Article ID: 2019-33
Article ID: 2019-33
Introduction: The benefits of a sitting position for neurosurgery involving the posterior fossa remain controversial. The main concern is the risk of venous air embolism (VAE). A recent study showed that the rate of VAE was higher when the head was elevated to 45° than when it was elevated to 30°. However, the degree of head elevation that causes clinically important VAE is unclear. The purpose of this study was to estimate the head elevation angle at which the probability of VAE is 50% by using EtCO2 monitoring to detect of VAE.
Methods: The anesthesia records of 23 patients who underwent neurosurgery in a sitting position were reviewed retrospectively. Intraoperative ventilation was set to maintain EtCO2 at approximately 38-42 mmHg. The head elevation angle in each case was determined from a photograph taken by the anesthesiologist or brain surgeon. Nineteen of the 23 cases had photographs available that contained a horizontal reference in the background. Seven cases were treated as VAE during the operation. Six of these cases met the criteria for VAE in this study. Data analysis was performed on a total of 18 patients. The angle between the line connecting the hip joint and the shoulder joint and the horizontal reference was obtained by ImageJ software. Logistic regression was performed using the Python programming language to determine the head elevation angle at which the probability of air embolism was 50%.
Results: The decision boundary in the logistic regression was 35.7°. This head elevation angle was the boundary where the probability of VAE was 50%.
Conclusion: The angle of head elevation that caused clinically important VAE was estimated to be 35.7°.
The benefits of a semi-sitting position for neurosurgery involving the posterior fossa remain controversial1). The semi-sitting position offers a number of advantages for the neurosurgeon, including gravitational drainage of venous blood and cerebrospinal fluid from the surgical site, which improves the anatomic orientation and surgical access to midline structures, and decreased intracranial pressure2). There are also several advantages for the anesthesiologist, including ventilation with a lower airway pressure, less impairment of diaphragmatic motion, and improved access to the tracheal tube3). However, despite these advantages, there are some complications related to use of a semi-sitting position, in particular the risk of venous air embolism (VAE)4). An air embolism occurs when the pressure in a venous vessel is decreased to a level that air may enter5). The reported incidence of VAE associated with sitting neurosurgical procedures ranges widely from 1.6%6) to 76%7) depending on the sensitivity of the monitoring measures used and the results of different patient-positioning techniques8). A recent study found a higher incidence of VAE when the angle of elevation was 45° than when it was 30°9). However, the angle of elevation that causes clinically important VAE is unknown. The purpose of this study was to estimate the head elevation angle at which the probability of VAE is 50% by using EtCO2 monitoring to detect of VAE.
A semi-sitting position was used in a manner that has been reported previously10). All patients were screened for patent foramen ovale by transesophageal echocardiography (TEE) preoperatively. If the patient was detected the presence of patent foramen oval, prone or park bench position was chosen during the surgery to avoid potential paradoxical air embolism and they were not included in this study11). Total intravenous anesthesia consisting of propofol and remifentanil was administered in all cases except in one patient who was on dialysis. Routine monitoring included electrocardiography, pulse oximetry, invasive arterial pressure measurement, and urine output. A bispectral index monitor was applied to assess the depth of anesthesia. Electrophysiologic monitoring of somatosensory and motor evoked potentials was performed intraoperatively as necessary. Posture preparation was performed as follows. The upper body and legs were elevated by bending the operating table to a position that allowed hip flexion to a maximum of 90°;the knees were kept at 30° of flexion to avoid overstretching of the tendons and nerves in the legs. All extremities were supported by gel pads to avoid pressure sores. The setting of mechanical ventilation during the operation was as follows. FiO2 was set to 0.4. The respiratory frequency was 10-12 times/min, and the airway pressure was 30 cmH2O or less. The ventilation volume was adjusted so that EtCO2 was about 38-42 mmHg. A positive end-expiratory pressure of 5 cmH2O was applied in all cases. A central venous catheter was inserted into the axillary vein with infraclavicular access in all patients12). The position of the tip of the central venous catheter was evaluated by saline flush and echocardiography13). Intraoperative VAE was diagnosed mainly using a sudden decrease in end-tidal CO2 (EtCO2) and supplementary precordial Doppler monitoring. VAE onset was reconfirmed by air aspiration from a central venous catheter. If VAE occurred during neurosurgery in the semi-sitting position, the emergency measures outlined in the VAE section of the operating room crisis checklist14) were implemented, i.e., the FIO2 was increased to 1.0 and the surgeon was required to find and close off the air entry source while intermittent jugular compressions were gently performed by an anesthesiologist.
Study designAfter obtaining approval from the ethics committee of our institute (reference number: H30-011), the anesthesia records of 23 patients who underwent neurosurgery in the semi-sitting position between March 29, 2017 and August 22, 2018 at our institution were reviewed. Most patients had an American Society of Anesthesiologists physical status classification of I or II. A clinically significant VAE was defined as the case in which the air was drawn from a central venous catheter simultaneously with a sudden reduction of ≥4 mmHg in the end-tidal carbon dioxide15). Postural photographs obtained by the anesthesiologist or neurosurgeon were analyzed. The records of 19 cases that were photographed from a lateral viewpoint with a horizontal reference in the background (Figure 1) were selected. Seven cases were treated as VAE during the operation. Six of these cases met the criteria above. Data analysis was performed on a total of 18 patients, 6 cases meeting the criteria for VAE and 12 cases without VAE. The head elevation angle was obtained as follows. The line connecting the hip joint and shoulder joint was drawn. ImageJ processing software (National Institutes of Health, Bethesda, MD, USA) was used to determine the angle between the line and the horizontal reference16). A decreased EtCO2 was classified as 1 and an unchanged EtCO2 as 0 to allow use of the Python programming language (version 3.6.7). Logistic regression was performed using scikit-learn (version 0.20.0) from the Python library to determine the decision boundary for 50% probability of an air embolism. The statistical analysis was performed using Python and SciPy (scientific library version 1.1.0). The Mann-Whitney U test was used to compare the means of continuous variables. The descriptive data are presented as the mean ± standard deviation. A p-value <0.05 was considered statistically significant.

Horizontal baseline in the background and the head elevation angle
Red lines : horizontal reference in the background
Green line : line connecting the shoulder joint and the hip joint
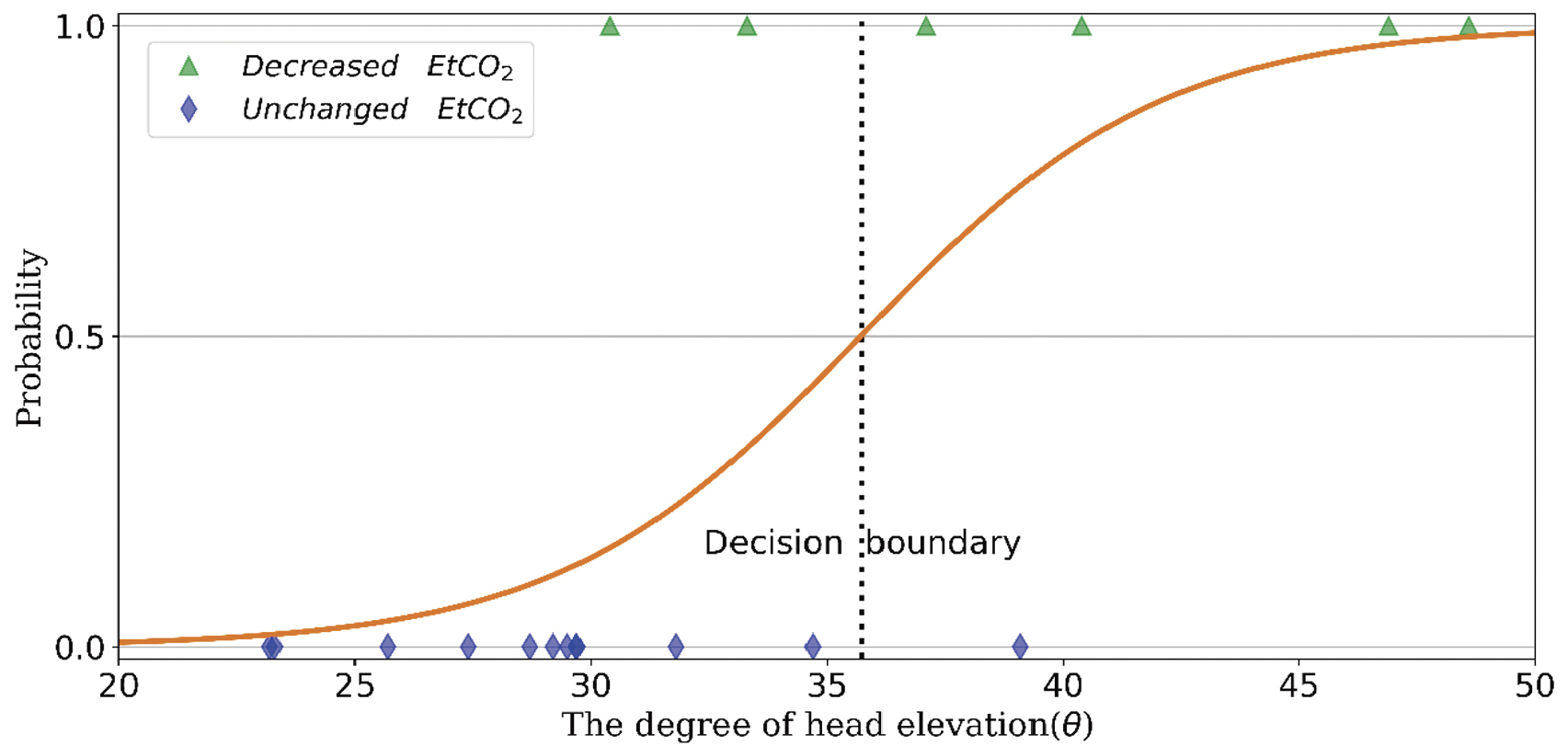
Logistic regression of head elevation angle and incidence of VAE, and its decision boundary
The decision boundary in the logistic regression was 35.7°.
The characteristics of the 18 patients are presented in Table 1. Details of the cases that developed VAE are shown in Table 2. EtCO2 is the value before and at the onset of VAE. Blood pressure and SpO2 in Table 2 are the lowest values at the time of the VAE onset. There were no cases of permanent morbidity and mortality related to the semi-sitting position. Surgery was completed in a semi-sitting position without interruption in all patients. The decision boundary in logistic regression was 35.7° (Figure 2). Patients with trigeminal neuralgia, glossopharyngeal neuralgia, or hemifacial spasm underwent microvascular decompression (MVD;Table 1). The head elevation angles used for removal of a brain tumor (BT) and clipping of a vertebral artery aneurysm (VAA) (39.3 ± 6.3°) were significantly greater than those used for MVD (31.2 ± 5.8°; p=0.023, Mann-Whitney U test).
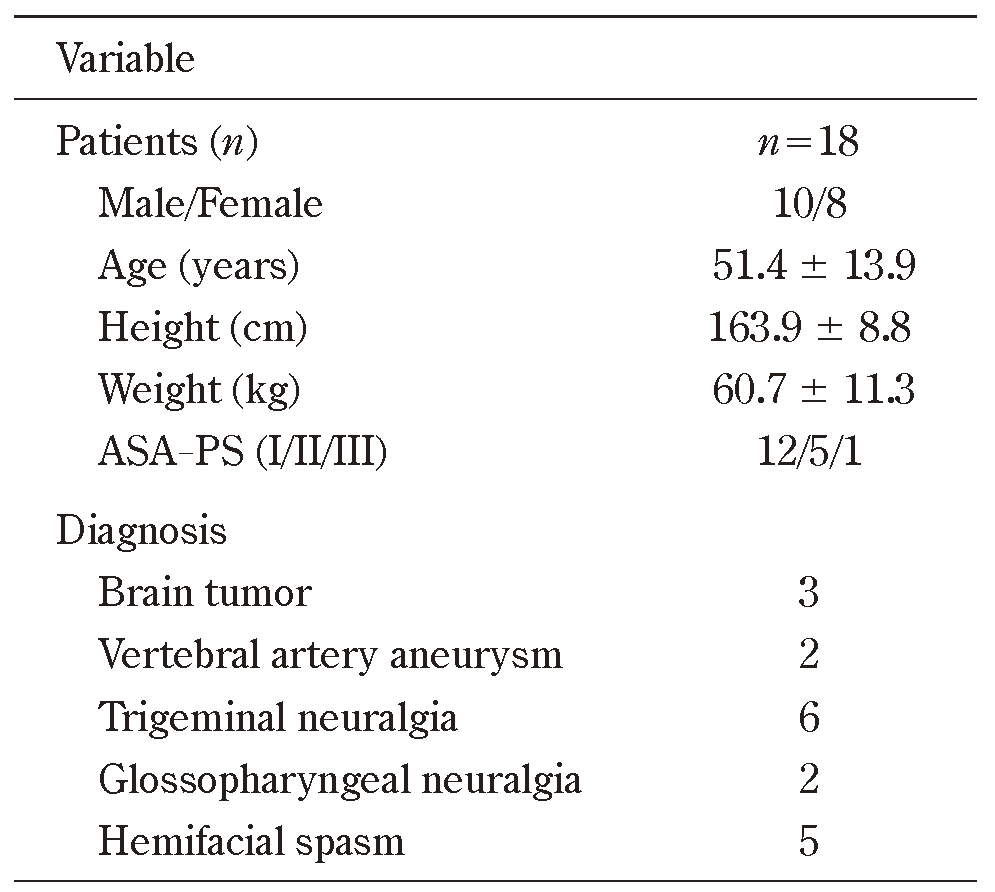
ASA, American Society of Anesthesiologists ; PS, physical status
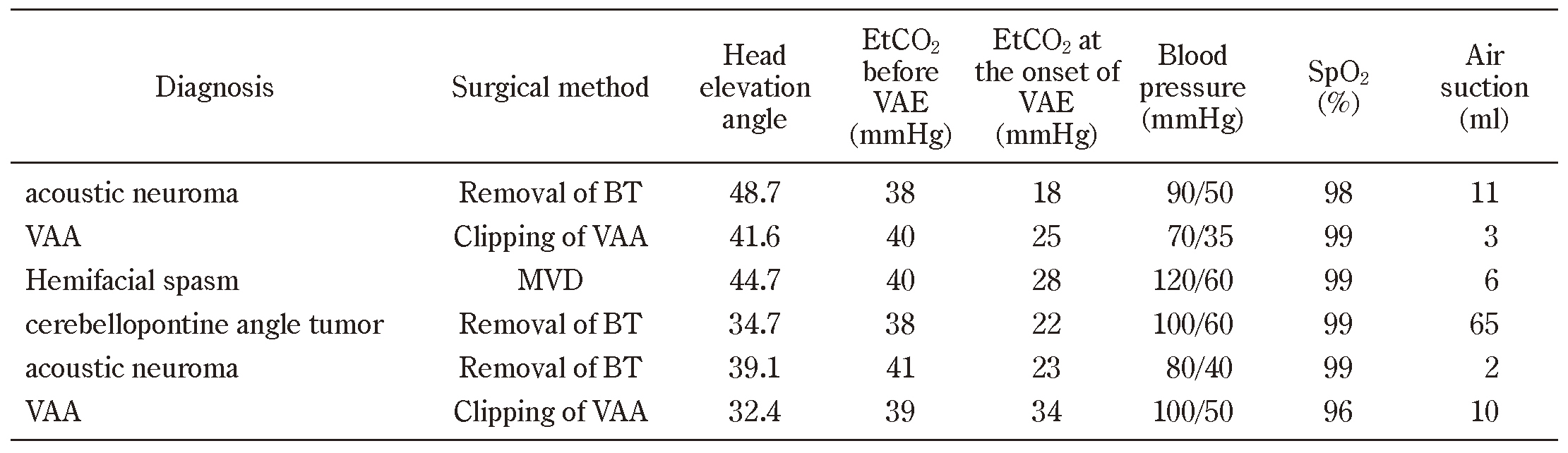
BT, brain tumor ; VAA, vertebral artery aneurysm ; MVD, microvascular decompression
VAE is one of the principal reasons for the decline in the use of the sitting position in neurosurgical practice17). Although TEE is the most sensitive method for detecting intracardiac air, TEE will detect tiny microbubbles that may be of no clinical importance18). Moreover, TEE may lead to complications in esophageal bleeding, displacement of the endotracheal tube, and risk of glottis injury with prolonged use19). In consideration of the fact that TEE detects even minute air which leads to no adverse sequelae and its invasiveness20), the fall of EtCO2 was used to detect VAE. Continuous monitoring of EtCO2 offers intermediate sensitivity for VAE detection21). Furthermore, we confirmed the onset of VAE by suctioning air from the central venous catheter. The rates of VAE that occur with sitting neurosurgical procedures have been reported in a wide range, from 1.6% to 76%8). This range is too wide to be explained only by different detection methods. These results reflect there is no standardized head elevation angle. Air can be entrained because the venous pressure at the wound level is usually negative22). As the elevation angle increases, the vertical distance between the head and the right atrium increases. Therefore, the head elevation angle indirectly reflects gravitational gradients. Perhaps because there was no concept of a standard head elevation angle, few papers have clearly described the relationship between the head elevation angle and the occurrence of VAE. Only recent studies have shown that the incidence of VAE is higher at 45° elevation than at 30° elevation9). However, how many degrees of head elevation cause VAE is unknown.
In this study we estimated the angle of elevation at which the probability of VAE is 50%. Looking at Figure 2 from another perspective, VAE occurrence and non-occurrence are mixed when the head elevation angle is between 30° and 40°. Table 2 shows that the minimum angle at which VAE occurred is 32.4 degrees in this study. Türe H et al. described that VAE resulting in EtCO2 reduction was 8.0% in the 30° group and 50.0% in the 45° group9). In terms of angles that do not affect EtCO2, 30 degrees can be said to apply.
Logistic regression is a classification algorithm that assigns observations to discrete classes and outputs classification probabilities23). The boundary at which the probability of classification is 50% is called the decision boundary. The decision boundary in this study was that the probability of developing VAE is 50%. Furthermore, it can be inferred from the nature of logistic regression that the higher the angle, the higher the incidence of VAE.
There are some limitations to this study. First, the sample size was relatively small because the study involved a rare problem and was performed at a single center. Second, using EtCO2 as an indicator of VAE may underestimate the incidence of VAE. In addition, blood gas analysis should have been done for the treatment. Finally, the head elevation angle may be affected by the operative method. We found that the head elevation angles used for the removal of a BT and clipping of a VAA were significantly greater than those used for MVD. The head elevation angle may need to be greater for the removal of a BT and clipping of a VAA to obtain the necessary view for surgery.
In this study, the head elevation angle causing clinically important VAE in patients undergoing neurosurgery in the semi-sitting position was estimated to be 35.7°. The sitting position affords many advantages with acceptable risks in adult neurosurgical patients. However, we need to minimize preventable complications. When creating a semi-sitting position for neurosurgery, it may be better to consider the head elevation angle associated with the onset of VAE.
The authors declare no conflicts of interest associated with this manuscript.
Ethics approval and consent to participateThe protocol for this retrospective study was approved by the Minami Tohoku Hospital Ethics Committee (reference number: H30-011). The requirement for informed consent was waived in view of the retrospective nature of the research.