Methods
Study 1: Relationship between FMD of the Brachial Artery and serum Potassium Levels
A total of 4502 Japanese subjects were recruited from FMD-J Study A (n=679), FMD-J Study B (n=966), and Hiroshima University Vascular Function (HUVF) registry (n=2857). Detailed information on the subjects and protocol of the FMD-J study is publicly available11). In brief, the FMD-J study was a prospective multicenter study conducted at 22 university hospitals and affiliated clinics in Japan to examine the usefulness of FMD assessment for the management of patients at risk for cardiovascular disease. Patients aged 20 to 74 years who had been diagnosed with coronary artery disease were enrolled in study A and patients aged 20 to 74 years with controlled hypertension or diabetes mellitus who had been receiving antihypertensive or antidiabetic treatment for at least 6 months were enrolled in study B. Some of the data from the FMD-J study were previously reported elsewhere12, 13). In the HUVF registry, subjects aged 20 years or older who underwent a vascular function test at Hiroshima University Hospital between September 2007 and June 2020 were recruited. Subjects with inadequate FMD recordings (n=144), atrial fibrillation (n=190), malignancy (n=104), severe valvular heart disease (n=59), secondary hypertension (n=551), including primary aldosteronism (PA), Cushing syndrome, and subclinical Cushing syndrome, subjects undergoing treatment with nitrate (n=368), and subjects receiving dialysis (n=41) were excluded (Fig.1). Finally, a total of 3045 subjects (1964 men and 1081 women; mean age, 62.3±13.8 years) were enrolled in study 1 for investigating the association between FMD of the brachial artery and serum potassium levels. This study was performed in accordance with the 1975 Declaration of Helsinki. The ethical committees of the participating institutions approved the study protocol. Informed consent for participation in the study was obtained from all subjects. The protocol was registered in the University Hospital Medical Information Network Clinical Trials Registry (UMIN000012950, UMIN000012951, and UMIN000039512).

Among the 1787 subjects enrolled in study 1 from the HUVF registry, 209 subjects without measurement of NID of the brachial artery were excluded. A total of 1578 subjects (1001 men and 577 women; mean age, 61.8±16.3 years) were enrolled in study 2 for investigating the association between NID of the brachial artery and serum potassium levels (Fig.1). This study was performed in accordance with the Declaration of Helsinki. The Hiroshima University Hospital institutional review board approved the study protocol. Informed consent for participation in the study was obtained from all subjects. The protocol was registered in the University Hospital Medical Information Network Clinical Trials Registry (UMIN000039512).
Study Protocol
The subjects fasted the previous night for at least 8 hours and abstained from consuming caffeine, alcohol, and antioxidant vitamins and from smoking on the day of the examination. The subjects were kept in the supine position in a quiet, dark, air-conditioned room (constant temperature of 23-26℃) throughout the study. A 23-gauge polyethylene catheter was inserted into the left deep antecubital vein to obtain blood samples for measurements of biochemical parameters, including potassium. At least 20 min after maintaining the supine position, the vascular function test was performed by skilled and trained physicians or sonographers without detailed knowledge of baseline clinical characteristics of the subjects.
Measurements of FMD and NID of the Brachial Artery
The same protocol as that used for the measurement of FMD of the brachial artery was used in both the FMD-J study and the HUVF registry. In both studies, FMD and NID were measured using UNEXEF 18G (UNEX Co, Nagoya, Japan), an ultrasound instrument specialized for FMD and NID measurements that is equipped with a high-resolution linear array transducer (10-MHz). This device has an automated edge detection system for continuous measurement of brachial artery diameter. Vascular response to reactive hyperemia in the brachial artery was used for assessment of endothelium-dependent FMD. A blood pressure cuff was placed around the forearm. The brachial artery was scanned longitudinally 5 to 10 cm above the elbow. When the clearest B-mode image of the anterior and posterior intimal interfaces between the lumen and vessel wall was obtained, the transducer was held at the same point throughout the scan by a special probe holder (UNEX Co) to ensure consistency of the image. Depth and gain setting were set to optimize the images of the arterial lumen wall interface. When the tracking gate was placed on the intima, the artery diameter was automatically tracked, and the waveform of diameter changes over the cardiac cycle was displayed in real time using the FMD mode of the tracking system. This allowed the ultrasound images to be optimized at the start of the scan and the transducer position to be adjusted immediately for optimal tracking performance throughout the scan. Pulsed Doppler flow was assessed at baseline and during peak hyperemic flow, which was confirmed to occur within 15 s after cuff deflation. Blood flow velocity was calculated from the color Doppler data and was displayed as a waveform in real time. The baseline longitudinal image of the artery was acquired for 30 s, and then the blood pressure cuff was inflated to 50 mm Hg above systolic pressure for 5 min. The longitudinal image of the artery was recorded continuously until 5 min after cuff deflation. Pulsed Doppler velocity signals were obtained for 20 s at baseline and for 10 s immediately after cuff deflation. Changes in brachial artery diameter were immediately expressed as percentage change relative to the vessel diameter before cuff inflation. FMD was automatically calculated as the percentage change in peak vessel diameter from the baseline value. Percentage of FMD [(Peak diameter - Baseline diameter)/Baseline diameter] was used for analysis14). All of the sonographers specialized in FMD measurement at the participating institutions received training for a standard protocol of FMD measurement and training for scanning and analysis of the record at the core laboratory located in Tokyo Medial University in the FMD-J study. All recordings of brachial artery scans obtained during the measurement of FMD were sent from the participant institutions to the core laboratory in Tokyo Medical University by universal serial bus flash drives and were individually analyzed by a well-experienced reader at the core laboratory without any information about the patients in the FMD-J study. The intra-class correlation coefficient between each of the participating institutions and the core laboratory has been previously described15). The correlation coefficient between FMD analyzed at the core laboratory and participant institutions was 0.84 (P<0.001). Intra-observer variability (coefficient of variation) was 10.1-11.2%16).
The response to nitroglycerine was used for assessment of endothelium-independent vasodilation. After acquiring baseline rest images for 30 seconds, a sublingual tablet (75 µg nitroglycerine) was given, and image of the artery were recorded continuously until the dilation reached a plateau after administration of nitroglycerine. We carefully checked in the mouth to confirm that tablet had been dissolved and absorbed a few minutes after administration of nitroglycerine. Subjects in whom the sublingually administered nitroglycerine tablet was not dissolved during the measurement were not included in this study. Nitroglycerine-induced vasodilation was automatically calculated as a percent change in peak vessel diameter from the baseline value. Percentage of NID [(Peak diameter - Baseline diameter)/Baseline diameter] was used for analysis.
Cardiovascular Risk Factors and Cardiovascular Disease
Hypertension was defined as treatment with oral antihypertensive agents or systolic blood pressure of ≥ 140 mm Hg and/or diastolic blood pressure of ≥ 90 mm Hg without medication17). Dyslipidemia was defined according to the third report of the National Cholesterol Education Program18). Diabetes was defined according to the recommendations of the American Diabetes Associations19). We defined smokers as those who were current smokers. The estimated glomerular filtration rate (eGFR) was calculated using the Japanese eGFR equation20). Chronic kidney disease (CKD) was defined as eGFR <60 ml/min/1.73 m2 21). Coronary artery disease and cerebrovascular disease were included in cardiovascular diseases. Coronary artery disease included angina pectoris, myocardial infarction, and unstable angina. Cerebrovascular disease included ischemic stroke, hemorrhagic stroke, and transient ischemic attack.
Statistical Analysis
All reported probability values were 2-sided, and a probability value of <0.05 was considered statistically significant. Continuous variables are summarized as means±SD and were compared by using ANOVA with Tukey’s post hoc comparisons for multiple groups. Categorical variables are presented as frequencies and percentages. Univariate linear regression analyses were performed to assess relationships between serum potassium levels and vascular function tests. Multiple linear regression analyses were performed to identify independent variables associated with FMD and NID. Age, sex, body mass index, systolic blood pressure, heart rate, triglycerides, high-density lipoprotein (HDL) cholesterol, glucose, eGFR, serum sodium levels, current smoking, cardiovascular disease, angiotensin receptor blockers/angiotensin-converting enzyme inhibitors (ARBs/ACEIs), diuretics, mineralocorticoid receptor blockers (MRAs), calcium channel blockers, β-blockers, lipid-lowering drugs, hypoglycemia drugs, and serum potassium levels were entered into the model. Multiple logistic regression analyses were performed to identify independent variables associated with endothelial dysfunction defined as the lowest tertile of FMD (≤ 2.5%) and vascular smooth muscle dysfunction defined as the lowest tertile of NID (≤ 9.3%). Age, sex, and categories of serum potassium levels were entered into the model. The data were processed using JMP version pro 15 (SAS Institute, Cary, NC).
Results
Study 1
The baseline clinical characteristics of the subjects in study 1 are summarized in Table 1. Of the 3045 subjects, 2561 (84.2%) had hypertension, 2148 (71.2%) had dyslipidemia, 851 (28.0%) had diabetes mellitus, 488 (16.3%) were current smokers, 724 (23.8%) had CKD, and 718 (23.8%) had cardiovascular diseases. Among the subjects, 2350 (77.2%) were being treated with antihypertensive drugs. The mean values were 4.1±3.0% (median, 3.9%; interquartile range, 1.9-6.0%; range, -7.0-18.5%) for FMD of the brachial artery, 4.2±0.4 mmol/L (median, 4.2 mmol/L; interquartile range, 4.0-4.4 mmol/L; range, 3.0-6.3 mmol/L) for serum potassium, and 141±3 mmol/L (median, 141 mmol/L; interquartile range, 140-142 mmol/L; range, 123-155 mmol/L) for serum sodium. There was a significant positive correlation between FMD and serum potassium levels (r=0.09, P<0.001) (Fig.2A). The relationship between serum potassium levels and FMD was consistent across the three study cohorts; Serum potassium levels significantly correlated with FMD in FMD-J Study A (r=0.11, P=0.03), FMD-J Study B (r=0.10, P=0.005), and the HUVF registry (r=0.07, P=0.004). There was a significant correlation between serum potassium levels and serum sodium levels (r=-0.10, P<0.001), but there was no significant correlation between serum sodium levels and FMD (r=0.02, P=0.38). Multiple linear regression analysis revealed that serum potassium levels (β=0.109, P<0.001), age (β=-0.239, P<0.001), men (β=-0.053, P=0.007), triglycerides (β=-0.041, P=0.03), eGFR (β=0.081, P<0.001), serum sodium levels (β=0.051, P=0.006), current smoking (β=-0.060, P=0.002), cardiovascular disease (β=0.046, P=0.04), ARBs/ACEIs (β=-0.061, P=0.002), calcium channel blockers (β=-0.143, P<0.001), β-blockers (β=0.076, P<0.001), and hypoglycemic drugs (β=-0.041, P=0.04) were significantly associated with FMD (Table 2).
Table 1.
Clinical Characteristics of the Subjects in Study 1
| Variables |
Total
n = 3045
|
Subjects without ARBs/ACEIs/ Diuretics/MRAs n = 1276
|
Subjects with ARBs/ACEIs/ Diuretics/MRAs n = 1769
|
| Potassium, mmol/L |
4.2±0.4 |
4.2±0.4 |
4.2±0.4 |
| Age, y |
62.3±13.8 |
58.4±16.5 |
65.1±10.7 |
| Male, n (%)
|
1964 (64.5) |
795 (62.3) |
1169 (66.1) |
| Body mass index, kg/m2
|
24.1±3.8 |
23.1±3.5 |
24.9±3.8 |
| Systolic blood pressure, mm Hg |
130.7±17.1 |
130.8±18.1 |
130.6±16.4 |
| Diastolic blood pressure, mm Hg |
77.0±11.6 |
77.9±12.4 |
76.4±10.9 |
| Heart rate, bpm |
69.2±11.9 |
68.9±11.9 |
69.5±11.8 |
| Total cholesterol, mmol/L |
4.94±0.94 |
5.06±0.98 |
4.85±0.89 |
| Triglycerides, mmol/L |
1.55±1.14 |
1.52±1.24 |
1.58±1.07 |
| HDL cholesterol, mmol/L |
1.51±0.42 |
1.57±0.44 |
1.47±0.41 |
| LDL cholesterol, mmol/L |
2.74±0.83 |
2.82±0.86 |
2.68±0.80 |
| Glucose, mmol/L |
6.23±1.92 |
6.17±2.00 |
6.26±1.86 |
| HbA1c, % |
6.0±1.0 |
5.9±0.9 |
6.1±0.8 |
| eGFR, ml/min/1.73m2
|
72.2±18.9 |
77.1±19.1 |
68.7±18.0 |
| Sodium, mmol/L |
141±3 |
141±3 |
141±2 |
| Current smokers, n (%)
|
488 (16.3) |
269 (21.5) |
214 (12.6) |
| Comorbidities |
|
|
|
| Hypertension, n (%)
|
2561 (84.2) |
793 (62.3) |
1769 (100) |
| Dyslipidemia, n (%)
|
2148 (71.2) |
804 (64.2) |
1344 (76.2) |
| Diabetes mellitus, n (%)
|
851 (28.0) |
276 (21.7) |
575 (32.5) |
| Chronic kidney disease, n (%)
|
724 (23.8) |
203 (15.9) |
521 (29.5) |
| Cardiovascular disease, n (%)
|
718 (23.8) |
196 (15.5) |
522 (29.7) |
| Coronary artery disease, n (%)
|
646 (21.3) |
164 (12.9) |
482 (27.4) |
| Cerebrovascular disease, n (%)
|
125 (4.1) |
42 (3.3) |
83 (4.7) |
| Medication use |
|
|
|
| Antihypertensive drug, n (%)
|
2350 (77.2) |
581 (46.3) |
1769 (100) |
| ARBs/ACEIs, n (%)
|
1680 (55.5) |
0 (0) |
1680 (95.0) |
| Diuretics, n (%)
|
509 (16.8) |
0 (0) |
509 (28.8) |
| MRAs, n (%)
|
112 (3.7) |
0 (0) |
112 (6.3) |
| Calcium channel blockers, n (%)
|
1538 (50.9) |
508 (40.5) |
1030 (58.2) |
| β-blockers, n (%)
|
607 (20.1) |
150 (11.9) |
457 (25.8) |
| Lipid-lowering drugs, n (%)
|
1398 (46.2) |
437 (34.8) |
961 (54.3) |
| Hypoglycemic drugs, n (%)
|
592 (19.6) |
171 (13.6) |
421 (23.8) |
| FMD, % |
4.1±3.0 |
4.6±3.2 |
3.8±2.8 |
ARB indicates angiotensin receptor blocker; ACEI, angiotensin-converting enzyme inhibitor; MRA, mineralocorticoid receptor antagonist; HDL, high-density lipoprotein; LDL, low-density lipoprotein; eGFR, estimated glomerular filtration rate; FMD, flow-mediated vasodilation.

Table 2.
Multiple Linear Regression Analyses of the Relationships Between FMD and Variables
| FMD |
| Variables |
Total |
Subjects without ARBs/ACEIs/ Diuretics/MRAs |
Subjects with ARBs/ACEIs/ Diuretics/MRAs |
| β |
VIF |
Standard error |
t value |
P value
|
β |
VIF |
Standard error |
t value |
P value
|
β |
VIF |
Standard error |
t value |
P value
|
| Potassium, mmol/L |
0.109 |
1.12 |
0.148 |
5.89 |
<0.001 |
0.123 |
1.14 |
0.250 |
4.19 |
<0.001 |
0.096 |
1.12 |
0.183 |
3.93 |
<0.001 |
| Age, y |
-0.239 |
1.61 |
0.005 |
-10.7 |
<0.001 |
-0.228 |
1.95 |
0.007 |
-5.95 |
<0.001 |
-0.215 |
1.35 |
0.007 |
-8.06 |
<0.001 |
| Men |
-0.053 |
1.26 |
0.061 |
-2.70 |
0.007 |
-0.038 |
1.36 |
0.105 |
-1.18 |
0.24 |
-0.065 |
1.22 |
0.074 |
-2.57 |
0.01 |
| Body mass index, kg/m2
|
-0.038 |
1.31 |
0.016 |
-1.91 |
0.06 |
-0.022 |
1.28 |
0.028 |
-0.70 |
0.48 |
-0.043 |
1.28 |
0.019 |
-1.65 |
0.10 |
| Systolic blood pressure, mm Hg |
0.019 |
1.10 |
0.003 |
1.04 |
0.30 |
-0.007 |
1.24 |
0.005 |
-0.22 |
0.83 |
0.041 |
1.05 |
0.004 |
1.74 |
0.08 |
| Heart rate, bpm |
0.020 |
1.10 |
0.005 |
1.07 |
0.28 |
-0.004 |
1.18 |
0.008 |
-0.15 |
0.88 |
0.041 |
1.08 |
0.006 |
1.70 |
0.09 |
| Triglycerides, mmol/L |
-0.041 |
1.20 |
0.051 |
-2.13 |
0.03 |
-0.082 |
1.18 |
0.077 |
-2.74 |
0.006 |
-0.001 |
1.24 |
0.069 |
-0.06 |
0.95 |
| HDL cholesterol, mmol/L |
-0.027 |
1.35 |
0.143 |
-1.32 |
0.19 |
0.010 |
1.32 |
0.228 |
0.32 |
0.75 |
-0.055 |
1.35 |
0.182 |
-2.05 |
0.04 |
| Glucose, mmol/L |
-0.032 |
1.32 |
0.032 |
-1.60 |
0.11 |
-0.065 |
1.30 |
0.052 |
-2.09 |
0.04 |
-0.013 |
1.37 |
0.041 |
-0.47 |
0.64 |
| eGFR, ml/min/1.73 m2
|
0.081 |
1.41 |
0.003 |
3.91 |
<0.001 |
0.093 |
1.45 |
0.006 |
2.82 |
0.005 |
0.063 |
1.27 |
0.004 |
2.45 |
0.01 |
| Sodium, mmol/L |
0.051 |
1.13 |
0.022 |
2.76 |
0.006 |
0.059 |
1.14 |
0.037 |
2.02 |
0.04 |
0.044 |
1.14 |
0.028 |
1.80 |
0.07 |
| Current smoking |
-0.060 |
1.15 |
0.076 |
-3.18 |
0.002 |
-0.076 |
1.22 |
0.117 |
-2.50 |
0.01 |
-0.042 |
1.09 |
0.101 |
-1.75 |
0.08 |
| Cardiovascular disease |
0.046 |
1.56 |
0.077 |
2.09 |
0.04 |
0.017 |
1.40 |
0.145 |
0.52 |
0.60 |
0.069 |
1.60 |
0.089 |
2.37 |
0.02 |
| ARBs/ACEIs |
-0.061 |
1.25 |
0.059 |
-3.10 |
0.002 |
|
|
|
|
|
|
|
|
|
|
| Diuretics |
0.025 |
1.15 |
0.075 |
1.34 |
0.18 |
|
|
|
|
|
|
|
|
|
|
| MRAs |
-0.006 |
1.07 |
0.144 |
-0.35 |
0.72 |
|
|
|
|
|
|
|
|
|
|
| Calcium channel blockers |
-0.143 |
1.16 |
0.056 |
-7.55 |
<0.001 |
-0.093 |
1.28 |
0.100 |
-2.98 |
0.003 |
-0.178 |
1.07 |
0.067 |
-7.49 |
<0.001 |
| β-blockers |
0.076 |
1.23 |
0.073 |
3.88 |
<0.001 |
0.040 |
1.17 |
0.144 |
1.33 |
0.18 |
0.084 |
1.24 |
0.082 |
3.30 |
0.001 |
| Lipid-lowering drugs |
0.041 |
1.46 |
0.063 |
1.95 |
0.05 |
0.012 |
1.51 |
0.113 |
0.37 |
0.71 |
0.045 |
1.36 |
0.075 |
1.69 |
0.09 |
| Hypoglycemic drugs |
-0.041 |
1.32 |
0.076 |
-2.04 |
0.04 |
-0.010 |
1.28 |
0.145 |
-0.31 |
0.76 |
-0.066 |
1.36 |
0.088 |
-2.47 |
0.01 |
The adjusted r2 of the model for FMD in all subjects was 0.13.
The adjusted r2 of the model for FMD in subjects without ARBs/ACEIs/Diuretics/MRAs was 0.12. The adjusted r2 of the model for FMD in subjects with ARBs/ACEIs/Diuretics/MRAs was 0.12.
FMD indicates flow-mediated vasodilation; ARB, angiotensin receptor blocker; ACEI, angiotensin-converting enzyme inhibitor; MRA, mineralocorticoid receptor antagonist; VIF, variance inflation factor; HDL, high-density lipoprotein; LDL, low-density lipoprotein; eGFR, estimated glomerular filtration rate.
We divided patients with normal renal function (eGFR ≥ 60 ml/min/1.73m2) into two groups according to serum potassium levels: subjects with serum potassium levels of <4.5 mmol/L and subjects with serum potassium levels of ≥ 4.5 mmol/L. The baseline clinical characteristics are summarized in Supplementary Table 1. Age, body mass index, systolic blood pressure, diastolic blood pressure, heart rate, eGFR, and prevalences of cerebrovascular disease, hypertension, antihypertension drug use, and calcium channel blocker use were significantly lower and percentages of men and current smokers, prevalences of cardiovascular disease, coronary artery disease, and lipid-lowering drug use, and FMD were significantly higher in subjects with serum potassium levels of ≥ 4.5 mmol/L than in subjects with serum potassium levels of <4.5 mmol/L among subjects with normal renal function.
Supplementary Table 1.
Clinical Characteristics
| Variables |
Potassium <4.5 mmol/L n = 1843
|
Potassium ≥ 4.5 mmol/L n = 478
|
P value
|
| Age, y |
60.3±13.6 |
58.8±16.2 |
0.04 |
| Male, n (%)
|
1153 (62.6) |
362 (75.7) |
<0.001 |
| Body mass index, kg/m2
|
24.3±4.0 |
23.6±3.7 |
0.001 |
| Systolic blood pressure, mm Hg |
131.2±16.7 |
128.5±15.9 |
0.002 |
| Diastolic blood pressure, mm Hg |
78.1±11.7 |
75.4±10.8 |
<0.001 |
| Heart rate, bpm |
70.1±11.9 |
67.9±11.5 |
<0.001 |
| Total cholesterol, mmol/L |
4.99±0.92 |
4.91±0.93 |
0.10 |
| Triglycerides, mmol/L |
1.55±1.21 |
1.44±0.89 |
0.06 |
| HDL cholesterol, mmol/L |
1.53±0.43 |
1.53±0.42 |
0.85 |
| LDL cholesterol, mmol/L |
2.77±0.82 |
2.73±0.84 |
0.29 |
| Glucose, mmol/L |
6.14±1.77 |
6.27±2.22 |
0.19 |
| HbA1c, % |
6.0±0.9 |
5.9±0.9 |
0.34 |
| eGFR, ml/min/1.73m2
|
79.8±15.4 |
77.6±13.9 |
0.004 |
| Sodium, mmol/L |
141±2 |
141±3 |
0.003 |
| Current smokers, n (%)
|
312 (17.3) |
110 (23.5) |
0.002 |
| Comorbidities |
|
|
|
| Hypertension, n (%)
|
1542 (83.9) |
350 (73.2) |
<0.001 |
| Dyslipidemia, n (%)
|
1239 (68.0) |
323 (68.0) |
0.99 |
| Diabetes mellitus, n (%)
|
462 (25.1) |
124 (26.0) |
0.69 |
| Cardiovascular disease, n (%)
|
358 (19.6) |
113 (23.8) |
0.04 |
| Coronary artery disease, n (%)
|
306 (16.7) |
110 (23.2) |
0.001 |
| Cerebrovascular disease, n (%)
|
61 (3.3) |
6 (1.3) |
0.02 |
| Medication use |
|
|
|
| Antihypertensive drug, n (%)
|
1393 (75.6) |
321 (67.2) |
<0.001 |
| ARBs/ACEIs, n (%)
|
954 (52.1) |
239 (50.2) |
0.46 |
| Diuretics, n (%)
|
266 (14.5) |
55 (11.6) |
0.10 |
| MRAs, n (%)
|
49 (2.7) |
13 (2.7) |
0.94 |
| Calcium channel blockers, n (%)
|
947 (51.7) |
190 (39.9) |
<0.001 |
| β-blockers, n (%)
|
297 (16.2) |
94 (19.8) |
0.07 |
| Lipid-lowering drugs, n (%)
|
743 (40.6) |
217 (45.6) |
0.04 |
| Hypoglycemic drugs, n (%)
|
301 (16.4) |
86 (18.1) |
0.40 |
| FMD, % |
4.2±2.9 |
4.9±3.3 |
<0.001 |
ARB indicates angiotensin receptor blocker; ACEI, angiotensin-converting enzyme inhibitor; MRA, mineralocorticoid receptor antagonist; HDL, high-density lipoprotein; LDL, low-density lipoprotein; eGFR, estimated glomerular filtration rate; FMD, flow-mediated vasodilation.
We divided the subjects into four groups according to serum potassium levels: subjects with serum potassium levels of <4.0 mmol/L (n=674), subjects with serum potassium levels of 4.0-<4.5 mmol/L (n=1635), subjects with serum potassium levels of 4.5-<5.0 mmol/L (n=616), and subjects with serum potassium levels of ≥ 5.0 mmol/L (n=120). FMD was significantly lower in subjects with serum potassium levels of <4.0 mmol/L than in those with serum potassium levels of 4.0-<4.5 mmol/L, those with serum potassium levels of 4.5-<5.0 mmol/L, or those with serum potassium levels of ≥ 5.0 mmol/L (<4.0 mmol/L, 3.7±2.8%; 4.0-<4.5 mmol/L, 4.2±2.9%; 4.5-<5.0 mmol/L, 4.5±3.2%; ≥ 5.0 mmol/L, 4.4±3.3%; P=0.002 for subjects with serum potassium levels of <4.0 mmol/L vs. subjects with serum potassium levels of 4.0-<4.5 mmol/L; P<0.001 for subjects with serum potassium levels of <4.0 mmol/L vs. subjects with serum potassium levels of 4.5-<5.0 mmol/L; P=0.04 for subjects with serum potassium levels of <4.0 mmol/L vs. subjects with serum potassium levels of ≥ 5.0 mmol/L). Multiple logistic regression analysis revealed that serum potassium levels of 4.0-<4.5 mmol/L (odds ratio [OR], 0.73; 95% confidence interval [CI], 0.60-0.88; P=0.001) and serum potassium levels of 4.5-<5.0 mmol/L (OR, 0.57; 95% CI, 0.45-0.73; P<0.001) were significantly associated with lower risk of endothelial dysfunction defined as the lowest tertile of FMD (≤ 2.5%) using serum potassium levels of <4.0 mmol/L as the reference (Supplementary Table 2). However, serum potassium levels of ≥ 5.0 mmol/L were not associated with lower risk of endothelial dysfunction (OR, 0.67; 95% CI, 0.44-1.03; P=0.07) (Supplementary Table 2).
Supplementary Table 2.
Multivariate Analysis of the Relationship between Endothelial Dysfunction and Variables
| Variables |
Odds ratio (95% Confidence Interval); P value
|
| Potassium level (mmol/L) |
Unadjusted |
Model 1 |
| <4.0 |
1 (reference) |
1 (reference) |
| 4.0-<4.5 |
0.79 (0.65-0.95); 0.01 |
0.73 (0.60-0.88); 0.001 |
| 4.5-<5.0 |
0.65 (0.52-0.82); <0.001 |
0.57 (0.45-0.73); <0.001 |
| 5.0- |
0.77 (0.51-1.17); 0.22 |
0.67 (0.44-1.03); 0.07 |
Model 1: Adjusted for age and sex.
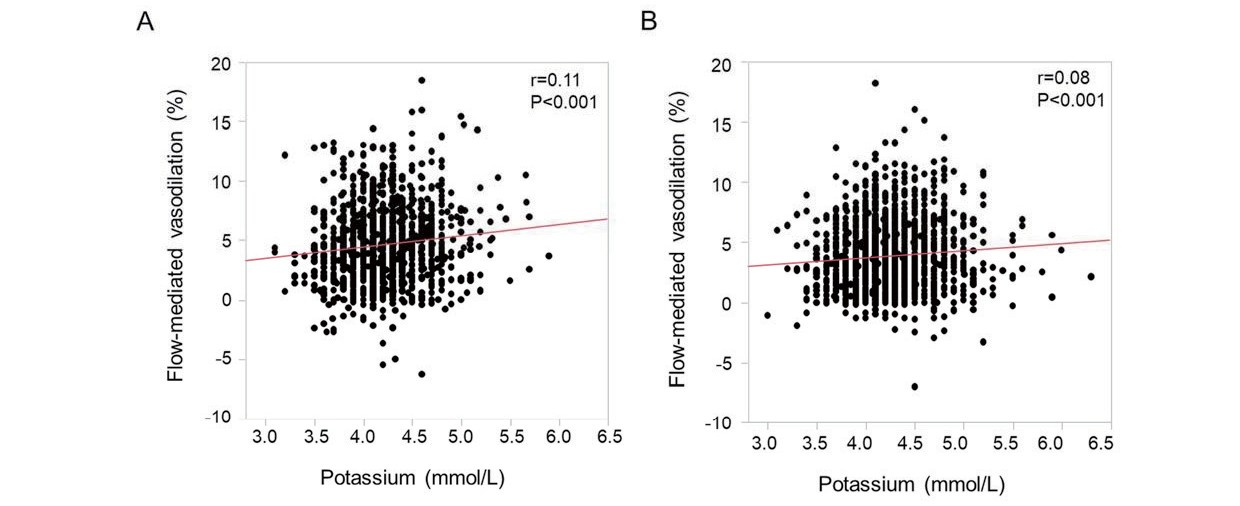
Then, we divided the subjects into two groups based on treatment with drugs that could alter serum potassium levels, including ARBs/ACEIs, diuretics and MRAs, to determine whether the association between FMD and serum potassium levels is affected by those drugs (Table 1). In 1276 subjects who were not being treated with ARBs/ACEIs, diuretics or MRAs, the mean values were 4.6±3.2% (median, 4.3%; interquartile range, 2.3-6.5%; range, -6.3-18.5%) for FMD of the brachial artery, 4.2±0.4 mmol/L (median, 4.2 mmol/L; interquartile range, 4.0-4.4 mmol/L; range, 3.1-5.9 mmol/L) for serum potassium, and 141±3 mmol/L (median, 141 mmol/L; interquartile range, 139-142 mmol/L; range, 123-154 mmol/L) for serum sodium. There was a significant positive correlation between FMD and serum potassium levels (r=0.11, P<0.001) (Supplementary Fig.1A). There was no significant correlation of serum sodium levels with serum potassium levels (r=-0.04, P=0.21) or FMD (r=0.02, P=0.55). Multiple linear regression analysis revealed that serum potassium levels (β=0.123, P<0.001), age (β=-0.228, P<0.001), triglycerides (β=-0.082, P=0.006), glucose (β=-0.065, P=0.04), eGFR (β=0.093, P=0.005), serum sodium levels (β=0.059, P=0.04), current smoking (β=-0.076, P=0.01), and calcium channel blockers (β=-0.093, P=0.003) were significantly associated with FMD in subjects who were not being treated with drugs that could alter serum potassium levels (Table 2).
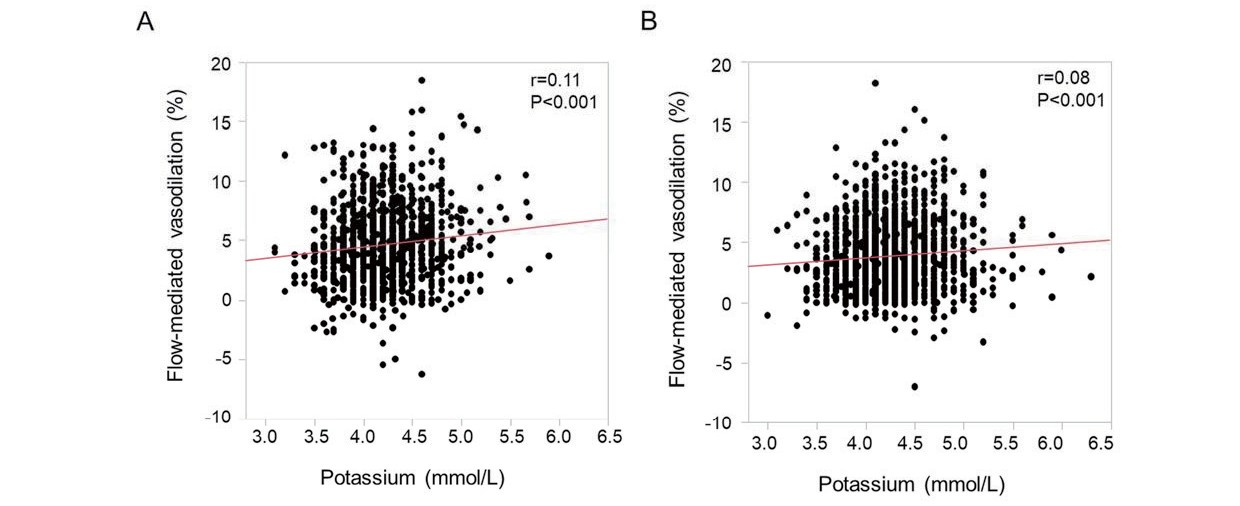
In 1769 subjects who were being treated with ARBs/ACEIs, diuretics and/or MRAs, the mean values were 3.8±2.8% (median, 3.5%; interquartile range, 1.7-5.5%; range, -7.0-18.2%) for FMD of the brachial artery, 4.2±0.4 mmol/L (median, 4.2 mmol/L; interquartile range, 4.0-4.4 mmol/L; range, 3.0-6.3 mmol/L) for serum potassium, and 141±2 mmol/L (median, 141 mmol/L; interquartile range, 140-142 mmol/L; range, 125-155 mmol/L) for serum sodium (Table 1). There was a significant positive correlation between FMD and serum potassium levels (r=0.08, P<0.001) (Supplementary Fig.1B). There was a significant correlation between serum potassium levels and serum sodium levels (r=-0.15, P<0.001), but there was no significant correlation between serum sodium levels and FMD (r=0.01, P=0.55). Multiple linear regression analysis revealed that serum potassium levels (β=0.096, P<0.001), age (β=-0.215, P<0.001), men (β=-0.065, P=0.01), HDL cholesterol (β=-0.055, P=0.04), eGFR (β=0.063, P=0.01), cardiovascular disease (β=0.069, P=0.02), calcium channel blockers (β=-0.178, P<0.001), β-blockers (β=0.084, P=0.001), and hypoglycemic drugs (β=-0.066, P=0.01) were significantly associated with FMD in subjects who were being treated with drugs that could alter serum potassium levels (Table 2).
Study 2
The baseline clinical characteristics of the subjects in study 2 are summarized in Table 3. Of the 1578 subjects, 1211 (76.9%) had hypertension, 1055 (67.8%) had dyslipidemia, 484 (30.7%) had diabetes mellitus, 305 (19.4%) were current smokers, 400 (25.3%) had CKD, and 294 (18.9%) had cardiovascular diseases. Among the subjects, 1050 (66.5%) were being treated with antihypertensive drugs. The mean values were 12.0±5.8% (median, 11.7%; interquartile range, 7.8-15.6%; range, 0-33.8%) for NID of the brachial artery, 4.2±0.4 mmol/L (median, 4.2 mmol/L; interquartile range, 4.0-4.5 mmol/L; range, 3.1-6.3 mmol/L) for serum potassium, and 141±3 mmol/L (median, 141 mmol/L; interquartile range, 139-142 mmol/L; range, 123-154 mmol/L) for serum sodium. There was a significant positive correlation between NID and serum potassium levels (r=0.11, P<0.001) (Fig.2B). There was a significant correlation between serum potassium levels and serum sodium levels (r=-0.12, P<0.001), but there was no significant correlation between serum sodium levels and FMD (r=-0.04, P=0.09). Multiple linear regression analysis revealed that serum potassium levels (β=0.098, P<0.001), age (β=-0.211, P<0.001), systolic blood pressure (β=-0.066, P=0.01), eGFR (β=0.065, P=0.03), cardiovascular disease (β=-0.066, P=0.02), calcium channel blockers (β=-0.157, P<0.001), and β-blockers (β=0.063, P=0.02) were significantly associated with NID (Table 4).
Table 3.
Clinical Characteristics of the Subjects in Study 2
| Variables |
Total n = 1578
|
Subjects without ARBs/ACEIs/ Diuretics/MRAs n = 798
|
Subjects with ARBs/ACEIs/ Diuretics/MRAs n = 780
|
| Potassium, mmol/L |
4.2±0.4 |
4.2±0.3 |
4.2±0.4 |
| Age, y |
61.8±16.3 |
56.1±18.5 |
67.7±11.0 |
| Male, n (%)
|
1001 (63.4) |
510 (63.9) |
491 (62.9) |
| Body mass index, kg/m2
|
23.7±3.8 |
22.8±3.5 |
24.6±3.8 |
| Systolic blood pressure, mm Hg |
129.7±18.2 |
130.4±18.8 |
129.1±17.6 |
| Diastolic blood pressure, mm Hg |
76.4±12.1 |
77.3±12.8 |
75.5±11.2 |
| Heart rate, bpm |
68.8±11.5 |
68.9±11.8 |
68.7±11.2 |
| Total cholesterol, mmol/L |
4.96±0.96 |
5.08±1.00 |
4.84±0.90 |
| Triglycerides, mmol/L |
1.59±1.28 |
1.58±0.44 |
1.52±0.42 |
| HDL cholesterol, mmol/L |
1.55±0.43 |
1.58±0.44 |
1.52±0.42 |
| LDL cholesterol, mmol/L |
2.71±0.84 |
2.81±0.88 |
2.61±0.79 |
| Glucose, mmol/L |
6.32±2.18 |
6.33±2.24 |
6.32±2.11 |
| HbA1c, % |
6.0±0.9 |
5.9±0.9 |
6.0±0.9 |
| eGFR, ml/min/1.73m2
|
71.6±18.9 |
78.2±18.6 |
65.0±16.9 |
| Sodium, mmol/L |
141±3 |
141±3 |
141±3 |
| Current smokers, n (%)
|
305 (19.4) |
94 (12.1) |
211 (26.6) |
| Comorbidities |
|
|
|
| Hypertension, n (%)
|
1211 (76.9) |
431 (54.2) |
780 (100) |
| Dyslipidemia, n (%)
|
1055 (67.8) |
474 (60.8) |
581 (74.8) |
| Diabetes mellitus, n (%)
|
484 (30.7) |
194 (24.4) |
290 (37.2) |
| Chronic kidney disease, n (%)
|
400 (25.3) |
119 (14.9) |
281 (36.0) |
| Cardiovascular disease, n (%)
|
294 (18.9) |
93 (11.8) |
201 (26.1) |
| Coronary artery disease, n (%)
|
225 (14.4) |
62 (7.8) |
163 (21.1) |
| Cerebrovascular disease, n (%)
|
115 (7.3) |
39 (4.9) |
76 (9.8) |
| Medication use |
|
|
|
| Antihypertensive drug, n (%)
|
1050 (66.5) |
270 (33.8) |
780 (100) |
| ARBs/ACEIs, n (%)
|
737 (47.2) |
0 (0) |
737 (94.5) |
| Diuretics, n (%)
|
209 (13.4) |
0 (0) |
209 (26.8) |
| MRAs, n (%)
|
69 (4.4) |
0 (0) |
69 (8.9) |
| Calcium channel blockers, n (%)
|
739 (47.4) |
245 (31.4) |
494 (63.3) |
| β-blockers, n (%)
|
208 (13.3) |
47 (6.0) |
161 (20.6) |
| Lipid-lowering drugs, n (%)
|
650 (41.6) |
223 (28.6) |
427 (54.7) |
| Hypoglycemic drugs, n (%)
|
332 (21.3) |
116 (14.9) |
216 (27.7) |
| NID, % |
12.0±5.8 |
13.0±5.9 |
10.9±5.4 |
ARB indicates angiotensin receptor blocker; ACEI, angiotensin-converting enzyme inhibitor; MRA, mineralocorticoid receptor antagonist; HDL, high-density lipoprotein; LDL, low-density lipoprotein; eGFR, estimated glomerular filtration rate; NID, nitroglycerine-induced vasodilation.
Table 4.
Multiple Linear Regression Analyses of the Relationships Between NID and Variables
| NID |
| Variables |
Total |
Subjects without ARBs/ACEIs/ Diuretics/MRAs |
Subjects with ARBs/ACEIs/ Diuretics/MRAs |
| β |
VIF |
Standard error |
t value |
P value
|
β |
VIF |
Standard error |
t value |
P value
|
β |
VIF |
Standard error |
t value |
P value
|
| Potassium, mmol/L |
0.098 |
1.14 |
0.375 |
3.82 |
<0.001 |
0.083 |
1.19 |
0.555 |
2.23 |
0.03 |
0.121 |
1.15 |
0.516 |
3.21 |
0.001 |
| Age, yr |
-0.211 |
2.00 |
0.012 |
-6.19 |
<0.001 |
-0.159 |
2.34 |
0.017 |
-3.04 |
0.002 |
-0.196 |
1.37 |
0.021 |
-4.75 |
<0.001 |
| Men |
0.045 |
1.31 |
0.165 |
1.64 |
0.10 |
0.028 |
1.54 |
0.260 |
0.67 |
0.51 |
0.080 |
1.25 |
0.220 |
2.03 |
0.04 |
| Body mass index, kg/m2
|
-0.048 |
1.34 |
0.043 |
-1.73 |
0.08 |
-0.057 |
1.32 |
0.067 |
-1.44 |
0.15 |
-0.035 |
1.29 |
0.057 |
-0.88 |
0.38 |
| Systolic blood pressure, mm Hg |
-0.066 |
1.14 |
0.008 |
-2.57 |
0.01 |
-0.078 |
1.30 |
0.012 |
-2.00 |
0.04 |
-0.042 |
1.11 |
0.011 |
-1.14 |
0.25 |
| Heart rate, bpm |
0.038 |
1.11 |
0.013 |
1.51 |
0.13 |
-0.008 |
1.19 |
0.018 |
-0.22 |
0.83 |
0.085 |
1.11 |
0.018 |
2.29 |
0.02 |
| Triglycerides, mmol/L |
-0.009 |
1.20 |
0.119 |
-0.34 |
0.73 |
-0.063 |
1.17 |
0.156 |
-1.71 |
0.09 |
0.061 |
1.29 |
0.189 |
1.52 |
0.13 |
| HDL cholesterol, mmol/L |
0.015 |
1.28 |
0.363 |
0.54 |
0.59 |
0.002 |
1.27 |
0.510 |
0.05 |
0.96 |
0.034 |
1.29 |
0.519 |
0.84 |
0.40 |
| Glucose, mmol/L |
-0.016 |
1.32 |
0.075 |
-0.59 |
0.55 |
-0.032 |
1.28 |
0.107 |
-0.84 |
0.40 |
-0.019 |
1.43 |
0.107 |
-0.46 |
0.64 |
| eGFR, ml/min/1.73 m2
|
0.065 |
1.63 |
0.009 |
2.13 |
0.03 |
0.119 |
1.57 |
0.014 |
2.80 |
0.005 |
0.004 |
1.32 |
0.013 |
0.10 |
0.92 |
| Sodium, mmol/L |
0.005 |
1.18 |
0.056 |
0.19 |
0.85 |
-0.012 |
1.20 |
0.084 |
-0.31 |
0.76 |
0.027 |
1.25 |
0.077 |
0.69 |
0.49 |
| Current smoking |
-0.020 |
1.23 |
0.196 |
-0.76 |
0.45 |
-0.008 |
1.29 |
0.257 |
-0.22 |
0.83 |
-0.022 |
1.16 |
0.322 |
-0.57 |
0.57 |
| Cardiovascular disease |
-0.066 |
1.45 |
0.216 |
-2.26 |
0.02 |
-0.067 |
1.29 |
0.363 |
-1.73 |
0.08 |
-0.068 |
1.59 |
0.275 |
-1.53 |
0.13 |
| ARBs/ACEIs |
-0.021 |
1.43 |
0.167 |
-0.72 |
0.47 |
|
|
|
|
|
|
|
|
|
|
| Diuretics |
0.020 |
1.21 |
0.225 |
0.76 |
0.45 |
|
|
|
|
|
|
|
|
|
|
| MRAs |
-0.007 |
1.21 |
0.371 |
-0.27 |
0.78 |
|
|
|
|
|
|
|
|
|
|
| Calcium channel blockers |
-0.157 |
1.37 |
0.163 |
-5.57 |
<0.001 |
-0.129 |
1.45 |
0.262 |
-3.14 |
0.002 |
-0.166 |
1.14 |
0.211 |
-4.41 |
<0.001 |
| β-blockers |
0.063 |
1.29 |
0.235 |
2.31 |
0.02 |
0.006 |
1.12 |
0.444 |
0.18 |
0.86 |
0.108 |
1.34 |
0.277 |
2.66 |
0.008 |
| Lipid-lowering drugs |
-0.014 |
1.50 |
0.173 |
-0.49 |
0.62 |
-0.011 |
1.61 |
0.287 |
-0.26 |
0.79 |
-0.028 |
1.30 |
0.218 |
-0.69 |
0.49 |
| Hypoglycemic drugs |
-0.018 |
1.33 |
0.195 |
-0.66 |
0.51 |
-0.037 |
1.29 |
0.325 |
-0.97 |
0.33 |
-0.010 |
1.38 |
0.249 |
-0.24 |
0.81 |
The adjusted r2 of the model for NID in all subjects was 0.17.
The adjusted r2 of the model for NID in subjects without ARBs/ACEIs/Diuretics/MRAs was 0.17. The adjusted r2 of the model for NID in subjects with ARBs/ACEIs/Diuretics/MRAs was 0.11.
NID indicates nitroglycerine-induced vasodilation; ARB, angiotensin receptor blocker; ACEI, angiotensin-converting enzyme inhibitor; MRA, mineralocorticoid receptor antagonist; VIF, variance inflation factor; HDL, high-density lipoprotein; LDL, low-density lipoprotein; eGFR, estimated glomerular filtration rate.
We divided the subjects into four groups according to serum potassium levels: subjects with serum potassium levels of <4.0 mmol/L (n=404), subjects with serum potassium levels of 4.0-<4.5 mmol/L (n=805), subjects with serum potassium levels of 4.5-<5.0 mmol/L (n=298), and subjects with serum potassium levels of ≥ 5.0 mmol/L (n=71). NID was significantly lower in subjects with serum potassium levels of <4.0 mmol/L than in those with serum potassium levels of 4.5-<5.0 mmol/L or those with serum potassium levels of ≥ 5.0 mmol/L (<4.0 mmol/L, 11.5±5.5%; 4.5-<5.0 mmol/L, 12.7±5.9%; ≥ 5.0 mmol/L, 13.5±6.6%; P=0.03 for subjects with serum potassium levels of <4.0 mmol/L vs. subjects with serum potassium levels of 4.5-<5.0 mmol/L or subjects with serum potassium levels of ≥ 5.0 mmol/L), whereas there was no significant difference in NID between subjects with serum potassium levels of <4.0 mmol/L and those with serum potassium levels of 4.0-<4.5 mmol/L (11.5±5.5% vs. 11.9±5.7%, P=0.61). Multiple logistic regression analysis revealed that serum potassium levels of 4.5-<5.0 mmol/L (OR, 0.67; 95% CI, 0.48-0.93; P=0.02) and serum potassium levels of ≥ 5.0 mmol/L (OR, 0.51; 95% CI, 0.28-0.93; P=0.03) were significantly associated with lower risk of vascular smooth muscle dysfunction defined as the lowest tertile of NID (≤ 9.3%) using serum potassium levels of <4.0 mmol/L as the reference (Supplementary Table 3). However, serum potassium levels of 4.0-<4.5 mmol/L were not associated with lower risk of vascular smooth muscle dysfunction (OR, 0.82; 95% CI, 0.63-1.06; P=0.13) (Supplementary Table 3).
Supplementary Table 3.
Multivariate Analysis of the Relationship between Vascular Smooth Muscle dysfunction and Variables
| Variables |
Odds ratio (95% Confidence Interval); P value
|
| Potassium level (mmol/L) |
Unadjusted |
Model 1 |
| <4.0 |
1 (reference) |
1 (reference) |
| 4.0-<4.5 |
0.86 (0.67-1.11); 0.25 |
0.82 (0.63-1.06); 0.13 |
| 4.5-<5.0 |
0.68 (0.49-0.94); 0.02 |
0.67 (0.48-0.93); 0.02 |
| 5.0- |
0.53 (0.29-0.94); 0.03 |
0.51 (0.28-0.93); 0.03 |
Model 1: Adjusted for age and sex.
Then, we divided the subjects into two groups based on treatment with drugs that could alter serum potassium levels, including ARBs/ACEIs, diuretics and MRAs, to determine whether the association between NID and serum potassium levels is affected by those drugs (Table 3). In 798 subjects who were not being treated with ARBs/ACEIs, diuretics or MRAs, the mean values were 13.0±5.9% (median, 12.6%; interquartile range, 8.9-16.8%; range, 0-32.2%) for NID of the brachial artery, 4.2±0.3 mmol/L (median, 4.2 mmol/L; interquartile range, 3.9-4.4 mmol/L; range, 3.1-5.9 mmol/L) for serum potassium, and 141±3 mmol/L (median, 141 mmol/L; interquartile range, 139-142 mmol/L; range, 123-154 mmol/L) for serum sodium. There was a significant positive correlation between NID and serum potassium levels (r=0.13, P<0.001) (Supplementary Fig.2A). There was no significant correlation of serum sodium levels with serum potassium levels (r=-0.06, P=0.12) or FMD (r=-0.05, P=0.17). Multiple linear regression analysis revealed that serum potassium levels (β=0.083, P=0.03), age (β=-0.159, P=0.002), systolic blood pressure (β=-0.078, P=0.04), eGFR (β=0.119, P=0.005), and calcium channel blockers (β=-0.129, P=0.002) were significantly associated with NID in subjects who were not being treated with drugs that could alter serum potassium levels (Table 4).

In 780 subjects who were being treated with ARBs/ACEIs, diuretics and/or MRAs, the mean values were 10.9±5.4% (median, 10.7%; interquartile range, 6.9-14.3%; range, 0-33.8%) for NID of the brachial artery, 4.2±0.4 mmol/L (median, 4.2 mmol/L; interquartile range, 4.0-4.4 mmol/L; range, 3.0-5.8 mmol/L) for serum potassium, and 141±3 mmol/L (median, 141 mmol/L; interquartile range, 140-142 mmol/L; range, 125-154 mmol/L) for serum sodium (Table 3). There was a significant positive correlation between NID and serum potassium levels (r=0.09, P=0.01) (Supplementary Fig.2B). There was a significant correlation between serum potassium levels and serum sodium levels (r=-0.17, P<0.001), but there was no significant correlation between serum sodium levels and FMD (r=-0.04, P=0.30). Multiple linear regression analysis revealed that serum potassium levels (β=0.121, P=0.001), age (β=-0.196, P<0.001), men (β=0.080, P=0.04), heart rate (β=0.085, P=0.02), calcium channel blockers (β=-0.166, P<0.001), and β-blockers (β=0.108, P=0.008) were significantly associated with NID in subjects who were being treated with drugs that could alter serum potassium levels (Table 4).
Discussion
In the present study, we demonstrated that FMD and NID of the brachial artery were increased with an increase in serum potassium levels and that serum potassium levels were significantly associated with FMD and NID even after adjusting for other confounding factors. The associations of serum potassium levels with FMD and NID were significant regardless of treatment with drugs that could alter serum potassium levels. To our knowledge, this is the first study to assess the relationship between serum potassium levels and vascular function and to show that serum potassium levels of 4.5-<5.0 mmol/L are associated with better vascular function in humans.
Endothelial function has been shown to be impaired in patients with cardiovascular risk factors2). One mechanism of endothelial dysfunction caused by cardiovascular risk factors is an increase in oxidative stress that refers to a condition in which the antioxidant defense system cannot sufficiently counteract excessively generated ROS3). An excess of ROS reduces NO bioavailability through increasing NO inactivation and decreasing NO production from endothelial NO synthase, leading to endothelial dysfunction2, 22).
Recent studies have shown that NID of the brachial artery itself is impaired in patients with multiple cardiovascular risk factors or cardiovascular disease and that patients with impaired NID are at high risk for cardiovascular events23-26). Oxidative stress may play a crucial role in the pathogenesis of impaired NID as an index of vascular smooth muscle function. Therefore, enhanced production of ROS would contribute not only to endothelial dysfunction but also to vascular smooth muscle dysfunction in patients with cardiovascular risk factors. Lower oxidative stress may be associated with better endothelial function and vascular smooth muscle function.
A previous in vitro study showed an inhibitory effect of potassium on the formation of ROS by vascular cells10). McCabe et al. reported that an increase in potassium concentration from 3 to 7 mmol/L caused significant decreases in ROS formation in endothelial and monocyte/macrophage cell lines and that even an increase in potassium concentration from 3 to 5 mmol/L reduced the formation of ROS in endothelial cells or monocytes/macrophages by 30% to 64%, indicating that increases in potassium concentration within the physiological range inhibit the formation of ROS in vascular cells10). We recently reported that ROS generated in circulating leukocytes could be associated with endothelial function in humans27). These findings suggest that physiological increases in serum potassium levels decrease oxidative stress by inhibiting the formation of ROS in endothelial cells and monocytes/macrophages, leading to better vascular function through increased NO bioavailability and NO signaling activity in VSMCs in individuals with higher serum potassium levels.
The present study showed that FMD and NID were significantly increased with an increase in serum potassium levels. Correlations of serum potassium levels with FMD and NID were relatively weak. However, considering that vascular function, especially FMD as an index of endothelial function, is affected by many factors such as age, blood pressure, glucose levels, lipid parameters, and smoking, weak but significant correlations between serum potassium levels and vascular function markers may be clinically relevant28, 29). In addition, the associations of serum potassium levels with FMD and NID remained significant event after adjusting for other confounding factors. Therefore, serum potassium levels should be regarded as one of the significant factors associated with vascular function.
The associations of serum potassium levels with FMD and NID were significant not only in subjects who were not treated with drugs that could alter serum potassium levels, including ARBs/ACEIs, diuretics and MRAs, but also in subjects who were being treated with drugs that could alter serum potassium levels. Therefore, in the aspect of vascular function, preventing hypokalemia and maintaining serum potassium levels at higher levels through dietary modification, potassium supplementation, and aggressive use of potassium-sparing diuretics, ARBs/ACEIs, or MRAs are recommended. However, only serum potassium levels of 4.5-<5.0 were associated with lower risk of both endothelial dysfunction and vascular smooth muscle dysfunction in the present study. In addition, a recent cohort study in which the association between serum potassium levels and all-cause mortality was investigated in a large number of subjects by using electronic medical record data has shown that subjects with hypokalemia defined as serum potassium levels of <4.0 mmol/L and subjects with hyperkalemia defined as serum potassium levels of ≥ 5.0 mmol/L have higher all-cause mortality than do subjects with serum potassium levels of 4.0-<5.0 mmol/L, which may be due to a higher risk of serious or life-threatening cardiac arrhythmias and sudden death in subjects with dyskalemia30). Therefore, it is recommended to maintain serum potassium levels at 4.5<-5.0 mmol/L in the aspects of both all-cause mortality and vascular function. Patients with renal dysfunction are predisposed to hyperkalemia. Therefore, it is recommended to maintain serum potassium levels below 5.0 mmol/L, especially in patients with renal dysfunction.
There are several limitations in this study. First, it was a cross-sectional study. Therefore, we could not establish a definitive causal relationship between serum potassium levels and vascular functions due to the nature of the study design. Second, the potassium levels ranged from 3.0 to 6.3 mmol/L in the present study. Therefore, the results cannot be extrapolated to subjects with serum potassium levels out of this range. Third, not all of the subjects underwent screening for PA. PA, the most common cause of secondary hypertension, is characterized by autonomously increased secretion of aldosterone, suppressed plasma renin activity (PRA), and hypokalemia. We have shown that FMD and NID of the brachial artery are significantly lower in patients with aldosterone-producing adenoma than in patents with essential hypertension, possibly due to a high plasma aldosterone concentration (PAC) or a high PAC/PRA ratio31, 32). We cannot rule out the possibility that undiagnosed patients with PA were included in the present study and that the inclusion of such patients contributed to the significant association between low serum potassium levels and impaired vascular function independent of serum potassium levels, though we carefully excluded patients who had been diagnosed with PA in the present study. In addition, we could not deny the possibility that the renin/aldosterone/angiotensin system is an underlying mechanism of the significant association between serum potassium levels and endothelial function even in patients without primary or secondary aldosteronism. Indeed, results of a previous study showed that high and high-normal PAC or ARR was associated with decreased FMD in young to middle-aged subjects from a general population33). However, the number of subjects with PAC or ARR measurement was too small to investigate the associations between serum potassium levels, endothelial function, and PAC or ARR in the present study. Fourth, there was no information on treatment with potassium supplements for hypokalemia or potassium binders for hyperkalemia. Fifth, we did not perform oxidative stress testing. Oxidative stress testing would enable more specific conclusions regarding the association between serum potassium levels and vascular function to be drawn. Sixth, we have no data on daily intake of potassium, alcohol, or other substances. Those data would enable more specific conclusions regarding the nutritional effect on the association between serum potassium levels and vascular function to be drawn.