Abstract
Purpose:We assessed the stiffness of unilateral undescended testes after orchiopexy, examining its value in tracking histopathological changes and fertility potential during postoperative follow-up. Additionally, we explored the optimal timing for surgery based on testicular stiffness.
Patients and Methods:Thirty-six boys who had been diagnosed with unilateral undescended testis and treated with orchiopexy were included in the study. Testicular stiffness was evaluated several times over respective follow-up periods by ultrasound strain elastography after orchiopexy. The strain ratios were measured as the ratios of the elasticities of the descended testis to those of the operated testes. The patients were divided into two groups based on the age at which they underwent orchiopexy:under < 2 years (Group A) and ≥ 2 years (Group B).
Results:The mean strain ratios were 0.90 ± 0.32 and 0.92 ± 0.20 in Groups A and B, respectively. In Group A, the strain ratio was constant regardless of postoperative months (r = 0.01, p = 0.99); however, in Group B, it tended to increase with postoperative months (r = 0.42, p = 0.07).
Conclusions:Evaluation of testicular stiffness may be useful for the estimation of histopathological changes and fertility potential in boys with unilateral undescended testes at follow-up appointments after orchiopexy. Our data indicate that performing orchiopexy as early as possible may be recommended to avoid testicular damage.
Introduction
Cryptorchidism (undescended testis) is one of the most frequent anomalies in boys and leads to a risk of male infertility and a higher incidence of testicular malignancy1). The incidence of azoospermia associated with undescended testis is 13% in unilateral cases and 89% in bilateral cases2). Usually, orchiopexy is the standard treatment in patients with undescended testis. Although historical studies have reported improved fertility when orchiopexy is performed at an earlier age, and while surgical trends in recent years have followed by making diagnoses and performing corrective surgery at younger ages in order to preserve future spermatogenesis3), a definitive conclusion has not been reached concerning the optimal age at which orchiopexy should be performed4-6). This is because a follow-up period of > 20 years may be required to assess fertility and paternity after orchiopexy before a conclusion can be drawn, and such a long-term prospective study would be extremely difficult in a clinical setting.
Although assessment of spermatogenesis before puberty after orchiopexy is also difficult, new evaluation methods are needed to predict histological changes, including spermatogenesis and testicular development, Recently, a noninvasive imaging or numerical evaluation method of tissue stiffness using ultrasound, called ultrasound elastography, has been developed to measure the stiffness of target organs7,8). We hypothesized that this technology could be used to assess testicular development and estimate testicular histopathology in patients who have undergone orchiopexy, since indirect estimation of histological changes is usually made by evaluation of testicular size and volume using ultrasonography and testicular hardness by palpation8). The purpose of this study is to evaluate the testicular stiffness of unilateral undescended testes in patients who had undergone orchiopexy using ultrasound strain elastography, and clarify its usefulness during the follow-up as much as possible. In addition, this paper will discuss strain elastography’s usefulness in the evaluation of testicular stiffness at follow-up appointments after orchiopexy to estimate histopathological findings and fertility potential, and to determine appropriate surgery timing from the viewpoint of testicular stiffness.
Methods
Patients
Thirty-six boys with unilateral undescended testis, for which they had undergone orchiopexy at our hospital, were included in the study. The ages of the patients were recorded at the time of orchiopexy and ultrasonographic examination. The mean age at surgery was 24.5 months (12-127). Thirteen patients had received right orchiopexy and 23 had received left orchiopexy. Patients were excluded if:they had retractile testis and/or other associated malformations; and/or if they were undergoing or had undergone other surgical interventions on their genital organs. Patients with intrabdominal testes and testicular microlithiasis were also excluded. There were no patients with a history of inguinal hernia, epididymorchitis, testicular tumor, previous hormonal treatment, or other inflammation lesions that could affect testicular elasticity. There were no patients approaching the onset of puberty in this study. We performed ultrasound strain elastography multiple times in some patients. Sixteen patients who underwent orchiopexy at age < 2 years were assigned to Group A and 20 patients who underwent orchiopexy at age ≥ 2 years were assigned to Group B. The 36 patients visited our follow-up outpatient clinic between April 2018 and October 2020. The respective median follow-up periods for the groups were 67.2 (9-122) and 20.2 (1-79) months. The ethics committee of Fukushima Medical University Hospital approved the study design (approval number:2245), and all parents of the patients provided written informed consent.
Evaluation of testicular stiffness by ultrasound strain elastography
Testicular stiffness was evaluated using an ultrasound device (HITACHI ARIETTA 70, Hitachi Healthcare Co., Chiba, Japan) with a 9-4MHz linear probe on which real-time tissue elastography software had been installed, enabling the device to visualize intravital distortion caused by pressure (strain elastography). Ultrasonography and strain elastography were performed with the patients lying in the supine position. Elastography was performed by applying slight compression to the testis with the ultrasound probe (Figure 1a). An ultrasound probe was placed in the middle of the scrotum on the affected testis, on which orchiopexy had been performed (operated testis), as well as the contralateral descended testis, and both testes were visualized in the same field of view in the ultrasound image (Figure 1b). The diameter of the region of interest (ROI) was taken as the center of each testis. The strain ratios were measured as the ratios of the elasticities of the descended testis to those of the operated testis (descended testis/operated testis). The strain ratio was calculated between each point of each testis. If the strain ratio was over 1.0, the stiffness of the operated testis was higher than that of the contralateral descended testis. The testicular long diameters of both testes were also measured by ultrasound. One urologist performed all scans to reduce the bias involved in this operator-dependent imaging technique. The strain ratio was automatically calculated by the ultrasound device.

Fig. 1.
Ultrasound strain elastosonographic image of a 6-year-old boy with undescended testis who had received orchiopexy 60 months previously. (a) Ultrasound strain elastography was performed with the patient lying in the supine position. The elastography was performed by applying slight compression to the testis with the ultrasound probe. An echo probe was placed in the middle of the scrotum on the operated testis and the contralateral descended testis. (b) Both testes were visualized in the same field of view in the ultrasound image. The diameter of the ROI was taken as the center of each testis (dotted circle).
All data were analyzed using SPSS statistical package version 29.0 (SPSS Inc., Chicago, IL, USA). The strain ratio and testicular long diameters were compared between the groups using the Mann-Whitney U test. The correlation between the strain ratio and postoperative months in each group was evaluated using the Spearman correlation test. Statistical significance was considered when p < 0.05.
Results
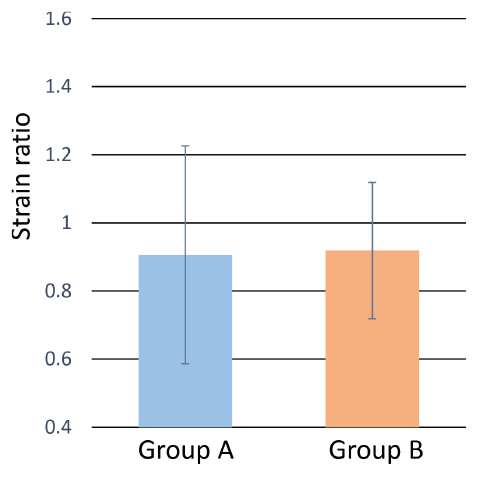
We compared the strain ratio between Groups A and B. In the Group A patients, who underwent surgery at age < 2 years, the mean strain ratio was 0.90 ± 0.32, and in the Group B patients, who underwent surgery at age ≥ 2 years, the ratio was 0.92 ± 0.20. There was no statistically significant difference in the strain ratio between the two groups (p = 0.89) (Figure 2).
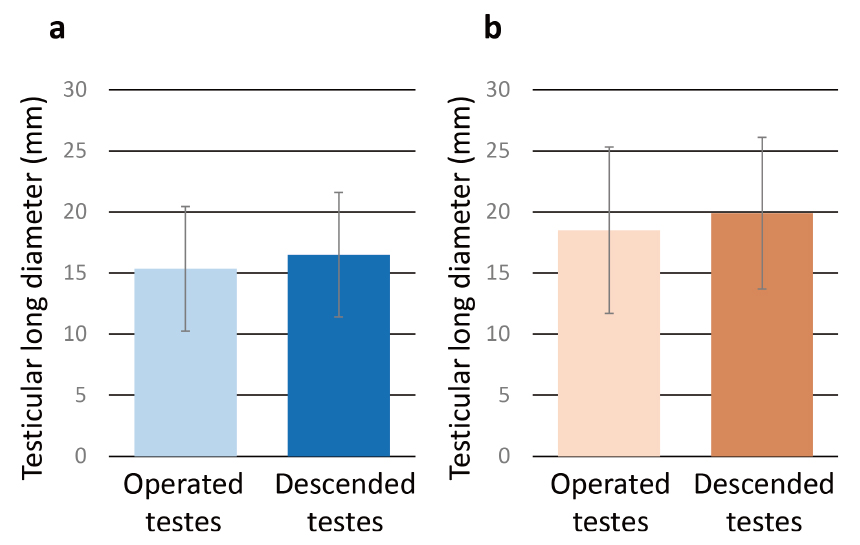
Next, we compared testicular long diameters between the two groups. The testicular long diameter was 15.4 ± 5.1 mm on the operated testis and 16.5 ± 5.1 mm on the contralateral descended testis in Group A. In Group B, the diameter was 18.5 ± 6.8 mm on the operated testes and 19.9 ± 6.2 mm on the contralateral descended testes. The testicular long diameter tended to be smaller in the operated testis than in the contralateral descended testis in both groups, although significant differences were not found. (Groups A and B:p = 0.53, and p = 0.46, respectively; Figure 3). There was also no significant difference in the testicular long diameters of both the operated and contralateral descended testis between the two groups (p = 0.12 and 0.08, respectively). No structural abnormalities, such as microcalcifications or parenchymal gaps, on the parenchyma of both testes were observed by conventional ultrasonography in any patient.
We examined the correlation between the strain ratio and postoperative months in Groups A and B. In Group A, there was no significant correlation between the strain ratio and postoperative months (r = 0.01, p = 0.99), suggesting that testicular stiffness was constant regardless of postoperative months (Figure 4a). In Group B, although no significant correlation was found between the strain ratio and post-operated month (r = 0.42, p = 0.07), the strain ratio tended to increase with the postoperative month (Figure 4b). As shown in Figure 4b, variations in the strain ratio were observed in Group B. In other words, some boys had high strain ratios, while others did not, indicating that the testicular stiffness of the operated testis differed among the patients.
We also examined the correlation between the testicular long diameter and post-operated months in Groups A and B. In both groups, there was a significant positive correlation between the testicular long diameter of operated testis and postoperative months (Groups A and B:r = 0.72, p < 0.01 and r = 0.75, p < 0.01, respectively; Figures 5a and 5b), suggesting that testicular long diameter increased over time. Similarly, a significant positive correlation between the testicular long diameter of the descended testis and postoperative months was found in both groups (r = 0.69, p < 0.01 and r = 0.76, p < 0.01, respectively; Figures 5c and 5d).
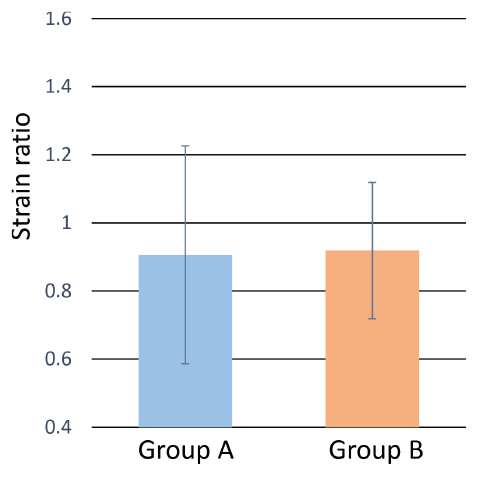
Fig. 2.
Strain ratio in Group A, in whom surgery was performed at age < 2 years, and Group B, in whom surgery was performed at age ≥ 2 years.
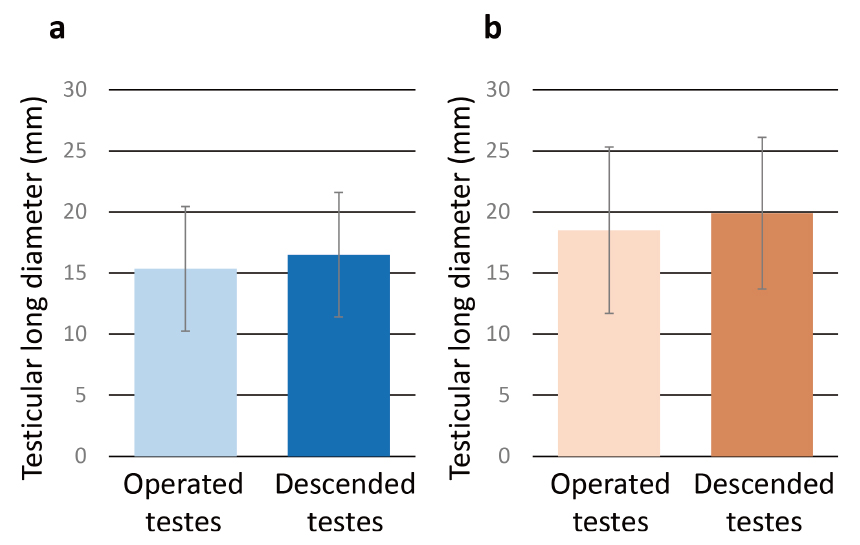
Fig. 3.
Testicular long diameter of operated testes and contralateral descended testes in Group A (a), and Group B (b).

Fig. 4.
Correlation between the strain ratio and post-operated months in Groups A (a) and B (b).

Fig. 5.
Correlation between the testicular long diameter of operated testes (a,b) or descended testes (c,d) and post-operated months in Groups A (a,c) and B (b,d).
Discussion
In the present study, we measured testicular stiffness using ultrasound strain elastography to examine whether we can estimate testicular development and histopathological changes after orchiopexy, and discuss the optimal timing of orchiopexy.
Significant histopathological changes in some patients with undescended testis have been observed, which led to disturbances of spermatogenesis and male infertility in the future9). Several studies demonstrated testicular fibrosis in adults with a history of cryptorchidism10). There are a limited number of tools available to evaluate these histopathologic changes in testes after orchiopexy. Although testicular biopsy can be used to assess histopathological changes such as fibrosis, it is not recommended in the follow-up period because of its invasiveness. Measurement of testicular volume and size by ultrasonography is a noninvasive method to evaluate testicular development. In the present study, a significant positive correlation between the testicular long diameter of both operated testis and postoperative months was found regardless of the timing of orchiopexy. However, testicular volume and size may not always reflect testicular histopathological change. Therefore, a non-invasive procedure to estimate testicular histopathological change is needed.
Ultrasound elastography is a relatively modern evolutionary technique of sonographic imaging. Originally, it was developed to assess tissue stiffness with the potential of differentiating between benign and malignant tumors11). Complementary to conventional ultrasonography, elastography can be used to assess quantitative and qualitative information about tissue stiffness12) and estimate the degree of fibrosis as a result of tissue damage in various organs, including the liver, kidney, and thyroid11,13-16). Therefore, elastography is expected to be used to predict pathological status without tissue biopsy. In the present study, we measured the testicular stiffness of undescended testes after orchiopexy using ultrasound strain elastography.
There are two main methods of measuring stiffness in ultrasound systems:shear wave elastography (also known as transient elastography; SWE), which is a quantitative evaluation using the propagation velocity of shear waves, and strain elastography (also known as static or compression elastography), which is a relative evaluation that visualizes differences in tissue distortion7). Some reports have evaluated testicular stiffness in patients with undescended testes8,17-22), most of which utilized SWE. However, SWE does not take into account individual differences in testicular stiffness because it is used for quantitative evaluations of individual testes. In the present study, therefore, we used strain elastography to evaluate testicular stiffness. Previous reports of testicular stiffness by strain elastography showed that the strain ratios were measured as the ratios of the elasticities of subcutaneous fat tissue to the elasticities of the undescended testes8). In the present study, we measured the strain ratios as the ratios of the elasticities of contralateral descended testes to the elasticities of the operated testes, because they can be visualized in the same field of view by strain elastography simultaneously, and the relative testicular stiffness can be evaluated by causing bilateral testicular tissue distortion with an echo probe. We considered that strain elastography could directly compare the difference in testicular stiffness between the operated testis and the contralateral descended testis, reduce individual differences, and make a more accurate evaluation of postoperative changes occurring in the operated testis.
There are some reports that have investigated the testicular stiffness of undescended testes using SWE17-21). Shin et al. evaluated the differences and changes in testicular volume and elasticity in the normal and undescended testes of children using SWE and reported that instead of increasing volume and decreasing stiffness of normal testes during development in the first 60 months of age, undescended testes had smaller volume and increased stiffness when compared to normal testes. The contralateral descended testes of patients with unilateral undescended testes showed increased volume without stiffness change17).
In the present study, the mean strain ratios were 0.90 ± 0.32 and 0.92 ± 0.20 in the patients who received orchiopexy at age < 2 years and ≥ 2 years, respectively, suggesting that testicular stiffness was similar between the operated and contralateral descended testes. However, the strain ratio remained constant with postoperative months in the patients who received orchiopexy at age ≤ 2 years, while it tended to increase with postoperative months in boys who had received orchiopexy at age ≥ 2 years, although a significant change was not found. Interestingly, variations in the strain ratios were observed in patients who had received orchiopexy at age ≥ 2 years. Some patients had a high strain ratio, while others did not, indicating that the testicular stiffness of the operated testis differed from patient to patient. The variation may be due to a mix of cases that were missed by screening despite having clear undescended testes, or mild cases that were not determined to have undescended testes by screening. Patients with a history of undescended testis do not always experience disturbances of spermatogenesis. Some patients might experience testicular damage and male infertility, while others are able to preserve spermatogenesis and fertility. Therefore, strain elastography may help to distinguish between these types of patients. Two previous reports showed testicular stiffness of undescended testes after orchiopexy. Hattapoğlu et al. demonstrated that the median SWE values of testes were significantly higher in operated undescended testes than in descended and normal testes18). Durmaz et al. also demonstrated that the testicular stiffness of operated testes was significantly higher than those of the contralateral descended testes and undescended testes20). Since undescended testes have reduced numbers and delayed maturation of germ cells, they can induce interstitial fibrosis and, consequently, higher testicular stiffness20). Evaluation of testicular stiffness may be useful to estimate testicular histopathological changes such as interstitial fibrosis and the severity of histologic damage in each patient with unilateral undescended testes who undergoes orchiopexy, although further study is needed to confirm this.
The optimal age for orchiopexy remains a controversial issue, although many recent findings suggest that early intervention may be beneficial. We demonstrated in this study that the strain ratio tended to increase with postoperative months in the patients who received orchiopexy at age ≥ 2 years, while it remained constant with postoperative months in the patients who had received orchiopexy at age < 2 years. Our data may support those of previous reports, which recommended orchiopexy as early as possible to avoid testicular damage.
There are some limitations to the present study. First, the sample size was relatively small and future studies will require larger study populations. Second, we did not show a statistically significant correlation between the strain ratio and post-operated months. Third, we also did not investigate a correlation between the testicular stiffness and testicular histopathological findings. Since testicular biopsy is no longer indicated for undescended testes, we cannot obtain histopathological data from the patients. Forth, one operator performed all of the examinations, and we did not evaluate interobserver variability. Although Agladioglu et al. have shown that the interobserver agreement of ultrasound strain elastography was excellent for the elasticity pattern and the concordance of the strain ratios between the observers was excellent22), this should be further explored in future studies. Fifth, we did not measure pre-operative stiffness, and therefore, could not compare the stiffness between pre- and post-operated testis. This is due to the measurement method of testicular stiffness by ultrasound strain elastography. As described above, we measured the strain ratios as the ratios of the elasticities of contralateral descended testes to the elasticities of the operated testes. The testicular stiffness was evaluated by causing bilateral testicular tissue distortion with an echo probe. This method is characterized by that both testes must be visualized in the same field of view by strain elastography simultaneously. Therefore, we cannot measure the stiffness of pre-operated testis since pre-operative undescended (inguinal) testis and descended (scrotal) testis cannot be visualized in the same field of view in the ultrasound image because of the distance between both testes. Because this is a preliminary study, further study will be needed.
Conclusions
In this study we demonstrated that the strain ratio tended to increase over time in patients who underwent orchiopexy at age ≥ 2 years, while it remained constant in patients who received orchiopexy at age < 2 years. Evaluation of testicular stiffness may be able to be used in the follow-up period after orchiopexy as a complementary method to hormonal evaluation, testicular size measurement, semen analysis, and testicular biopsy to estimate histopathological findings and fertility potential in patients with unilateral undescended testes who had undergone orchiopexy. In addition, our data may support those of previous reports, which recommended orchiopexy as early as possible to avoid testicular damage, although further study is needed to confirm these conclusions.
References
- 1. Loebenstein M, Thorup J, Cortes D, Clasen-Linde E, Hutson JM, Li R. Cryptorchidism, gonocyte development, and the risks of germ cell malignancy and infertility:A systematic review. J Pediatr Surg, 55:1201-1210, 2020.
- 2. Suskind A, Hayner-Buchan A, Feustel P, Kogan BA, Fibrosis correlates with detailed histological analysis of human undescended testes. BJU Int, 101:1441-1445, 2008.
- 3. Hanerhoff BL, Welliver C. Does early orchidopexy improve fertility? Transl Androl Urol, 3: 370-376, 2014.
- 4. Huff DS, Hadziselimovic F, Snyder HM 3rd, Duckett JW, Keating MA. Postnatal testicular maldevelopment in unilateral cryptorchidism. J Urol, 142:546-548, 1989.
- 5. Lee PA, O’Leary LA, Songer NJ, Bellinger MF, LaPorte RE. Paternity after cryptorchidism:lack of correlation with age at orchiopexy. Br J Urol, 75:704-707, 1995.
- 6. McAleer IM, Packer MG, Kaplan GW, Scherz HC, Krous HF, Billman GF. Fertility index analysis in cryptorchidism. J Urol, 153:1255-1258, 1995.
- 7. Sigrist RMS, Liau J, Kaffas AE, Chammas MC, Willmann JK. Ultrasound Elastography:Review of Techniques and Clinical Applications. Theranostics, 7:1303-1329, 2017.
- 8. Çildağ MB. Evaluation of Pediatric Undescended Testes with Elastosonography. J Med Ultrasound, 25:157-160, 2017.
- 9. Cobellis G, Noviello C, Nino F, et al. Spermatogenesis and cryptorchidism. Front Endocrinol (Lausanne), 5:63, 2014.
- 10. Amat P, Paniagua R, Montero J. Seminiferous tubule degeneration in human cryptorchid testes. J Androl, 6:1-9, 1985.
- 11. Dietrich CF, Barr RG, Farrokh A, et al. Strain elastography—how to do It? Ultrasound Int Open, 3:E137-E149, 2017.
- 12. Cotoi L, Amzar D, Sporea I, et al. Shear Wave Elastography versus Strain Elastography in Diagnosing Parathyroid Adenomas. Int J Endocrinol, 2020:3801902, 2020.
- 13. Dewall RJ. Ultrasound elastography:principles, techniques, and clinical applications. Crit Rev Biomed Eng, 41:1-19, 2013.
- 14. Marsaud A, Durand M, Raffaelli C, et al. Elastography shows promise in testicular cancer detection. Prog Urol, 25:75-82, 2015.
- 15. Dudea SM, Ciurea A, Chiorean A, Botar-Jid C. Doppler applications in testicular and scrotal disease. Med Ultrason, 12:43-51, 2010.
- 16. Bota S, Herkner H, Sporea I, et al. Meta-analysis:ARFI elastography versus transient elastography for the evaluation of liver fibrosis. Liver Int, 33:1138-1147, 2013.
- 17. Shin HJ, Lee YS, Yoon H, et al. Testicular volume and elasticity changes in young children with undescended testes. Med Ultrason, 19:380-385, 2017.
- 18. Hattapoğlu S, Göya C, Arslan S, et al. Evaluation of postoperative undescended testicles using point shear wave elastography in children. Ultrasonics, 72:191-194, 2016.
- 19. Ucar AK, Alis D, Samanci C, et al. A preliminary study of shear wave elastography for the evaluation of unilateral palpable undescended testes. Eur J Radiol, 86:248-251, 2017.
- 20. Durmaz MS, Sivri M, Sekmenli T, Kocaoğlu C, Çiftçi İ. Experience of Using Shear Wave Elastography Imaging in Evaluation of Undescended Testes in Children:Feasibility, Reproducibility, and Clinical Potential. Ultrasound Q, 34:206-212, 2018.
- 21. Turna O, Alis D. A comparative study of shear wave elastography in the evaluation of undescended and retractile testes in a pediatric population. J Med Ultrason, 46:231-237, 2019.
- 22. Agladioglu K, Herek D, Herek O, Agladioglu SY, Cördük N, Ozhan B. Can ultrasound elastography be used as a new technique in the differentiation of undescended testes and reactive lymph nodes in children? Clin Radiol, 70:1269-1275, 2015.