2017 年 63 巻 2 号 p. 121-125
2017 年 63 巻 2 号 p. 121-125
A 24-year-old man with severe atopic dermatitis underwent anterior cruciate ligament (ACL) reconstruction of the right knee seven years earlier but developed a surgical site infection. The infection did not heal after removal of the metal implants, and a fistula eventually developed. This condition was left untreated for six years before he was referred to our hospital. Magnetic resonance imaging showed fluid in the tibial bone tunnel and extensive bone marrow edema surrounding the bone tunnel. Based on these findings, abscess formation within the tibial bone tunnel and osteomyelitis spreading to the proximal tibia were suspected. During the surgery, a portion of artificial ligament and non-absorbable suture were observed in the bone tunnel, and the infection healed immediately after removal of this complex. When surgical site infection occurs after ACL reconstruction, it is important to completely remove all artificial materials as early as possible.
The incidence of postoperative infection after ACL reconstruction is reported to be 0.4 to 0.9%1,2). Early debridement and complete removal of the artificial implant have been reported to be very important for complete recovery from postoperative infection after ACL reconstruction. A case of prolonged infection at the tibial bone tunnel caused by residual artificial materials after ACL reconstruction is reported.
A 24-year-old man, who had poorly managed severe atopic dermatitis, underwent double-bundle ACL reconstruction of his right knee with hybrid grafts using autologous hamstrings tendon and artificial ligaments at the age of 17 years at a local hospital. Endo-button CL® was used to fix the graft at the femoral side, and interference screws and staples were used at the tibial side. After the first surgery, severe knee pain and swelling developed suddenly, and turbid synovial fluid was obtained by joint puncture on postoperative day 17. Postoperative suppurative knee arthritis was suspected, and arthroscopic debridement was performed immediately. After the debridement, the swelling and pain of the right knee joint decreased immediately; however, wound redness and swelling subsequently developed at the right proximal lower leg where the grafts were fixed by staples and interference screws. Surgical site infection was suspected, and wound debridement with staple removal was performed 10 weeks after surgery, but the interference screws were not removed at that time. Staphylococcus aureus was isolated on wound culture and treated with antibiotics after the surgery. However, the wound did not heal, and a fistula eventually formed. One year after the primary surgery, second wound debridement with interference screw removal was performed, but wound infection was prolonged, and a fistula formed again. The condition was left untreated for six years, and the patient was referred to our hospital at his family’s request. At the initial visit to our hospital, a purulent discharge was observed from the fistula at the right proximal lower leg (Figure 1). There were no inflammatory signs at the knee joint, and range of motion was unrestricted. There was no instability, and he did not feel any knee pain or giving way. Laboratory data showed mild elevation of C-reactive protein (CRP) at 0.32 mg/dL (<0.3 mg/dL). On imaging, partially discontinuous osteosclerosis of the tibial bone tunnel wall was observed, but no obvious evidence of osteolytic change was observed on plain radiographs (Figure 2). On magnetic resonance imaging (MRI), iso-intensity to the muscle on T1-weighted imaging (WI) and high intensity on T2WI were observed within the widened tibial bone tunnel, and linear-shaped low intensity areas on both T1 and T2WI were found within this area. In addition, low intensity on T1WI and high intensity on T2WI with fat-suppression were observed over an extensive area in the bone marrow at the proximal tibia surrounding the bone tunnel, but there was no area of low intensity on T2WI within the bone marrow (Figure 3). These imaging findings indicated abscess formation with necrotic tissue within the tibial bone tunnel and widespread inflammation at the proximal tibia. For this reason, surgery was planned as follows: first, debridement of the tibial bone tunnel where abscess and necrotic tissue were definitively present;and second, additional extensive debridement approaching from the bone tunnel to the proximal tibia as appropriate if intraoperative findings showed spread of infection beyond the bone tunnel to the proximal tibia. Prior to the surgery, the patient was admitted to our hospital for two weeks to treat his atopic dermatitis and improve his skin condition. During the surgery, a fistula was found connected to the tibial bone tunnel, and pus was observed within the bone tunnel. When debridement was advanced further, a portion of the artificial ligament and non-absorbable suture were extracted along with the pus from the bone tunnel (Figure 4). Further observation of the bone tunnel with an endoscope showed osteosclerosis of the bone tunnel wall without destruction, and no obvious communication to the surrounding bone marrow was observed. Moreover, no obvious communication between the bone tunnel and joint was also observed, which indicated that the reconstructed ligament was conserved in the joint. Bone cement mixed with vancomycin was formed into a rod shape and loaded into the bone tunnel. Skin and subcutaneous tissue around the fistula were excised, while still allowing for primary closure. The patient was treated with an antibiotic (cefazolin 6 g/day) intravenously. Since Staphylococcus aureus was isolated from intraoperative tissue culture, cefazolin was administered for two weeks postoperatively, and then levofloxacin was administered orally for three months. Signs of infection were not observed at the surgical site, and healing of the surgical site was achieved on postoperative day 7. CRP also rapidly returned to normal levels on postoperative day 14. The bone cement was removed at eight weeks postoperatively. On MRI, the extensive bone marrow edema at the proximal tibia had disappeared (Figure 5) at three months after surgery. One year after the surgery, there were no signs of infection at the surgical site and the knee joint. There was no instability, and the patient had no subjective symptoms such as pain or “giving way”. He had no limitations in activities of daily living and returned to normal activities.

Purulent discharge is observed from the fistula, and uncontrolled atopic dermatitis is also observed at the right proximal lower leg.

On plain radiographs of the right knee (A, anteroposterior view; B, lateral view), partially discontinuous osteosclerosis of the tibial bone tunnel wall is observed, with no obvious evidence of osteolytic change.
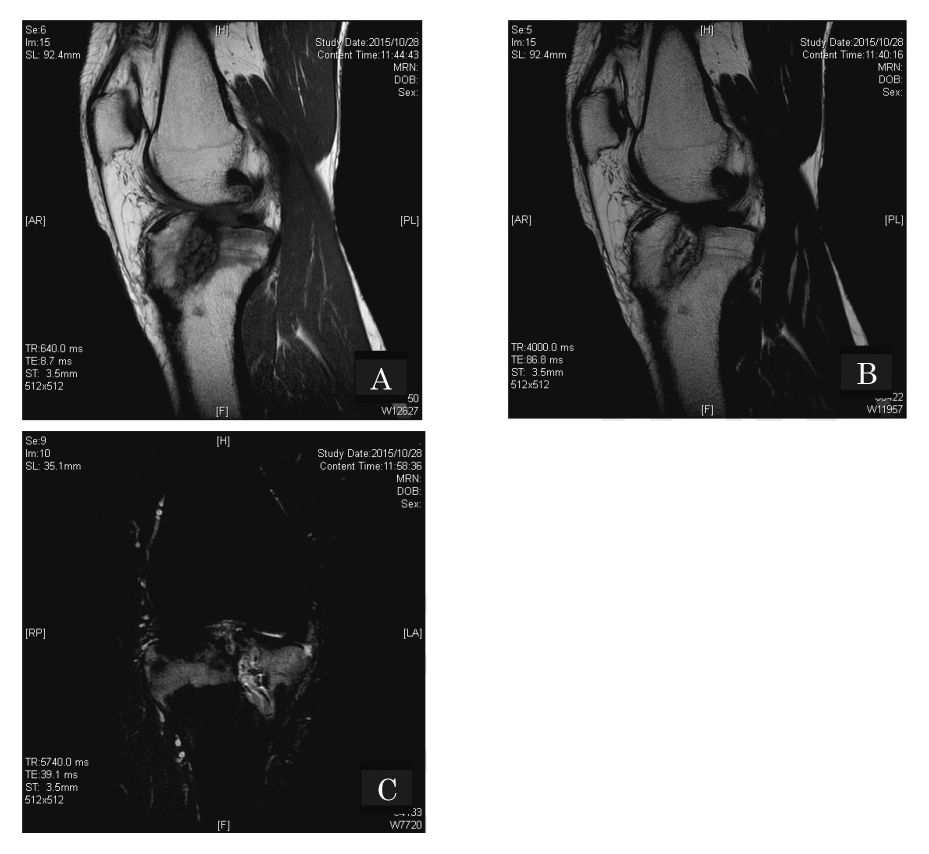
MRI of the right knee. Iso-intensity to the muscle on T1-weighted imaging (WI) (A, sagittal view) and high intensity on T2WI (B, sagittal view) are observed within the widened tibial bone tunnel, and linear-shaped low intensity areas on both T1 and T2WI are found within this area. In addition, low intensity on T1WI (A, sagittal view) and high intensity on T2WI with fat-suppression (C, coronal view) are observed over an extensive area in the bone marrow at the proximal tibia surrounding the bone tunnel, but there is no area of low intensity on T2WI within the bone marrow.

A portion of the artificial ligament and non-absorbable suture were extracted along with pus from the bone tunnel.

The extensive bone marrow edema at the proximal tibia surrounding the bone tunnel has disappeared on MRI performed three months after surgery (A, T1WI, sagittal view; B, T2WI with fat-suppression, coronal view).
Although the development of osteomyelitis after ACL reconstruction is extremely rare, it sometimes induces severe knee dysfunction3-7).
This case is an extremely miserable case of prolonged infection after ACL reconstruction with a fistula untreated for six years despite complete removal of the metal implant and debridement of necrotic tissue. From an intraoperative perspective, the main cause of persistent infection might be the remaining artificial ligament and non-absorbable suture in the bone tunnel. The clinical course of this case indicated that complete removal of artificial implants, not only the metal implant, but also the artificial ligament and non-absorbable sutures, is required to prevent persistent infection after ACL reconstruction.
If an infection spreads to an extensive area around the knee joint, reconstruction of knee joint function becomes extremely difficult. Frank et al. reported a case of osteomyelitis at the distal femur after ACL reconstruction, and knee reconstruction with a modular hinged endoprosthesis was ultimately required4).
In this case, fortunately, the infection immediately and completely subsided with debridement only within the tibial bone tunnel and antibiotic treatment, whereas high-intensity change on T2WI with fat suppression had spread extensively to the proximal tibia around the bone tunnel, which indicated the possibility of extensive osteomyelitis. In general, bone marrow edema is frequently observed on MRI as a reactive change surrounding the abscess8), and it can improve with sufficient antibiotic treatment because of sufficient blood flow. In this case, since a low-intensity area on T2WI, which indicated bone necrosis, was not observed within the region, infection remained within the bone tunnel. To avoid excessive and unneeded debridement, it is very important to perform detailed assessment of the MRI findings and to strictly map the area that requires surgical debridement.
According to previous reports, even when postoperative infection occurs after ACL reconstruction, the reconstructed ligament can be conserved and a cure can be achieved most of the time by performing appropriate debridement and antibiotic treatment at an early stage1,2). Fortunately, intra-articular inflammation subsided after the first arthroscopic debridement, and the reconstructed ligament was preserved in this case. The reason for this is likely that the connection between the bone tunnel and intra-articular space might have been completely blocked after the arthroscopic debridement. However, since prolonged infection at the tibial bone tunnel might be considered to be associated with an extreme risk of spread of infection to the joint, it might be important to perform intensive debridement not only intra-articularly, but also in the bone tunnel as soon as possible when a postoperative wound infection develops after ACL reconstruction.
Since atopic dermatitis is considered to be one of the risk factors for postoperative infection following ACL reconstruction9), it is important to control the skin condition before surgery.
In the present case, the patient was admitted to the Dermatology Department to undergo treatment for two weeks before surgery to control the atopic dermatitis. We should give adequate consideration to the patient’s skin condition before surgery to avoid surgical site infection.
If surgical site infection develops after ACL reconstruction, it is important to remove all of the implants, including artificial ligaments, as early as possible.
The authors declare that there are no conflicts of interest regarding the publication of this paper.