2022 年 68 巻 2 号 p. 135-141
2022 年 68 巻 2 号 p. 135-141
Lumbar spinal canal stenosis (LSS) is a common spinal disorder among older people. Some LSS patients say that their pain worsens when they lift heavy objects. The Valsalva maneuver is the optimal breathing pattern for producing maximal force. Herein, we present two cases of LSS where the movement of the cauda equina was observed during the Valsalva maneuver.
Case Summary:
Case 1: A 74-year-old female with a history of LSS presented to our Department of Urology with frequent urination. The patient was diagnosed as having uterine and bladder prolapse. Pelvic cine MRI scan was conducted for detailed evaluation. While the Valsalva maneuver was performed to diagnose pelvic organ prolapses, we observed movement of the cauda equina. Spine MRI and CT, performed one year before presentation, showed severe LSS due to degenerative spondylolisthesis.
Case 2: A 73-year-old male underwent radical prostatectomy for prostate cancer. A follow-up cine MRI to confirm urethrorrhea showed the cauda equina moving during the Valsalva maneuver. Moderate LSS due to degenerative spondylolisthesis was retrospectively found on abdominal CT performed before prostatectomy.
Conclusion: The findings of our report suggest that movement of the cauda equina during the Valsalva maneuver may be implicated in LSS.
Lumbar spinal canal stenosis (LSS), a common spinal disorder among older adults, causes a variable clinical syndrome of gluteal and/or lower extremity pain, fatigue, and back pain1). The prevalence of LSS is increasing in Japan’s aging society. According to a population-based study among Japanese subjects aged 40 to 79 years, the prevalence of LSS was estimated to be 5.7% using a diagnostic support tool, and the number of patients with LSS was estimated to be 3,650,0002).
A recent systematic review found that symptoms of radiating leg pain, thigh pain, and pain that is exacerbated while standing up showed the highest sensitivity for LSS3). Some LSS patients say that their pain worsens when they lift heavy objects. It is a commonly held belief that the Valsalva maneuver is the optimal breathing pattern for producing maximal force. Intraspinal pressure, which synchronizes with central venous pressure, increases during the Valsalva maneuver4). Thus, intraspinal pressure increasing by the Valsalva maneuver is potentially associated with worsening of pain in LSS patients while lifting heavy objects. However, to date there has been no evidence of a relationship between worsening pain during the Valsalva maneuver and LSS, and the relevant mechanism is also unknown. Herein we present two cases of LSS where movement of the cauda equina was observed during the Valsalva maneuver. To the best of our knowledge, this phenomenon has not been previously reported.
A 74-year-old female with a history of LSS presented to our hospital’s Department of Urology with frequent urination due to bladder prolapse. Physical findings led to a diagnosis of grade 2 uterine prolapse and grade 3 bladder prolapse, based on the Pelvic Organ Prolapse quantification system5). In addition, LSS symptoms of pain in the right buttock and right lower limb were documented by our Department of Orthopedic Surgery.
For more detailed evaluation of pelvic organ prolapse, a pelvic MRI was conducted using a 1.5 T MR scanner (Optima 450w; GE Healthcare, Milwaukee, WI, USA). For cine MRI, an image of the pelvis in the mid-sagittal plane was obtained approximately every 0.42 seconds for 25 seconds using a FIESTA (fast imaging employing steady-state acquisition) cine sequence (repetition time, 4.1 ms; echo time, 1.8 ms; 60 degrees flip angle; slice thickness, 8 mm; field of view, 30 cm; matrix, 200 × 200; and number of signals averaged, 1) while the patient performed Valsalva maneuvers. Other MR sequences, including T2WI and DWI, were the same as those used for ordinary clinical diagnostic purposes.
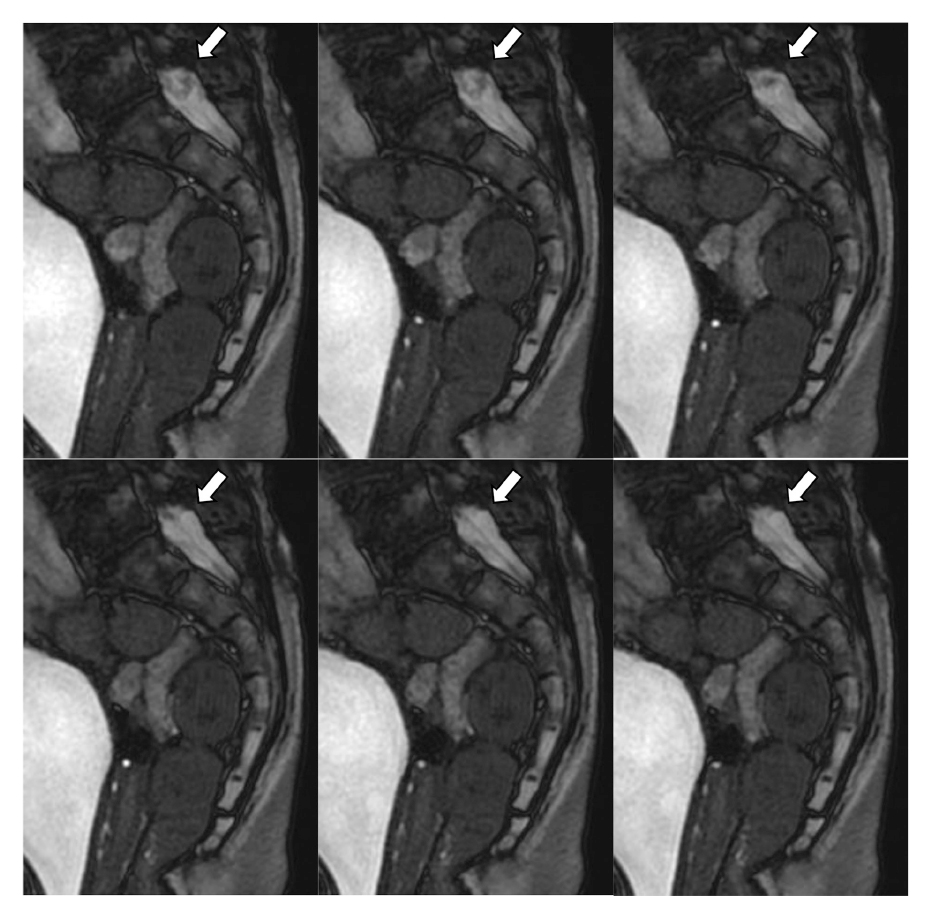
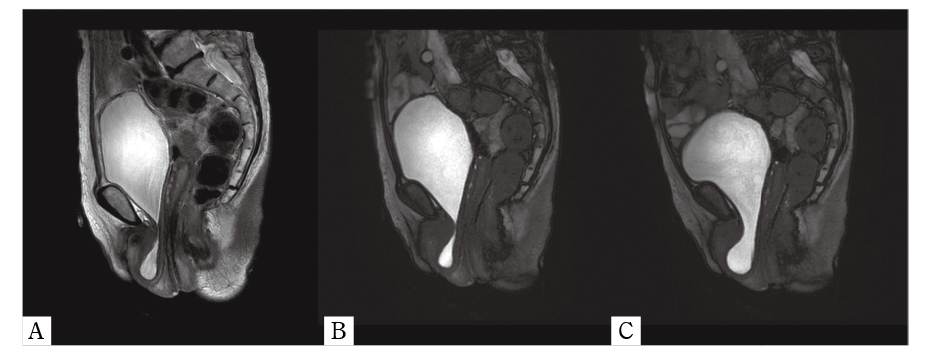
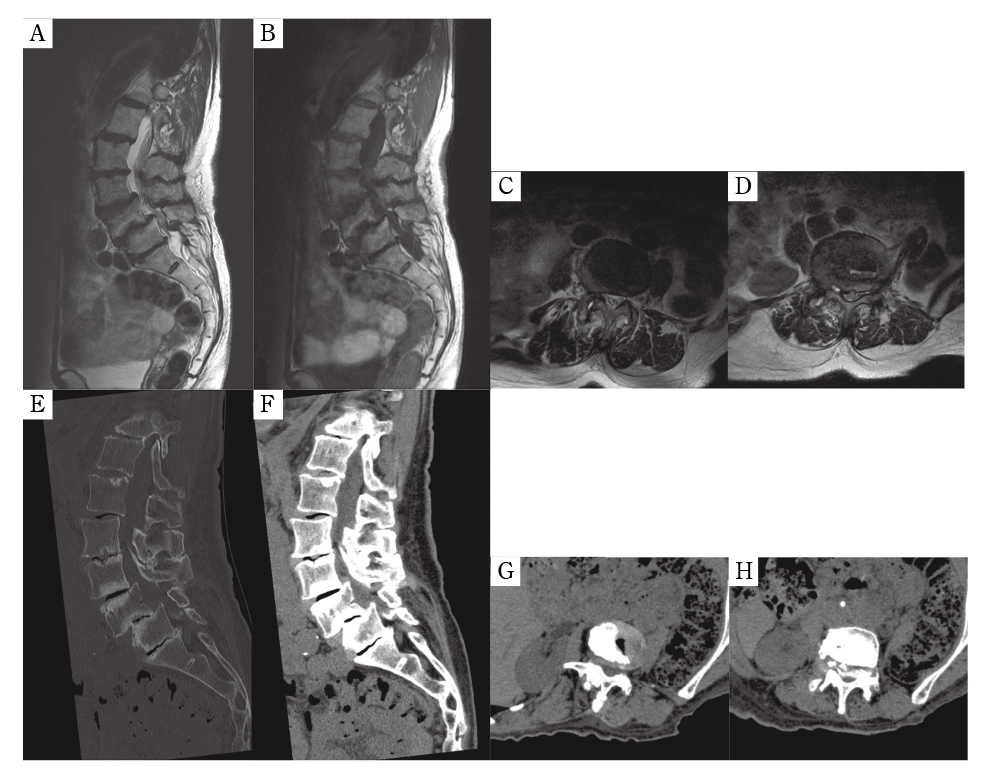
Cine MRI showed the cauda equina moving in an inchworm-like manner when the patient performed the Valsalva maneuver (Figure 1, Supplemental Movie 1). Uterine and bladder prolapses were also found on T2WI (Figure 2A) and cine MRI (Figure 2B, C). Spine MRI (Figure 3A-D) and CT (Figure 3E-H) performed one year before presentation showed severe lumber canal stenosis at L3/4 and L4/5 due to degenerative spondylolisthesis. Grade 2 lumbar spondylolisthesis in the Meyerding classification6) was found at L4/5, while the lumbar spondylolisthesis at L3/4 was grade 1. In the severity criteria of LSS described by Alsaleh et al.7), severe stenosis (spinal canal area reduced by more than two thirds compared to the normal level at the pedicles above) was found at L4/5, and moderate stenosis (a one-to-two thirds reduction in the spinal canal area) was found at L3/4. T2WI also revealed redundant nerve roots (RNRs). The patient has been followed up, and surgical repair for her pelvic organ prolapses is planned.
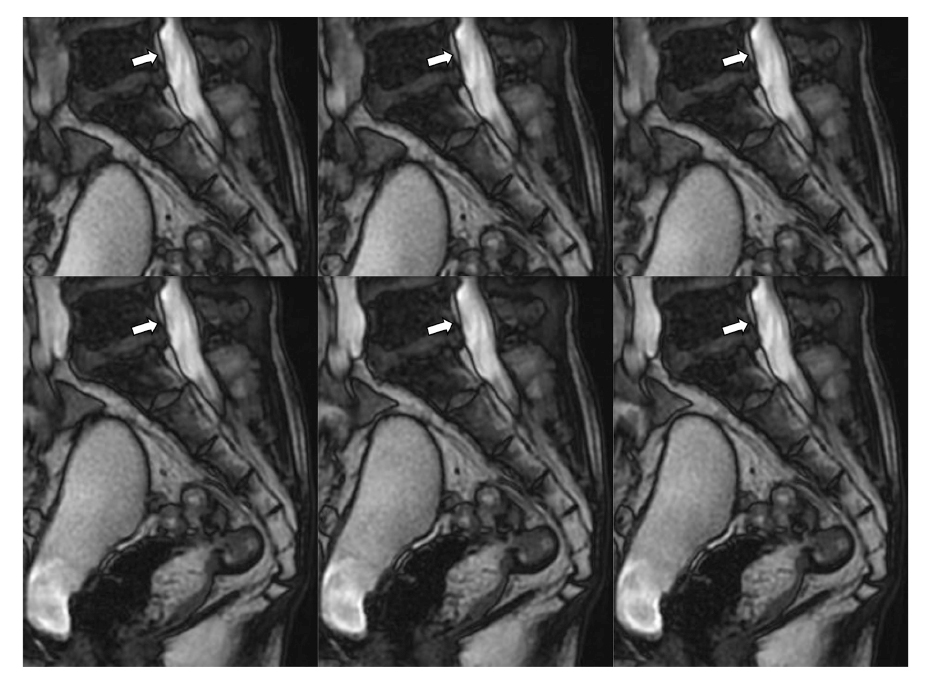
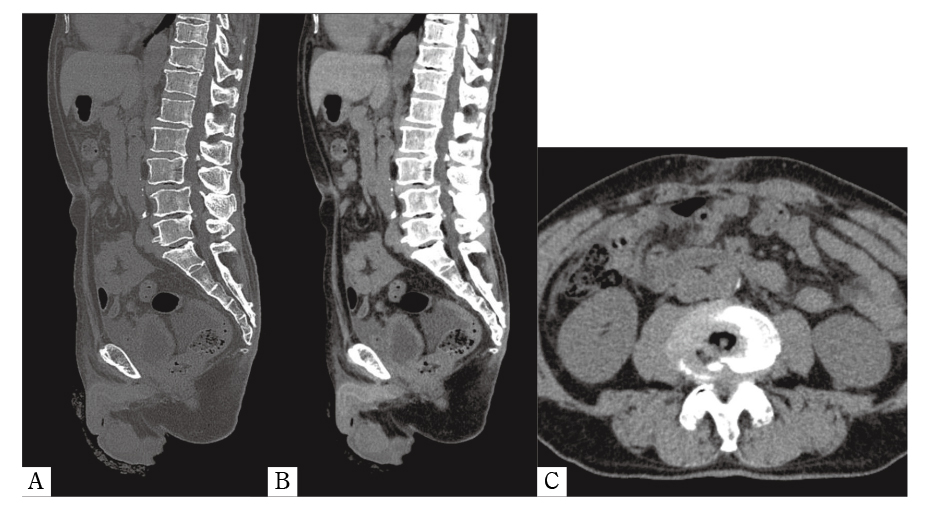
A 73-year-old male with a history of prostate cancer underwent radical prostatectomy and was followed at our hospital. One year after the operation, a follow-up MRI was performed, which included cine MRI for confirmation of urethrorrhea. The cine MRI was conducted according to the same protocol used in Case 1. The cine MRI showed the cauda equina moving in an inchworm manner when the Valsalva maneuver was performed, with movement smaller than observed in Case 1 (Figure 4, Supplemental Movie 2). LSS due to L3/4 degenerative spondylolisthesis was retrospectively found on abdominal CT performed before prostatectomy (Figure 5A-C). Grade 1 lumbar spondylolisthesis in the Meyerding classification and moderate spinal canal stenosis was found at L3/4. The patient is currently being followed and no metastases have been found.
We encountered two cases of spinal canal stenosis where inchworm-like movement of the cauda equina was observed when the patients performed the Valsalva maneuver for breathing. Subsequent searches on PubMed, with cauda equina, moving, and cine MRI as keywords, yielded no positive results. This suggests that we are the first to report movement of the cauda equina during the Valsalva maneuver in LSS patients.
In contrast to the absence of reports such as ours, some cases of spinal canal tumor motion akin to cauda equina motion have been reported. For instance, Moon et al. reported a mobile cauda equina ependymoma moving during a Valsalva maneuver8). In their report, the visualization was made possible by an anesthesiologist initiating a Valsalva maneuver while the patient was under general anesthesia, at which point the tumor was observed to migrate caudally into the operative field. Marin-Sanabria et al. also reported two cases of mobile cauda equina schwannomas9). In their report, the second patient had strained significantly at micturition; thus, they suspected the Valsalva maneuver to be the cause of tumor migration. Taking these reports into account, our cases may share a common mechanism with the aforementioned mobile tumors.
The Valsalva maneuver causes a significant increase in central venous pressure10). The vena cava connects to the vertebral venous system (VVS) by major systemic veins, such as the azygos system11). The VVS is a large, valveless, collateral venous network within and around the vertebral column that extends from the sacral hiatus along the entire length of the vertebral column up to the foramen magnum12). The VVS can be divided into three intercommunicating divisions:the internal vertebral venous plexuses (IVVP), the basivertebral veins, and the external vertebral venous plexuses. The IVVP consist of a network of veins surrounding the dura mater within the spinal canal12). The dura matter is a layer that holds the cerebrospinal fluid (CSF) in and around the brain and spinal cord. Due to a lack of valves in the VVS, central venous pressure may be transmitted directly to the CSF when the Valsalva maneuver is being performed. In an experiment reported by Williams et al. in 1981, they measured venous pressure as well as intracranial and intraspinal CSF pressures simultaneously during the Valsalva maneuver, in conscious patients with sitting posture. In their report, all pressures increased in sync during the Valsalva maneuver4). Thus, a change of CSF pressure due to the Valsalva maneuver may generate CSF flow that moves the cauda equina.
RNRs are defined as elongated, enlarged, and tortuous manifestations of the cauda equina13). Post mortem14) and MRI15) studies reported a relationship between RNRs and LSS. In the present report, RNRs were found in Case 1. Papavero et al. defined the shape of RNRs in their study of MRI morphologies16). According to their study, the serpentines (a sinusoidal deflection of the majority of cauda nerve roots occuring within the height of a vertebral body without any horizontalization of the involved roots) and the loops (in at least two different areas dots or horizontal roots in the sagittal T2WI combined with tortuous, coiled roots in the axial T2WI) were defined as shapes of RNRs. In this regard, the shapes of RNRs, such as sinusoidal deflections and tortuous and coiled shapes, appear to be similar to that of an inchworm.
In LSS patients, the spinal CSF space is separated into the cephalad and caudal areas connected at the narrowed spinal canal. CSF pressures are increased when the Valsalva maneuver is performed. Because of difference in the vascular beds, the cephalad and caudal areas may have different pressures. When a pressure gradient occurs, flow is generated from the high-pressure space to the low-pressure space. It is possible that such flow causes the cauda equina to move. According to the equation of continuity, the flow velocity is inversely proportional to the area of the conduit cross section17). In this regard, the movement of the cauda equina may be related to LSS.
One limitation of this report is that we did not measure CSF flow in the spinal canal. To measure CSF flow in the clinical setting, we propose two methods: one is color Doppler ultrasound during the Valsalva maneuver in a patient undergoing laminectomy, and the other is phase contrast MRI. Another limitation of this report is the lack of data on symptoms during the Valsalva maneuver. Further research is required to evaluate the relationship between LSS symptoms and the movement of the cauda equina during the Valsalva maneuver.
Inchworm-like motion of the cauda equina during the Valsalva maneuver may be related to LSS. Corroborative reports and further research into the frequency of this finding and its relationship to symptoms could advance care for LSS patients.