2017 年 5 巻 1 号 p. 7-12
2017 年 5 巻 1 号 p. 7-12
Aim: This study aimed to clarify the appropriate management of hypertensive disorders of pregnancy (HDP) and establish a long-term follow-up system for women with HDP after delivery. We investigated issues relating to HDP management approaches by evaluating blood pressure measurement at the time of medical examination, home blood pressure measurement (HBPM) penetration rate, timing of blood pressure measurement during labor, and follow-up procedures after delivery in women with HDP.
Methods: We distributed questionnaire forms on blood pressure management during pregnancy, at delivery, and after delivery to obstetrics and gynecology departments of 52 professional medical institutions in Aomori prefecture, Japan, in 2013.
Results: We retrieved completed questionnaires from 52 institutions and analyzed responses from 39 institutions. Some institutions responded that antihypertensive medication was administered for mild hypertension (140/90 mmHg); these institutions had a lower target blood pressure. Only 56% of institutions measured blood pressure after the onset of labor pains. Postpartum follow-up was carried out not only by obstetric and gynecologic clinics, but also by many institutions. However, sufficient education on the risk of recurrence in subsequent pregnancy and lifestyle guidance were not provided.
Conclusions: There is little consensus on the timing of initiating antihypertensive medication, or appropriate levels of blood pressure control. Labor-onset hypertension might have been overlooked. Short-term follow-up of women with HDP was frequently carried out, whereas long-term follow-up was not. We will continue to investigate the appropriate follow-up duration and approach for women with a history of HDP and proactively engage in lifestyle interventions with the aim of improving longevity.
Hypertensive disorders of pregnancy (HDP) is defined as hypertension with or without proteinuria emerging after 20 weeks of gestation, but resolving up to 12 weeks postpartum, and are also defined as new onset proteinuria in hypertensive women who exhibit no proteinuria before 20 weeks of gestation. There are four classifications of HDP: gestational hypertension (GH), preeclampsia (PE), superimposed preeclampsia, and eclampsia.1)
As HDP adversely affects maternal and fetal health in 3–5% of all pregnancies, it must be carefully managed.2) The recurrence rate of HDP is high, and PE during the first pregnancy increases the risk of recurrence in future pregnancies by 6.6-fold compared with that of a normotensive individual.3) Moreover, a high proportion of women who experience HDP develop cardiovascular disease later in life.4,5,6,7,8,9,10,11,12,13,14) However, there are no established long-term follow-up systems for women with HDP.
In the present study, we aimed to clarify the appropriate management of HDP during pregnancy and establish a long-term follow-up system for women with HDP after delivery. We investigated problems related to HDP management approaches in Aomori prefecture, Japan, by evaluating the following clinical variables: blood pressure measurement at the time of medical examination, home blood pressure measurement (HBPM) penetration rate, timing of blood pressure measurement during labor, and follow-up procedure after delivery in women with HDP.
A total of 9,126 births occurred in 2013 in Aomori prefecture, where there are 52 obstetrics and gynecology institutions. In 2013, we distributed questionnaire forms on blood pressure management during pregnancy, at delivery, and after delivery to these 52 institutions (29 institutions perform deliveries, and 23 do not), with a response period of one month. In 2014, an HDP follow-up outpatient clinic was set up at our hospital in consideration of these concerns.
We retrieved completed questionnaire forms from all 52 institutions. Of these, responses from 39 institutions were analyzed. The questionnaire consisted of the following components:
Blood pressure measurement at the time of medical examination (1) Who measures blood pressure? (multiple choice)Response rates for institutions that perform deliveries were as follows: physician, 1 patient; midwife, 13; nurse, 16, and automatic sphygmomanometer, 19. Response rates for institutions that do not perform deliveries were as follows: physician, 1; midwife, 2; nurse, 8; and automatic sphygmomanometer, 3.
(2) How do you assess blood pressure measurements in Maternity Health Record Books?Response rates for institutions that perform deliveries were as follows: first time blood pressure, 8 (28%); second time blood pressure, 1 (3%); stable blood pressure, 10 (34.5%); and all results, 10 (34.5%). None of the institutions provided an average value. Response rates for institutions that do not perform deliveries were as follows: first time blood pressure, 2 (8.7%); stable blood pressure, 8 (34.8%); and all results, 13 (56.5%).
Home blood pressure measurement (HBPM) (1) Do you recommend HBPM to pregnant women?Response rates for institutions that perform deliveries were as follows: ‘Yes,’ 28 (97%); and ‘No,’ 1 (3%). Response rates for institutions that do not perform deliveries were as follows: ‘Yes,’ 4 (80%); and ‘No,’ 1 (20%).
(2) In what cases do you recommend HBPM?Response rates for institutions that perform deliveries were as follows: high blood pressure on medical examination, 26 (32%); chronic hypertension, 23 (28%); risk of HDP, 13 (16%); and past history of HDP, 19 (24%). Response rates for institutions that do not perform deliveries were as follows: high blood pressure on medical examination, 8 (38%); chronic hypertension, 8 (38%); risk of HDP, 4 (19%); and past history of HDP, 3 (14%).
(3) When do you recommend performing HBPM?Response rates for institutions that perform deliveries were as follows: in the morning, 2 (8%); in the morning and evening, 18 (75%); and at other times, 4 (17%). Response rates for institutions that do not perform deliveries were as follows: all responded that HBPM should be performed in the morning and evening.
Figure 1 shows when to recommend to patient to come to the clinic or hospital after instructions of HBPM. Figure 2 shows the blood pressure level at which antihypertensive medication was prescribed. Figure 3 shows the target blood pressure values according to institution.

BP level at which revisiting the clinic or hospital.

BP level at which antihypertensive medication was prescribed.

Target BP values according to institution.
Response rates were as follows: in all cases, 19 institutions (56%); in cases with high blood pressure at admission, 3 (9%); in high-risk cases, 5 (15%); and at the discretion of the staff, 7 (20%).
(2) Does the staff report measured blood pressure values to physicians?Response rates were as follows: in all cases, 3 (10%); in cases with blood pressure above 140/90 mmHg, 16 (55%); and at the discretion of the staff, 10 (35%).
Follow-up after deliveryFigure 4 shows follow-up blood pressure over 140/90 mmHg at one month after delivery.

Follow-up procedure for BP over 140/90 after 1-month check-up following delivery.
Blood pressure measurements were performed multiple times, regardless of whether the institution performed deliveries, until blood pressure was considered to have stabilized in over 50% of cases, and values were recorded in Maternity Health Record Books. However, no institution measured blood pressure twice and used the mean value, as stipulated in HDP guidelines.1)
Pregnant women may be referred to other institutions, return home to give birth, or undergo examinations at more than one clinic. Therefore, it is necessary to confirm whether sphygmomanometers used at each institution conform to standards, and that consistency is achieved in measurement methods, devices used, number of measurements, and frequency of recording blood pressure in Maternity Health Record Books.
2. Home blood pressure measurement (HBPM)Institutions should individually decide on criteria for reporting home blood pressure values to physicians. Pregnant women should be instructed to consult their physicians if the mean blood pressure value over several days exceeds 135/85 mmHg, if the measured value exceeds 140/90 mmHg twice in succession, or if a single measured value exceeds 160/110 mmHg. According to our survey, HBPM was encouraged by most of the participating institutions, suggesting that it may contribute to the early detection of HDP. Most institutions recommended HBPM if blood pressure was high at the hospital or if hypertensive complications of pregnancy were present, while some institutions also recommended HBPM if patients had a risk or history of HDP. Our results suggest that the methods and devices used to measure blood pressure should be unified. Although there was wide variation, in most cases, home blood pressure values that medical institutions recommended for reporting were 140/90 mmHg or higher. However, while some institutions set a cut-off value of blood pressure at 160/100 mmHg or higher, others did not set a particular value, suggesting the need for medical professionals to recognize the significance of HBPM. Medical professionals need to be aware of the fact that blood pressure not only exhibits diurnal, intraday, intraweek, and seasonal variations, but also varies according to the number of weeks of gestation;15,16) they must give patients numerical values.
3. Antihypertensive medicationAn excessive drop in blood pressure may cause non-reassuring fetal status and ischemia of the maternal central nervous system and other major organs. Therefore, adjustable hypotensive agents should be used under strict management.17) Acute hypertension (≥180/120 mmHg) may lead to eclamptic seizures, cerebral stroke, and other conditions that may cause maternal mortality, requiring immediate hypotensive treatment.18)
In the present survey, most institutions responded that hypotensive treatment was initiated if blood pressure was roughly 160/100 mmHg. However, some institutions perform hypotensive treatment for mild hypertension (around 140/90 mmHg), while others set the target for hypotension even lower. These approaches may result in excessive blood pressure reduction.
4. During deliveryRecently, labor-onset hypertension (LOH) has become a new disease concept. LOH is defined as hypertension that develops after the onset of labor in patients who are normotensive throughout pregnancy. LOH might contribute to the risk of eclampsia or stroke during labor.18) Only 56% of institutions reportedly measure blood pressure after the onset of labor pains; thus, the potential to overlook LOH is a concern. Our results suggest that criteria for reporting blood pressure values to physicians must be clarified at each institution.
5. Follow-up after deliveryPatients who have developed HDP previously have a high probability of recurrence during a subsequent pregnancy, with an approximately 6.6-fold greater risk of experiencing HDP again.3) Body mass index (BMI) immediately before pregnancy and weight gain during pregnancy are major contributors to the risk of HDP recurrence in a subsequent pregnancy, and some studies reported that reducing BMI decreases recurrence rates.19,20,21,22) It is thus important to explain this risk to patients and to provide them with appropriate exercise and diet guidance. Recent reports show that women with a history of HDP are more likely to develop conditions such as hypertension, cerebrovascular disorders, metabolic syndrome, and kidney disease during middle age and in later life.4,5,6,7,8,9,10,11,12,13,14) Thus, follow-up of patients with HDP is necessary from the standpoint of women’s healthcare, although there is no unified consensus on optimal follow-up methods, as evidenced by the 2014 Guidelines for Obstetrical Practice in Japan and the 2014 Guidelines for the Management of Hypertension. The Best Practice Guide 2015 For Care and Treatment of Hypertension in Pregnancy recommends providing guidance on lifestyle after delivery, but does not include details on the optimal follow-up policy.1) In addition, there are no specific descriptions of long-term HDP follow-up in the American Congress of Obstetricians and Gynecologists (ACOG), National Institute for Health and Care Excellence (NICE), and World Health Organization (WHO) guidelines.23,24,25,26)
Some studies have suggested that providing guidance on exercise therapy, dietary restrictions, and smoking cessation to women with a history of HDP reduces the risk of cardiovascular disease (CVD) development.22) Therefore, among general practitioners in the United Kingdom, providing lifestyle guidance to patients is encouraged.27)
In this study, we found that postpartum follow-up was carried out not only by obstetrics and gynecologic clinics, but also by many institutions (including the introduction to internal medicine clinics). However, sufficient education on the risk of recurrence in a subsequent pregnancy and lifestyle guidance were not provided. A uniform follow-up policy that takes into consideration both subsequent pregnancy and long-term prognosis should be formulated. Because most patients who experienced HDP do not subsequently exhibit symptoms, patient education is important for avoiding dropouts during follow-up.
Residents of Aomori prefecture are known to have the shortest lifespan in Japan, and three in four people die from lifestyle-related diseases
(URL: http://www.pref.aomori.lg.jp/soshiki/kenko/ganseikatsu/files/dai4.pdf). The prevention of lifestyle-related diseases is essential for improving longevity in this prefecture, and follow-up of women with a history of HDP may contribute toward that end as well.
In 2014, we set up an HDP follow-up outpatient clinic at our hospital in consideration of these concerns. In practical terms, the names of patients with HDP are included in a list and, even if they are normotensive at the one-month post-birth health checkup, they are asked to schedule a follow-up clinic visit annually at around their child’s birthday (Figure 5). At their appointment, blood pressure and weight are measured, and dietary guidance is provided; blood samples are also collected. Additionally, cervical cancer screening and ovarian ultrasound can be performed upon request. Patients are sent an appointment confirmation card one month prior to their appointment to avoid dropouts and no-shows.
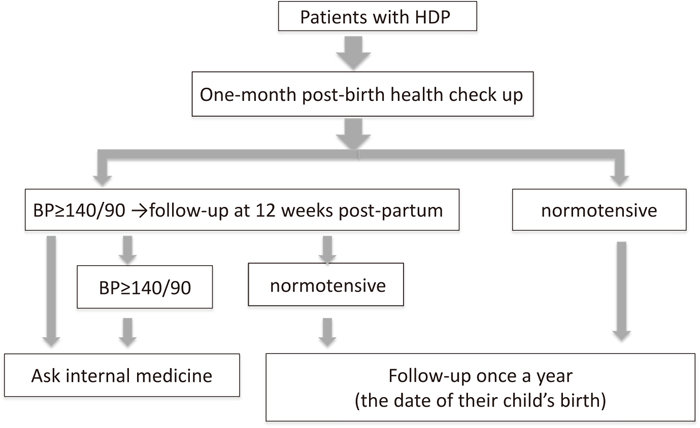
HDP follow-up system.
In the present study, blood pressure might have been lowered excessively as a result of institutional guidelines for initiating hypotensive treatment, and thus, there is a possibility that LOH had been overlooked.
In conclusion, we found that short-term follow-up of women with HDP was frequently carried out, whereas long-term follow-up was not. We will continue to investigate the appropriate follow-up duration and approach for women with a history of HDP and proactively engage in lifestyle interventions with the aim of improving longevity.
None.