2020 Volume 40 Issue 4 Pages 381-385
2020 Volume 40 Issue 4 Pages 381-385
[Purpose] Cervical intraepithelial neoplasia (CIN) and early cervical cancer are frequently detected in women of reproductive age. The appropriate treatments for these diseases should be selected considering sparing fertility. Of these treatments, photodynamic therapy (PDT) is a minimally invasive therapeutic technique that enables sparing of the cervix and is as effective as cervical conization in terms of treatment results. Talaporfin sodium (NPe6)-mediated PDT was administered intravenously to nine CIN cases. This study aimed to evaluate the effect of PDT and photosensitivity in these cases.
[Methods] PDT was administered to nine patients who were diagnosed with CIN based on cervical cytology, histology, and colposcopy findings. NPe6 was administered intravenously at a dose of 40 mg/m2. Four hours after the administration of NPe6, the patients were exposed to photoradiation (100 J/cm2).
[Results] PDT was used to treat a total of nine patients (two patients with CIN2 and seven patients with CIN3). Cure was confirmed in eight cases who were available for follow up thorough examinations conducted at three and six months after photoradiation. Seven patients exhibited no photosensitivity at day 14 after NPe6 administration. Mild photosensitivity by direct sunlight test was observed in one patient up to day 28.
[Conclusion] This study suggests that NPe6-mediated PDT might be a promising treatment for CIN.
【目的】子宮頸部上皮内腫瘍(cervical intraepithelial neoplasia: CIN)及び初期子宮頸がんは生殖年齢で多く認められる疾患である。それらに対する治療法として妊孕性温存に配慮した治療法の選択が求められる。その中で光線力学的療法(Photodynamic therapy: PDT)は非侵襲的で子宮頸部温存ができ治療成績は円錐切除に劣らない。今回,我々はタラポルフィンナトリウム(NPe6)を用いて9例のCIN症例に対しPDTを行いその治療効果と光線過敏症に対し評価することを目的した。
【方法】CINと診断された9例に対しPDTを施行した。40 mg/m2のNPe6を静脈投与し,光線照射(100 J/cm2)を行った。
【結果】CIN2が2例,CIN3が7例の計9例に対しPDTを施行した。追跡できた8例は照射後3か月後及び6か月後の検査で治癒を認めた。直射日光による皮膚光感受性試験では,1例が投与後28日まで皮膚光感受性を認めた。
【考察】NPe6によるPDTはCINに対する有望な治療法であることが示唆された。
Cervical intraepithelial neoplasia (CIN) and early cervical cancer are frequently detected in women of reproductive age. The appropriate treatment for these diseases is selected in consideration of sparing fertility. Regardless, cervical conization remains the standard treatment for these diseases particularly due to its high diagnostic ability. Other treatment options for CIN include laser vaporization and photodynamic therapy (PDT). However, cervical conization, a surgical procedure for reproductive-age women does also entail some risk. In particular, increased preterm birth rate and a higher intrapartum caesarean section rate are adverse events that are known to occur after cervical conization1-3).
In terms of achieving CIN cure rate, PDT is comparable to cervical conization. PDT is an excellent therapeutic technique that rarely leads to reduction in cervical length or pregnancy-associated adverse events including an increase in miscarriage and preterm birth. Porfimer Sodium (Photofrin) is the drug mainly used for PDT in Japan. Photosensitivity has been reported as an adverse effect of Photofrin. To alleviate photosensitivity, second-generation photosensitizers have been developed and used for the treatment of various types of cancer. Talaporfin sodium (mono-L-aspartyl chlorin e6: NPe6), which belongs to this group of second-generation photosensitizers, is excreted quickly and is less associated with photosensitivity. As therapeutic techniques for treating lung cancer and post-chemoradiotherapy (CRT)-recurrent esophageal cancer, PDT with NPe6 and a PD laser have been reported and used in clinical settings. NPe6 is an effective drug for PDT because of its excellent therapeutic effects and limited adverse effects.
We adopted PDT with NPe6 and a PD laser to treat nine patients with CIN. We report the results of our evaluation of the therapeutic effects and adverse events.
The subjects were female patients aged 20 years or older with no serious complications or photosensitivity who were diagnosed with CIN2 or CIN3 based on cervical cytology and histology findings and whose lesions were confirmed macroscopically by colposcopy. They received a full explanation about the study protocol, which was approved by the ethical committee of the Hamamatsu University School of Medicine (R15-223). Only patients who provided informed consent were included in the study.
2.2 Photosensitizer and Laser EquipmentFour hours after the intravenous administration of NPe6 (40 mg/m2), laser irradiation (100 J/cm2) was applied using PD Laser® (Panasonic). While observing the cervical lesion through colposcopy, the operator irradiated the entire vaginal lesion using the frontal probe. Reduction of the irradiation period was considered, and the irradiation diameter was adjusted to 15 mm. Irradiation was repeated several times to include the lesion in the irradiation area. Thus, to treat an endocervical lesion (20 mm), a radial probe was used for irradiation at a dose of 100 J/cm2.
The doses of NPe6 that were judged to be safe in previous reports on the treatment of lung cancer4) and post-CRT recurrent esophageal cancer5) were considered, and the dose was adjusted to 40 mg/m2 in this study. The photoradiation energy was adjusted to 100 J/cm2 because no serious adverse events were noted in the reports on photoradiation of lesions in the hollow organs such as those associated with lung cancer and esophageal cancer. The safety of photoradiation of a solid tumor at a dose of 100 J/cm2 was confirmed in a phase I study of NPe66), and the uterine cervix is a parenchymal organ.
2.3 ProtocolThe patients were admitted to our hospital one day before PDT. They were administered NPe6 intravenously and underwent photoradiation on their second day in the hospital. They underwent vaginal douching at one, three, five, and seven days after photoradiation. Patients were hospitalized for 14 days after NPe6 intravenous administration and avoided direct sunlight. They were checked for photosensitivity symptoms including reddening and pain. The severity grades of photosensitivity and lower abdominal pain were measured according to the “Common Terminology Criteria for Adverse Events (CTCAE) Version 4.0.” On day 14 after NPe6 administration, they were allowed to cease the shaded period after their photosensitivity check by sunlight. If the skin turned red by sunlight, the patient was examined repeatedly until the red changes disappeared.
To evaluate the treatment effect after PDT, cytology and histology examinations were conducted at three months after therapy. Cytology was further repeated at six months after treatment. A comprehensive pathological judgment was made based upon the results obtained at three and six months after PDT. A case was judged to be a complete response (CR) if negative results were obtained in all of the tests. Some patients may have had residual lesions. In these cases, a judgment of partial response (PR) or no change (NC) was made based upon the results of the pathological examinations of the residual lesions.
Between March 2016 and June 2018, a total of nine patients with CIN were enrolled. The subjects were nine female patients aged 27 to 39 years. They included two patients with CIN2 and seven patients with CIN3. All of their lesions were confirmed by colposcopy and photoradiation was performed. The frequency of photoradiation for the cervix ranged from 10 to 13 times while that of endocervical photoradiation was twice for all cases. The total energy applied by photoradiation ranged from 1200 J to 1500 J. The patients’ characteristics and outcomes are presented in Table 1. In all cases, photoradiation prevented further growth of the lesions. Colposcopy conducted six days after PDT revealed necrosis at the irradiated sites. Colposcopy conducted three and six months after discharge revealed regenerating epithelium only and the eight patients who were available for follow up responded completely to the treatment (CR) as demonstrated by the pathological findings. The changes in the cervical findings obtained in Case 1 are presented in Fig.1.
| Age | G/P | Diagnosis before PDT | 3 Mo after PDT | 6 Mo after PDT | respnce | ||
|---|---|---|---|---|---|---|---|
| cytology | biopsy | cytology | |||||
| Case 1 | 35 | 2/0 | CIN2 | NILM | Neg | NILM | CR |
| Case 2 | 34 | 0/0 | CIN3 | NILM | Neg | NILM | CR |
| Case 3 | 38 | 0/0 | CIN2 | NILM | Neg | NILM | CR |
| Case 4 | 35 | 2/2 | CIN3 | NILM | Neg | NILM | CR |
| Case 5* | 28 | 1/1 | CIN3 | — | — | — | — |
| Case 6 | 37 | 2/1 | CIN3 | NILM | Neg | NILM | CR |
| Case 7 | 39 | 0/0 | CIN3 | NILM | Neg | NILM | CR |
| Case 8 | 26 | 0/0 | CIN3 | NILM | Neg | NILM | CR |
| Case 9 | 31 | 0/0 | CIN3 | NILM | Neg | NILM | CR |
G; gravida, P; parity, CR; complete remission, *; No data was available as it was impossible to follow the patients after discharge.
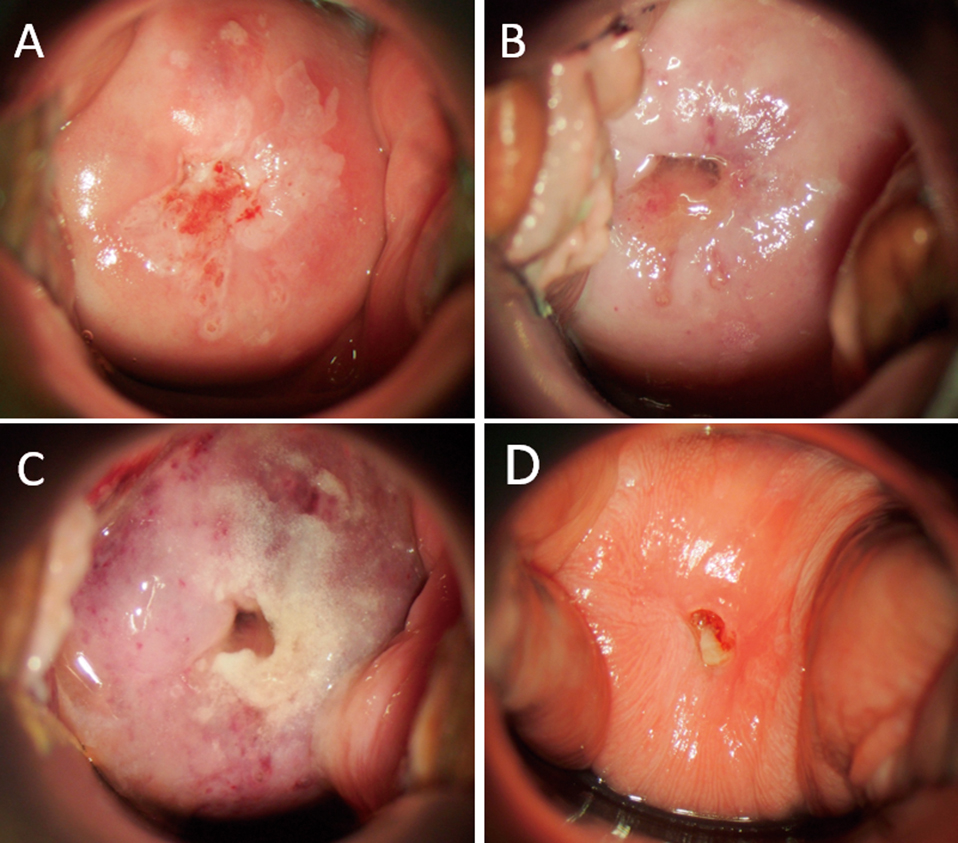
Colposcopic change by NPe6 PDT.
A: CIN2 before PDT. B: Just after photoirradiation. Shutdown effect made the whole cervix appear pale. C: 6 days after PDT. Necrotic tissue was found. D: 3 months after PDT. No acetowhitening area was apparent, but regenerating epithelium was observed.
Three patients complained of Grade 2 pain as an adverse event during photoradiation (Table 2). Three additional patients complained of Grade 1 lower abdominal pain. Only one patient complained of reddening over the back of the hand as a symptom of Grade 2 photosensitivity six days after PDT. This symptom improved in one day after clobetasone butyrate topical application. Eight of nine patients who underwent sunlight test 14 days after NPe6 administration showed no symptoms of photosensitivity including reddening. In one patient, we confirmed redness up to day 28 on the dorsum of her foot as a symptom of mild photosensitivity by direct sunlight.
| Grade | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| Photosensitivity | 1 | 1 | 0 | 0 | 0 |
| Lower abdominal pain | 3 | 3 | 0 | 0 | 0 |
Severity grade of photosensitivity and lower abdominal pain were measured according to the “Common Terminology Criteria for Adverse Events (CTCAE) Version 4.0”.
We adopted PDT using NPe6 and PD Laser® to treat nine patients with CIN. Because the response to the PDT was judged to be CR in eight cases with adequate follow up, this therapeutic technique was considered effective. Although the patients complained of mild pain during and after PDT, all of them completed therapy and few patients complained of photosensitivity. Accordingly, PDT was considered as a safe therapy that caused minimal adverse events. Eight patients, except one, did not show photosensitivity even when exposed to direct sunlight 14 days after NPe6 administration.
CR was recorded for eight of the patients who were available for follow up after undergoing NPe6-mediated PDT. Among those who underwent Photofrin-mediated PDT, the CIN cure rate was approximately 95%. Therefore, the therapeutic effect of NPe6-mediated PDT appeared to be comparable to that of Photofrin-mediated PDT. In this pilot study, only eight subjects were examined completely but CR was confirmed in all of the cases available for follow up. Moreover, eight of nine patients were able to be exposed to direct sunlight 14 days after NPe6 administration. Therefore, NPe6-mediated PDT is considered an effective therapeutic approach.
After NPe6-mediated PDT, elimination of further cell growth was consistently observed in all lesions exposed to photoradiation and thus, photoradiation could be applied without fail. This effect of NPe6 is considered as a phenomenon that enables the operator to macroscopically confirm damage to the feeding vessels of a tumor that occurs concomitant with cellular damage. Compared with Photofrin, NPe6 exerted this effect more markedly and the operator could clearly confirm whether or not photoradiation was applied. Because of this effect, NPe6-mediated PDT is expected to exert a beneficial effect that is not dependent on the skill of the operator.
In this study, PD Laser® was used to deliver photoradiation to a location 15 mm in diameter. In Photofrin-mediated PDT using EDL-1, the irradiation diameter is 10 mm. However, one session of radiation with PD Laser® requires approximately 11 minutes. For this reason, a larger irradiation diameter is needed. Because the irradiation diameter was adjusted to 15 mm in our study, the total photoradiation period was approximately two hours. This adjustment likely contributed to the alleviation of the patients’ stress.
Adverse events were reported in the current study. During PDT, three patients complained of Grade 2 pain. Moreover, immediately after PDT, three patients complained of Grade 1 pain, although, none of them required discontinuation of the PDT. This pain was likely to be due to the above-mentioned effect on cellular growth, leading to ischemia that might cause pain. After photoradiation, an analgesic was administered and the pain disappeared immediately. Therefore, these episodes of pain were considered as minor adverse events.
Another adverse event of concern was photosensitivity. One patient (11.1%) complained of mild reddening over the back of the hand six days after PDT under management of indoor illumination 200 lux. This symptom improved by clobetasone butyrate topical application in one day. There were no complaints of photosensitivity during the subsequent shading period in the other 8 cases. Previously, Kato et al. reported that photosensitivity, a side effect of Photofrin, occurred in 20.3% of patients7). On the other hand, photosensitivity due to NPe6 is reported to occur in 7.4% of patients8). We compared NPe6 with Photofrin and found that NPe6 was a safe photosensitizer. Although the patients were exposed to direct sunlight by photosensitivity test 14 days after the NPe6 administration, eight out of nine patients did not complain of any symptoms related to photosensitivity.
PDT is a minimally invasive tumor cell-targeting therapy in which combination of a photosensitive substance with tumor affinity and low-output laser irradiation minimizes injury to normal tissues. Many studies using this method have been performed since Dougherty et al. first applied PDT to epithelial cancer in 19789). However, despite being minimally invasive, PDT is used less frequently than surgical treatment because systemic photofrin administration can lead to severe adverse effects due to light hypersensitivity. Treatment of uterine cervical intraepithelial neoplasia (CIN) in the field of obstetrics and gynecology provides one relevant example. The incidence of CIN has increased in young women and conservation of fecundity is essential for these patients in which conization is widely used. However, this procedure has an increased risk of complications such as cervical stenosis which may induce postoperative hemorrhage and cervical incompetency leading to premature birth and low-birth-weight infants1-3).
PDT has been investigated using second-generation photosensitizers. Photodynamic diagnosis and PDT with local administration of photosensitizer precursors such as 5-aminolevulinic acid (5-ALA) have also been reported. HAL prepared by esterification of 5-ALA has been approved for fluorescence cystoscopy to detect urinary bladder cancer and intraepithelial cancer in Europe. Photodiagnosis using porphyrin fluorescence emitted by 5-ALA to identify CIN lesions is considered superior to that of general colposcopy10). However, the results of PDT for CIN remain unclear11). Hillemanns et al. have shown that locally administered HAL reaches the basement membrane of CIN lesions since esterification of 5-ALA increases its lipid permeability. In the treatment of CIN using PDT with local administration of HAL, the response rate is 64% whereas that with PDT using intravenous Photofrin administration is about 95%12,13). Istomin et al. reported PDT using Photolon, which is virtually identical to Talaporfin sodium14). The therapeutic effect of PDT using Photolon was 92.9% and was considered the most promising among the second-generation photosensitizer.
We used NPe6 and PD Laser® for PDT in patients with CIN. CR was achieved in all patients who with adequate follow up. Although the patients suffered from mild photosensitivity, they were able to undergo treatment without serious adverse events which exceeded Grade 2 toxicity. Due to this advantage, NPe6-mediated PDT is considered a useful therapeutic approach. The accumulation of more cases will be necessary before further examinations can be conducted. To validate the therapeutic effects and efficacy of NPe6-mediated PDT, we will need to compare this approach with cervical conization.
There is no conflict of interest (COI) to disclose related to this paper.