2025 年 19 巻 1 号 論文ID: oa.2025-0092
2025 年 19 巻 1 号 論文ID: oa.2025-0092
Objective: Carotid artery stenting (CAS) has been reported to be a safe and effective option for treating carotid atherosclerotic disease. However, reports and studies from resource-limited countries are scarce. The published data support the use of embolic protection devices (EPDs) to reduce periprocedural stroke. This study aimed to evaluate the outcomes of CAS procedures without EPDs in Yemen, one of the lowest-income countries.
Methods: This is a retrospective cohort study regarding CAS for symptomatic carotid artery stenosis that was conducted at the stroke center of Borg Al-Atiba and American Modern Hospital during the period from March 2023 to March 2025. All patients with symptomatic carotid artery stenosis were included in the study. CAS procedures were performed by a single interventional neurologist. The primary outcomes included a 30-day periprocedural mortality, stroke, myocardial infarction, or arrhythmia. Any other complications were considered secondary outcomes.
Results: A total of 62 patients (53 males) were included in this study, with a mean age of 60.2 ± 9.7 years. All patients had symptomatic carotid artery stenosis. The technical success rate was 100%. No perioperative cerebral infarctions were observed. One patient developed transient dysarthria, but diffusion-weighted-MRI was negative. Significant bradycardia occurred in 2 patients and responded immediately to atropine. Three patients developed mild local hematoma, and 1 patient had a femoral pseudoaneurysm. Closed-cell Carotid WALLSTENT (Boston Scientific, Marlborough, MA, USA) was used as a single stent in all patients.
Conclusion: CAS conducted by a trained interventional neurologist without EPDs demonstrates a low complication rate, and it is an effective and safe option in countries with limited resources.
carotid artery stenting
CEAcarotid endarterectomy
DMdiabetes mellitus
DW-MRIdiffusion-weighted-MRI
EPDsembolic protection devices
ICAinternal carotid artery
ICUintensive care unit
LMICslow middle-income countries
NASCETNorth American Symptomatic Carotid Endarterectomy Trial
NIHSSNational Institutes of Health Stroke Scale
Establishment of stroke centers has become the standard of care for all stroke patients to reduce death and disability.1) Almost 89% of these stroke-related deaths and disabilities occur in low middle-income countries (LMICs),2,3) and approximately 20% of strokes are caused by carotid atherosclerosis, with only a limited number of studies or clinical trials exploring the outcomes of carotid revascularization for patients with carotid artery disease in resource-limited countries.4,5)
Carotid artery stenting (CAS) is a minimally invasive alternative to carotid endarterectomy (CEA) with comparable outcome.6,7) CAS is associated with a higher risk of embolic complications than CEA, so the embolic protection devices (EPDs) are used to decrease this risk.8,9) However, mainly due to financial concerns, many studies in low-income countries have reported no major differences, and in experienced hands, CAS without EPD can be performed safely.10,11)
Yemen is a resource-limited country that has been overwhelmed by devastating political crises and military conflicts since 2011. Providing stroke care services in such conditions is challenged by infrastructure limitations, shortages of training and expertise, high procedural costs and financial constraints, ongoing conflicts, and humanitarian crises.12) Therefore, the experience with neurointerventions in Yemen needs to be evaluated.
This retrospective observational study explored the outcome of CAS without EPDs for symptomatic extracranial stenosis. It was conducted between March 2023 and March 2025 at the first and only interventional neurology center—Borg Al-Atiba and American Modern Hospital in Aden City, Yemen. Ethical committee approval is not required for retrospective cohort studies in our country. The data from all adult patients (>18 years) were included. The degree of stenosis was assessed by duplex ultrasound imaging or CTA, confirmed by DSA, and calculated according to the formula proposed by the North American Symptomatic Carotid Endarterectomy Trial (NASCET) method.13) Carotid stenosis was defined as symptomatic with ≥60% stenosis. Patients with complete occlusion or incomplete data were excluded. Demographic data and risk factors (diabetes mellitus [DM], hypertension, dyslipidemia, and current smoking [or within two years]) were obtained from all patients. Neurological examinations were performed for all patients, and investigations included routine labs, duplex, and echocardiography.
CAS procedureAll CAS procedures were performed by a single interventional neurologist (2 years of training as a subspecialty in Egypt), and the stents used were all Carotid WALLSTENT (Boston Scientific, Marlborough, MA, USA). The patients should be on dual antiplatelets (aspirin 75 mg and clopidogrel 75 mg for at least 5 days before the procedure, or aspirin 75 mg and ticagrelor 90 mg twice daily). In patients who were on aspirin only, they received a ticagrelor loading dose of 190 mg at least 2 hours before the procedure. Dual antiplatelets were continued for 6 months after the procedure, then switched to a single antiplatelet, usually aspirin 100 mg once daily. If financially feasible and the plaque was stable, the CAS procedure was performed early (within 2 weeks of symptom onset). In 14 patients with unstable hypoechoic plaque or mobile thrombus, the procedure was delayed, and duplex ultrasonography was repeated after 2 weeks and again after 1 month before proceeding with CAS.
The common femoral artery was used in all patients. Under local anesthesia, a short 10-cm Terumo (Terumo Medical, Tokyo, Japan) 8-Fr sheath was inserted into the common femoral artery, followed immediately by the administration of 5000 international units of heparin. First, a 5-Fr diagnostic catheter Bern (Cordis, Miami Lakes, FL, USA) was used to perform imaging of all arteries, and then an 8-Fr guiding catheter (Mach1 SoftTip; Boston Scientific) was placed in the common carotid artery under continuous heparin infusion. If angioplasty was needed before stenting, then a 2.5 × 20-mm balloon was used, and a 5 × 20-mm balloon was used for post-dilatation angioplasty, with a goal of covering the lesion and achieving residual stenosis of less than 30%. Atropine was kept ready in a syringe for any bradycardia. After the stent was deployed, final imaging of the vessels was performed to exclude distal embolism, and the catheter was removed. Finally, manual compression was applied to the access site for 20–30 minutes to prevent bleeding, and the patient was monitored in the intensive care unit (ICU) overnight for any complications such as bleeding or stroke.
Outcomes measuresNeurological evaluation was performed using the National Institutes of Health Stroke Scale (NIHSS) by a well-trained neurologist just before the procedure, immediately after, and 12 hours later before discharge. Complications associated with CAS (stroke, arrhythmia, hypotension, myocardial infarction, or death) occurring up to 30 days postoperatively were evaluated. Postoperative neuroimaging was ordered for patients who developed periprocedural neurological symptoms, and on day 30, carotid duplex was routinely performed. The CAS procedure was considered successful if the residual stenosis was less than 30%.
Statistical analysisData analyses were conducted using the Statistical Package for the Social Sciences version 23.0 (IBM, Armonk, NY, USA).
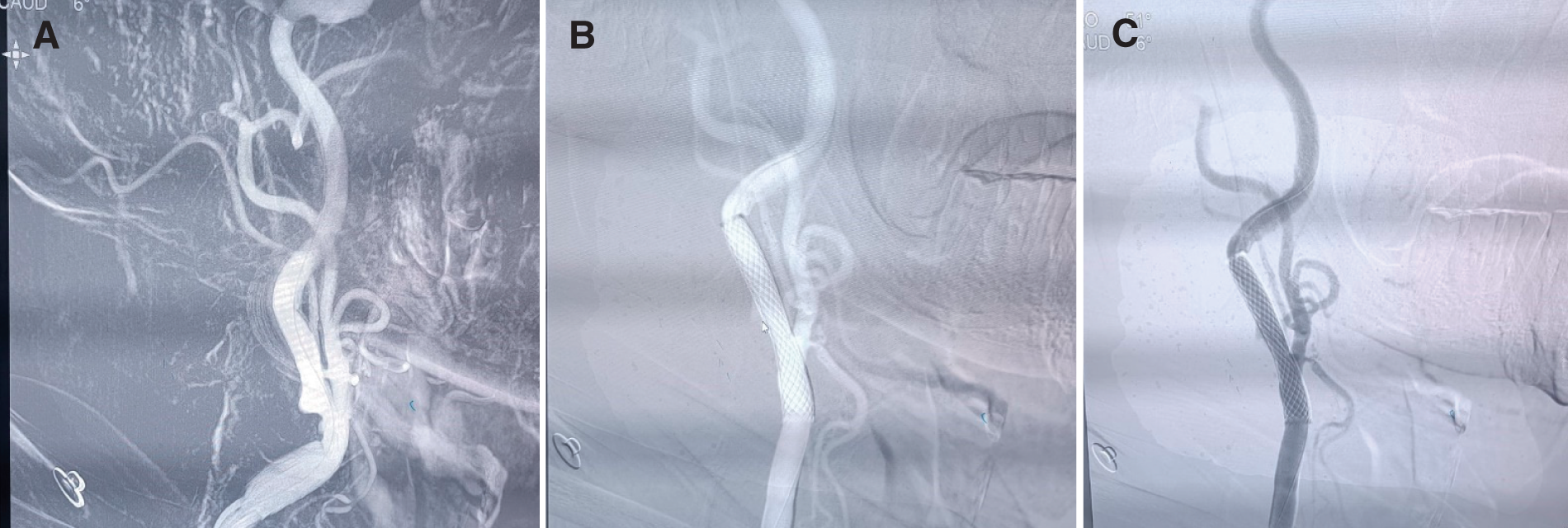
A total of 62 patients were included in this retrospective study. Fifty-three patients were male (85.5%), while 9 were female (14.5%). The mean age of patients was 60.2 ± 9.6 years. All patients were treated successfully with deployment of a single closed-cell stent (Carotid WALLSTENT; Boston Scientific). The site of stent deployment was the left internal carotid artery (ICA) in 43 patients (69.4%) and the right ICA in 19 patients (30.7%). NIHSS before the procedure was 0 in 47%, 3–5 in 34% and 6–9 in 19% of patients. The mean NASCET was 76% ± 10%. Predilation angioplasty was needed in 16 (25.8%) patients and postdilation angioplasty in 58 (93.6%) patients. There were no major complications, including cerebral infarctions. Significant bradycardia occurred in 2 patients and responded immediately to atropine, but no profound hypotension developed in any patient. One patient had transient dysarthria, but diffusion-weighted (DW)-MRI was negative. Three patients developed mild local hematoma, and 1 patient had a pseudoaneurysm. No stroke, myocardial infarction, or in-stent thrombosis was documented during the 30-day follow-up. A summary of the baseline characteristics and risk factors is presented in Table 1, and a case example illustrating a patient with significant right ICA stenosis before and after the procedure is shown in Fig. 1.
| Characteristics | Total no. of patients (62) |
|---|---|
| Age (mean ± SD) | 60.2 ± 9.7 |
| Gender | |
| Male | 53 (85.5%) |
| Female | 9 (14.5%) |
| Symptomatic lesion | All |
| NASCET (% ± SD) | 76% ± 10% |
| Risk factors (%) | |
| DM | 31 (50%) |
| Hypertension | 59 (95.2%) |
| IHD | 34 (54.8%) |
| Dyslipidemia | 57 (91.9%) |
| Smoking | 49 (79%) |
| Khat chewing | 51 (82.6%) |
| Type of stent | Carotid WALLSTENT (100%) |
| EPDs | None |
| Antiplatelets protocol | |
| Aspirin + clopidogrel | 8 (12.9%) |
| Aspirin + ticagrelor | 54 (87.1%) |
Carotid WALLSTENT, Boston Scientific, Marlborough, MA, USA; DM, diabetes mellitus; EPDs, embolic protection devices; IHD, ischemic heart disease; NASCET, North American Symptomatic Carotid Endarterectomy Trial; SD, standard deviation
CAS has emerged as a minimally invasive alternative to CEA for the treatment of carotid artery stenosis, particularly in patients at high surgical risk. This procedure has gained widespread acceptance in high-income countries with advanced medical infrastructure, and in the United States CAS is reimbursed for symptomatic patients with ≥50% carotid stenosis and asymptomatic patients with ≥70% stenosis by the Centers for Medicare & Medicaid Services, which issued a new national coverage determination.14) However, its implementation in resource-limited settings presents unique challenges. These challenges include restricted access to specialized centers, limited availability of trained interventionalists, and financial constraints that hinder the adoption of advanced medical technologies. The use of EPDs and closure systems presents an additional cost challenge, so the feasibility and outcomes of CAS in resource-limited settings remain underexplored, with limited data available to guide clinical practice.
This study evaluates the implementation, challenges, and outcomes of CAS without EPDs in a resource-limited country, focusing on the experience at American Modern Hospital in Aden, Yemen.
The first diagnostic cerebral angiography in Yemen was performed in February 2023, together with the establishment of the first comprehensive stroke center. The most common procedure performed at the center is the CAS. The overall technical success rate was 100% which compares well with the published data.
There are no large-scale or robust studies on the prevalence of extracranial atherosclerosis in Yemeni patients. In a small study conducted at Dhamar University, carotid stenosis was detected in 45 out of 84 patients (54%), while significant stenosis (>60%) was identified in 23 patients (27.4%).15) The predominant risk factors were smoking, hypertension, dyslipidemia, and DM, respectively. Khat chewing is included, as many studies support the association of this habit with cardiovascular diseases and premature atherosclerosis, which could explain the younger mean age of the population in our study.16,17)
The neurointerventionalist’s major concern during the CAS procedure is cerebral embolism. To reduce the incidence of periprocedural embolic stroke, EPDs are recommended (Class IIa, level B), and there are 2 types, distal EPDs and proximal EPDs.18,19,20) However, many studies argue the significance of protected CAS.21,22,23) Some believe that the unprotected techniques may decrease neurological sequelae, especially in tortuous arteries where EPDs can offer extra maneuvring that could lead to embolism, dissection, or vasospasm.24)
The recommendation of EPDs due to higher stroke risk in the unprotected group, such as in the EVA-3S trial, is questioned due to the later incidence of stroke and that the age of the unprotected group was 8 years older.25) The risk of cerebral embolization is present during all stages of CAS: passing the lesion with a wire, pre-dilatation, placement of the protection device, stent deployment, and post-dilatation.26,27)
Closed-cell designed stents can provide better scaffolding to the carotid lesion and hence decrease the danger of plaque extrusion via the interstices of the stent during deployment, post-dilatation, and after finishing the procedure.28) Two previous studies showed a trend of better outcomes with closed-cell stents,29,30) and other studies, such as that by Binning et al.,21) reported no cases of transient ischemic attack, intracranial hemorrhage, or ischemic stroke among 174 patients who underwent unprotected CAS. Similarly, Perona et al.23) observed 6 minor strokes and 3 major strokes (all in patients who had discontinued antiplatelet prophylaxis) among 397 patients included a study of CAS without EPDs. In our study, only 1 patient developed transient dysarthria, and DW-MRI was negative. Possible reasons for the absence of cerebral infarctions in our study, despite performing CAS without EPDs, include the use of direct stenting without pre-dilatation in most of the CAS procedures, the use of a very small and short balloon (2.5 × 20 mm) when pre-dilatation was necessary, and the consistent use of closed-cell stents.
No studies have specifically addressed the cost-effectiveness of CAS in Yemen. However, CAS can be a cost-effective procedure in selected patient populations, particularly when compared to the long-term costs of stroke care. This study highlights the potential of CAS as a viable treatment option for carotid artery stenosis in Yemen despite significant challenges. The clinical outcomes observed in Yemeni patients are comparable to those in other low-resource settings, underscoring the importance of expanding access to this life-saving procedure. However, the success of CAS in Yemen depends on addressing key barriers, including infrastructure limitations, training gaps, and financial constraints.
CAS is a promising intervention for stroke prevention in resource-limited countries, but its widespread adoption requires targeted efforts to overcome systemic challenges. This study underscores the need for further research and investment to ensure equitable access to CAS and to improve outcomes for patients with carotid artery stenosis.
The authors declare that they have no conflicts of interest.