved to be an independent factor for tumor recurrence and the strongest determinant of survival1). Long-term follow-up reports have shown that longer survival rates were correlated with more extensive tumor removal2-6).
In our previous study, we demonstrated long-term control of clival chordoma with initial aggressive surgical resection, and gamma knife stereotactic radiosurgery (SRS) for recurrence7). The mean follow-up after surgical resection at that time was 7.3 years. In the present study, we show further long-term outcome with the mean follow-up of 10.2 years and evaluate clinical factors for poor outcome.
From 1992 to 2011, we treated 24 consecutive patients with clival chordoma in Nagoya University Hospital, Fukushima Medical University Hospital, and their affiliated hospitals: 15 men and 9 women, age ranging from 7 to 75 years old (mean, 46) (Table 1). Two patients had recurrent tumor after surgery or multiple surgeries and radiation. Our principal strategy is aggressive surgical resection. We tried total removal of the tumors using various skull base approaches. The surrounding bone was removed or drilled out as completely as possible, and the clival dura was thoroughly cleaned up.
The location and extension of the tumors with surgical approaches are shown in Table 1. Selected approaches were a transsphenoidal approach: microscopic (2 patients) before 1998 and endoscopic (6 patients) thereafter, an anterior craniofacial approach with preserving olfaction (7 patients)8), staged lateral suboccipital and anterior craniofacial approaches (1 patient), an orbitozygomatic or zygomatic approach (2 patients), an anterior or combined petrosal approach (3 patients), 3-staged surgery: right and left transcondylar approaches and anterior approach, either transoral or mandibular swing approach (2 patients), and a combined zygomatic and extended endonasal endoscopic approach (1 patient). If a dural defect had been made by the tumor itself or was made by surgical procedures, it was patched using fascial graft and covered with either a nasoseptal flap or a temporoparietal galeal flap9,10).
After surgery, all patients were closely observed with magnetic resonance imaging (MRI) every 4-6 months. Our secondary strategy is to find recurrent tumors as early as possible, and treat them by surgical resection or SRS. Since the recurrent tumors were usually small and localized after aggressive resection, they could be treated with high-dose radiation (marginal dose ≥ 16 Gy, whenever possible) using SRS. Some tumors that adhered to the brainstem or recurred in the spine were treated with fractionated stereotactic radiotherapy (SRT, Novalis). The mean duration of postoperative follow-up was 10.2 years (range, 1-17.2 years).
Statistical analysis of data was performed using SPSS. Overall survival and progression-free survival (PFS) were calculated using Kaplan-Meier analysis. To detect clinical factors affecting survival, a log-rank test as well as uni- and multivariate analyses using the Cox proportional hazards model were performed. Values of p<0.05 were considered statistically significant.

Clinical factors, tumor location and extension, and selected approach of 24 patients with clival chordomas
Total removal was achieved in 16 patients (67%) and subtotal in 6 (25%). In the remaining 2 patients (8%), the tumor was partially removed because of extension to the cavernous sinus and invasion to the brainstem. Postoperative complications occurred in 11 patients, which were temporary in 5 and permanent in 6 (Table 2). The most frequent complication was abducens nerve palsy, which occurred in 8 patients, temporarily in 4 and permanently in 4. CFS leak in 2 patients was successfully treated with lumbar drainage. Postoperative Karnofsky performance scales for all 24 patients were between 80 and 100.
Three patients received conventional radiation since before 1996 we selected postoperative radiation for remnant tumor immediately after subtotal removal. One patient after partial removal received additional surgery using an anterior craniofacial approach to remove remnant tumor in the cavernous sinus. The other patient who had undergone partial removal received SRT (3 Gy, 14 fractions) for remnant tumor on the brainstem immediately after the initial operation.
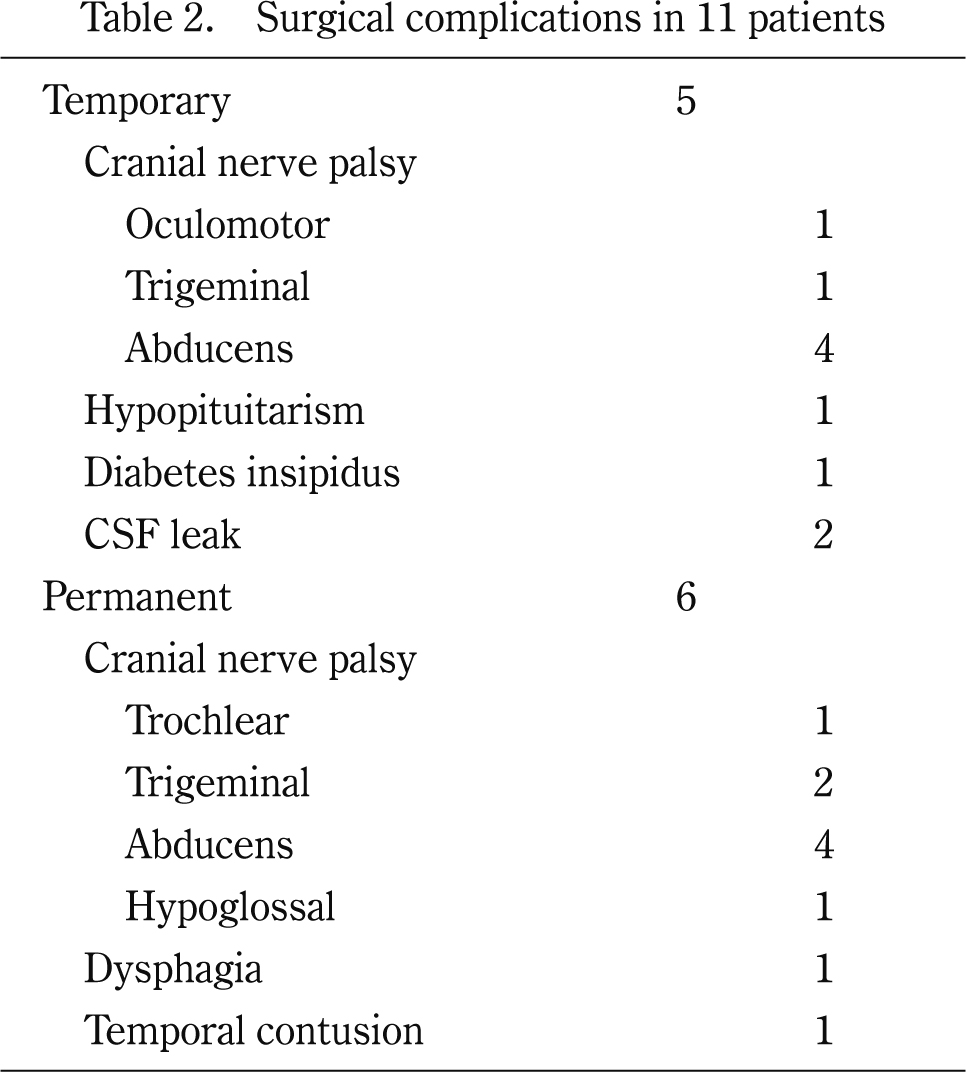
Surgical complications in 11 patients
During follow-up, tumors recurred in 13 patients, between 6 and 74 months (mean, 28) after initial surgery. Three tumors, 1 recurrence at the atlas and 2 drop metastases in the anterior cranial base and on the cerebellum, were surgically removed. The other 10 first recurrent tumors were treated with SRS. Five- and 10-year PFS were 47% and 35%, respectively (Fig. 1a).
Among the 13 patients with tumor recurrence, 9 were alive at the end of the study. Of these, 5 patients including Case 2 had a single recurrent tumor (treated by SRS in 4 and surgery in 1) and 4 had multiple recurrences. One of these 4 patients (Case 3) had 7 recurrent tumors in different locations of the clivus and paranasal sinuses, all treated by SRS. Taken together, a total of 22 recurrent tumors in 9 alive patients were treated by SRS. Three tumors recurred and the other 19 tumors were controlled during follow-up of 3 to 169 months (mean, 69 months).
SurvivalAmong the 11 patients without tumor recurrence, 2 patients died: 1 died of gastric cancer 10 months after surgery and the other died of surgical complication, infection and carotid artery rupture, 4 months after surgery. Among the 13 patients with tumor recurrence, 4 patients died. One patient died 104 months after initial surgery with dissemination along the tentorium. Another patient died 118 months after initial surgery, with tumor invasion around the carotid artery. Another patient died 45 months after initial surgery with tumor invasion to the brainstem and dissemination. The final patient died 40 months after initial surgery with tumors in the brainstem and drop metastases. The 5-, 10-, and 15-year overall survival rates were 86%, 72%, and 72%, respectively (Fig. 1b).

Kaplan-Meier curves for progression-free survival (a) and overall survival (b) of 24 patients with clival chordoma.
The relationships between the overall survival and clinical factors such as gender, age at the initial treatment, with or without dural defect, with or without intradural extension, with or without extension to the brainstem (adhesion to or invasion in the brainstem), degree of tumor resection, and MIB-1 labeling index were analyzed. Kaplan-Meier log-rank analysis indicated that overall survival was significantly longer in patients who were ≤ 55 years old than those who were >55 at the initial treatment (p=0.034), in those without intradural tumor extension than those with (p=0.044), in those without tumor extension into the brainstem than those with (p=0.001, Fig. 2a), and in those with total or subtotal removal than those with partial removal (p=0.016, Fig. 2b). Univariate analysis revealed correlations between tumor extension to the brainstem or the degree of tumor resection and the overall survival (Table 3). In multivariate analysis, significant relation with the overall survival was found in the tumor extension to the brainstem (p=0.021) but not in the degree of tumor resection (p=0.160).
The relationships between the PFS and clinical factors were analyzed. Kaplan-Meier log-rank analysis indicated that PFS was significantly longer in patients without tumor extension into the brainstem than those with (p=0.019, Fig. 3a), in those with total or subtotal removal than those with partial removal (p=0.015, Fig. 3b), and in those with MIB-1 index of the tumor < 3.44% than those with ≥ 3.44% (p=0.019). Univariate analysis revealed correlations between tumor extension to the brainstem, the degree of tumor resection, or MIB-1 index and the PFS (Table 4). In multivariate analysis, however, correlations between these factors and the PFS were not significant.

Kaplan-Meier curves for overall survival of 24 patients with clival chordoma. a: Survival of patients without tumor extension to the brainstem (n=20) was significantly better than that of patients with such extension (n=4) by log-rank test (p=0.001). b: Survival of patients with total or subtotal tumor removal (n=22) was significantly better than that of patients with partial tumor removal (n=2) by log-rank test (p=0.016).

Correlation between the clinical factors and overall survival based on the univariate analysis of Cox proportional hazards modeling.
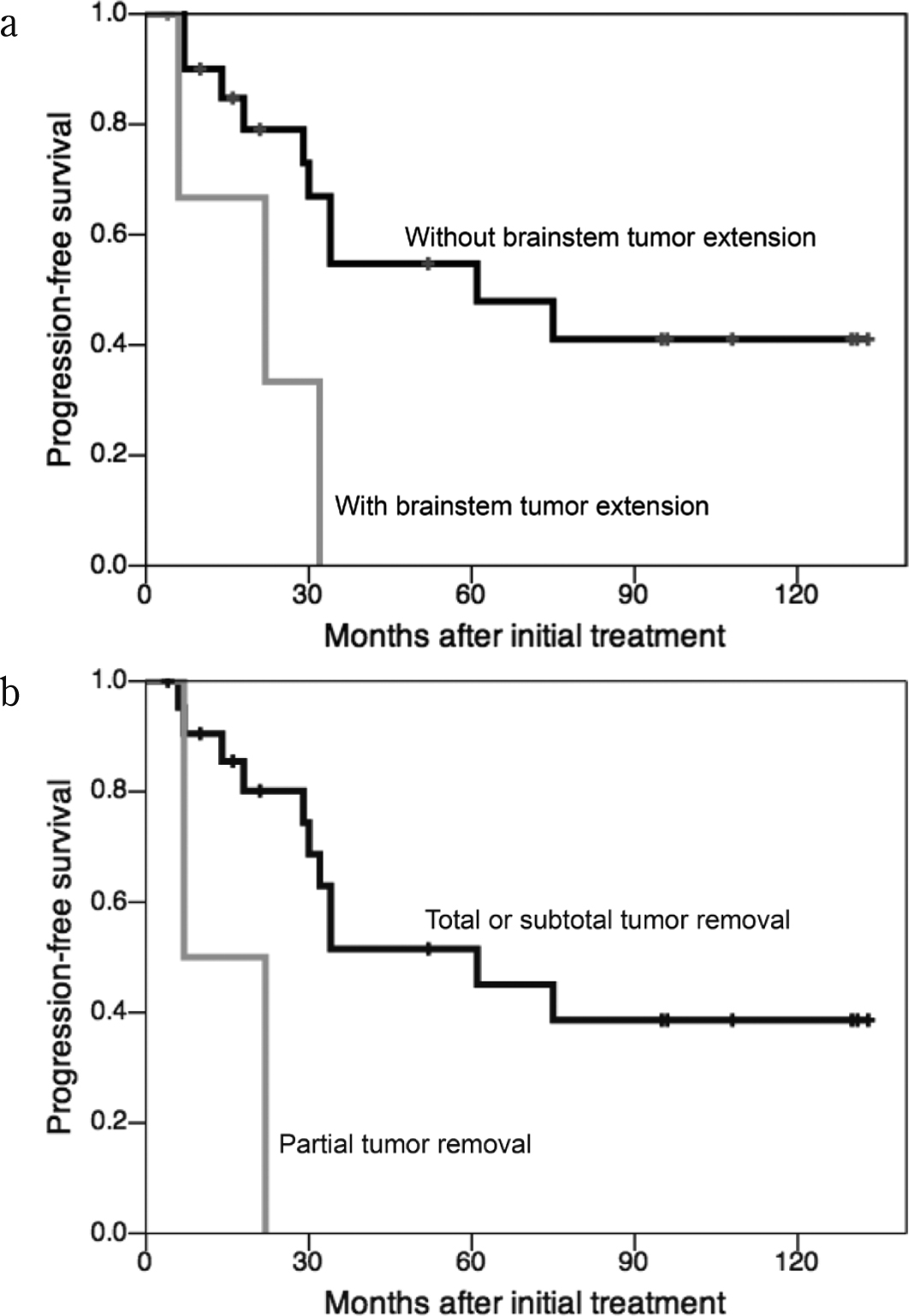
Kaplan-Meier curves for progression-free survival of 24 patients with clival chordoma. a: Progression-free survival of patients without tumor extension to the brainstem (n=20) was significantly better than that of patients with such extension (n=4) by log-rank test (p=0.019). b: Progression-free survival of patients with total or subtotal tumor removal (n=22) was significantly better than that of patients with partial tumor removal (n=2) by log-rank test (p=0.015).
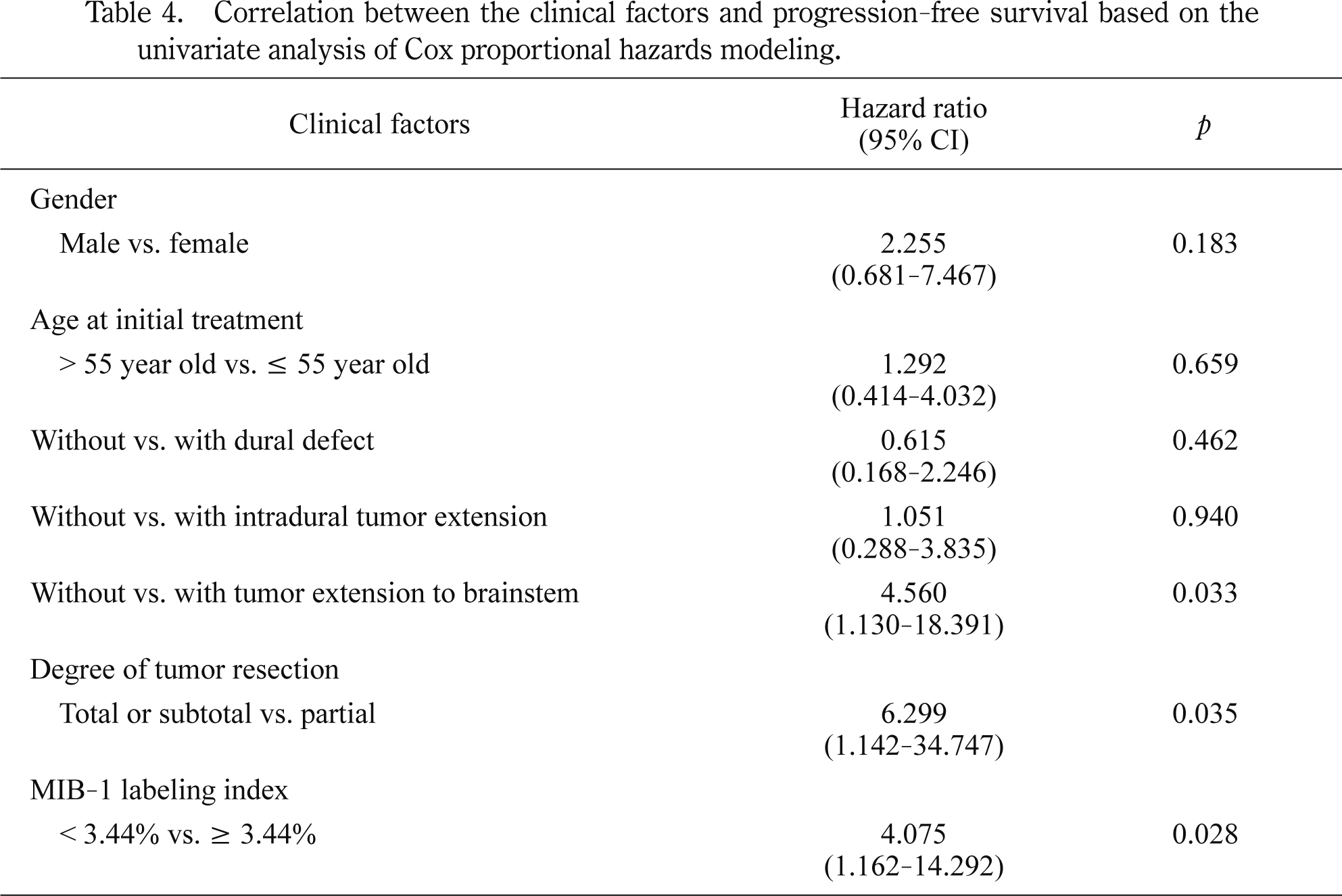
Correlation between the clinical factors and progression-free survival based on the univariate analysis of Cox proportional hazards modeling.
An 18-year-old woman was referred to us with diplopia due to left abducens nerve palsy. MRI revealed a clival tumor extended posteriorly with severe compression of the brainstem (Fig. 4a, b). We selected a right combined petrosal approach. Through a dural defect, the tumor extended into the intradural space without adhesion to or invasion into the brainstem. The tumor was totally removed (Fig. 4c, d). After surgery, the patient suffered from bilateral abducens nerve and left oculomotor nerve palsy. During a follow-up period of 10 years and 10 months, these symptoms were resolved and no recurrence was observed.

Case 1. a, b: Preoperative axial T1-weighted (a) and sagittal enhanced (b) MRI showing a clival tumor extended posteriorly and severely compressing the brainstem. The tumor occupied the right and left Meckel’s caves (arrows). c, d: Postoperative enhanced axial (c) and sagittal (d) MRI showing total removal of the tumor.
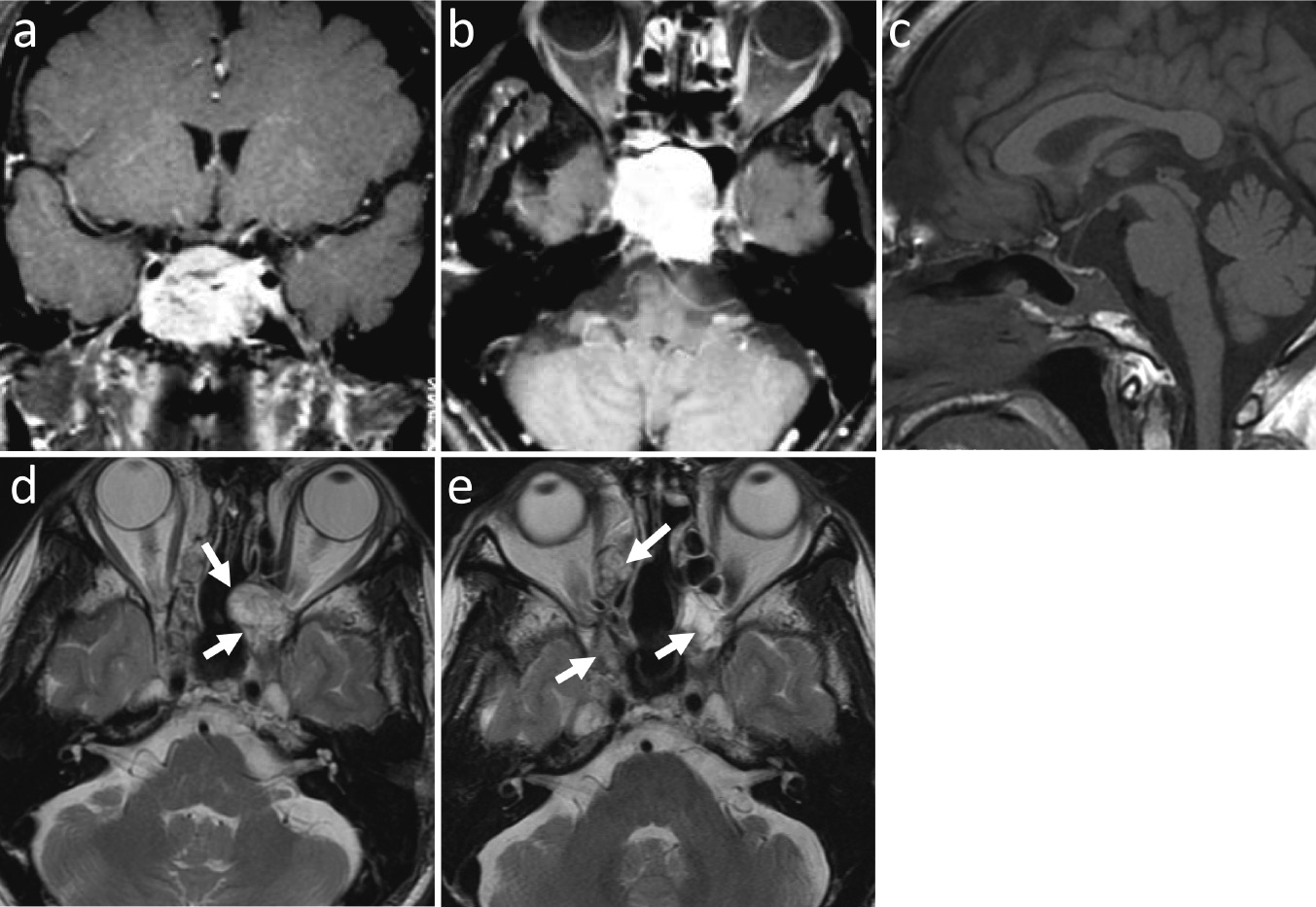
A 25-year-old woman was referred to us with symptoms of left facial dysesthesia and spasm. MRI revealed a clival tumor extended laterally into the cavernous sinus and the petrous bone (Fig. 5 a, b). We selected an orbitozygomatic approach. The tumor was totally removed. The petrous bone was removed to expose the entire petrous carotid artery, eustachian tube and part of the cochlea. The clivus was thoroughly drilled until to reach the normal bone at the remnant lower clivus (Fig. 5c). The skull base defect was reconstructed using a temporoparietal galeal flap. After surgery, the patient temporarily suffered from facial numbness and abducens nerve palsy. Twenty-nine months after surgery, MRI revealed a recurrent tumor in the right side of the posterior clinoid process (Fig. 5d, e), which was treated by SRS. For 10 years and 11 months after the initial surgery, the recurrent tumor was kept under control and no other recurrence was found.
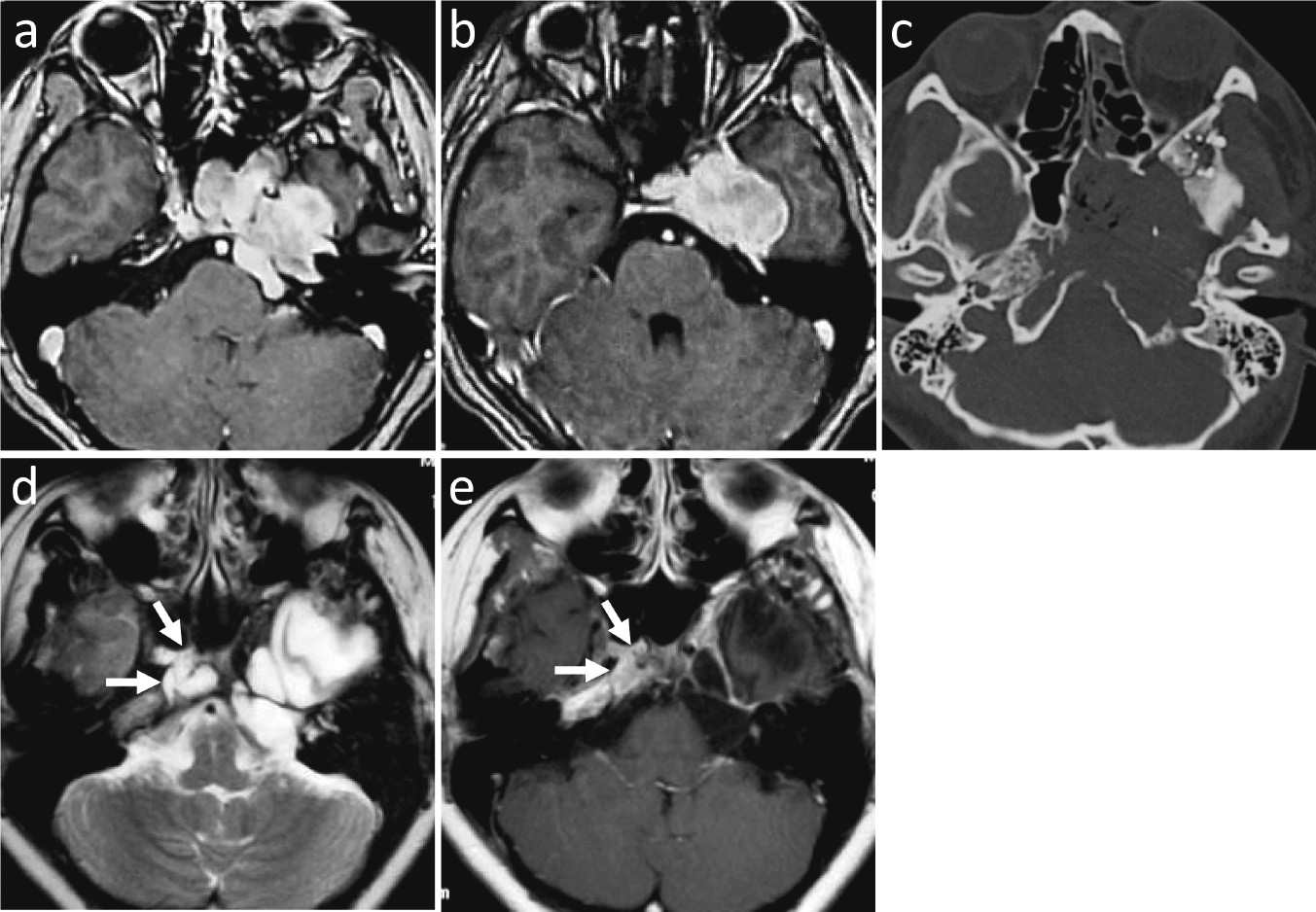
Case 2. a, b: Preoperative enhanced axial MRI showing a clival tumor extending to the left cavernous sinus and petrous bone. c: Postoperative CT showing resected clival and petrous bone. d, e: T2-weighted (d) and enhanced (e) axial MRI 29 months after surgery showing a recurrent tumor at the right posterior clinoid process (arrows).
A 55-year-old man was referred to us with diplopia due to left abducens nerve palsy. MRI revealed a clival tumor extended to the sphenoid sinus (Fig. 6a, b). We selected an anterior craniofacial approach. The tumor was totally removed (Fig. 6c). After surgery, the diplopia improved. Thirteen months after surgery, a recurrence was found in the left cavernous sinus and treated by SRS. Then, almost every year, a new recurrence was found in the ethmoid sinus, cavernous sinus, medial part of the orbit, or cranial base (Fig. 6d). In total, 7 recurrent tumors were treated by SRS and controlled for 7 years and 5 months after the initial surgery (Fig. 6e).
Case 3. a, b: Preoperative enhanced coronal (a) and axial (b) MRI showing a clival tumor extending to the sphenoid sinus. c: Postoperative sagittal T1-weighted MRI showing total removal of the tumor. d: T2-weighted axial MRI 53 months after surgery showing a recurrent tumor (arrows), which was treated by the fourth gamma knife radiosurgery. e: T2-weighted MRI 89 months after surgery showing controlled recurrent tumors (arrows).
Prognosis of chordoma patients remains unsatisfactory with 5-year overall survival rates of around 60-80%11-16). In the USA, the analysis of 400 patients from 1973 to1995 revealed 5- and 10-year relative survival rates of 67.5% and 39.9%, respectively13). In the UK, registry data showed that the 5-year survival rate of patients who were diagnosed between 1998 and 2002 was 56%15). A systematic review of 560 non-duplicated patients demonstrated 5- and 10-year survival rates of 63% and 16%, respectively12). Radical surgical resection has been shown to be a key factor for longer survival2,3,6). Previously, we reported the follow-up results of 19 patients7): all were alive at the end of the study with mean follow-up of 7.3 years. Since some patients died after the publication of that paper, we reviewed the follow-up data again with newly treated patients and longer follow-up outcome. Our mean postoperative follow-up of 10.2 years was significantly long in order to evaluate the long-term outcome. The 5- and 10-year overall survival rates of our patients, 86% and 72%, respectively, proved that aggressive removal of chordomas improves long-term outcome of chordoma.
We selected various skull base approaches and showed that aggressive removal is a fundamental factor for better outcome. Recently, an extended endonasal endoscopic approach has been developed17-19). Koutourousiou M, et al. reported results of the endoscopic endonasal approach on 60 patients with a mean follow-up of 17.8 months18). The limitations for gross total resection, achieved in two thirds of their patients, were tumor volume greater than 20 ml, tumor location in the lower clivus with lateral extension, and previously treated disease. The complications included CSF leak (20%) resulting in meningitis (3.3%), and carotid injuries occurred in 2 patients. Even in endoscopic surgeries, total tumor resection with removal or drilling of the surrounding bone should be performed. Longer follow-up results are necessary to confirm the real benefits of the extended endonasal endoscopic approach.
Besides incomplete surgical resection, clinical factors such as old age, female sex, large tumor size, prior surgery and prior radiotherapy have been associated with poor prognosis20-23). Wu Z, et al. analyzed 79 of 106 consecutive patients with an average follow-up of 63.9 months16). The history of radiotherapy or surgery, dedifferentiated pathology, and insufficient tumor resection were risk factors for long-term survival and recurrence. In our previous paper, we demonstrated that higher MIB-1 labeling index was associated with shorter progression-free survival7). In the data of this paper, tumor adhesion or invasion to the brainstem was a factor of poor long-term outcome.
High dose radiation is another important factor for better control of the chordoma1,3). Proton-beam therapy has been used to deliver high dose radiation to clival chordomas24,25). Data have shown an increase in local control and survival with the use of proton therapy26). Recently, carbon ion radiation therapy has been available27,28). Uhl M, et al. treated 155 patients with 5-year and 10-year local control rates of 72% and 54%, respectively, and 5-year and 10-year overall survival rates of 85% and 75%, respectively29). Fractionated stereotactic radiation therapy is another method for high dose radiation. Jiang B, et al. reported the outcome of 20 chordoma patients with a mean marginal dose of 32.5 Gy (18-50 Gy). The overall survival at 5 years was 52.5%30). Bugoci DM, et al. reported 12 patients who underwent surgical resection followed by high-dose fractionated stereotactic radiotherapy. The overall 5-year survival rate in that study was 76.4%31).
We selected SRS for recurrent tumors32,33) and treated them with high dose radiation since they had been localized and small after total or subtotal removal by initial aggressive surgery. Koga T, et al. showed that sufficient marginal doses of SRS at least 16 Gy appeared crucial34). Kano H, et al. reported results of SRS from the North American Gamma Knife Consortium35). In their paper, the 5-year overall survival rate was 80% for the entire group and 93% for the no prior fractionated radiation group. Marginal dose of ≥ 15 Gy and smaller tumor volume were significantly associated with better tumor control32,35). They concluded that SRS was a potent treatment option for small chordomas, especially in younger patients and as part of multipronged attack that includes surgical resection.
We report long-term outcome (mean follow-up of 10.2 years) of 24 patients with skull base chordoma treated using aggressive surgical removal as a principal strategy. Skull base approaches were selected according to tumor extension to remove the tumor and surrounding bone as completely as possible. The 5-, 10-, and 15-year overall survival rates were 86%, 72%, and 72%, respectively. The 5- and 10-year progression-free survival rates were 47% and 35%, respectively. Our results clearly suggest that aggressive surgical removal improves the long-term outcome of patients with skull base chordoma.
We have no relationship with companies that may have a financial interest.