2023 年 10 巻 p. 125-130
2023 年 10 巻 p. 125-130
Patients with neurofibromatosis type 1 not only have characteristic skin findings but are also known to have vascular disorders due to vascular vulnerability. A 44-year-old man with previously undiagnosed neurofibromatosis type 1 was brought to the emergency room due to a sudden subcutaneous hematoma with no history of trauma. Angiography revealed extravasation from the parietal branch of the right superficial temporal artery, which was embolized with n-butyl-2-cyanoacrylate. However, the next day, the patient exhibited an increased subcutaneous hematoma, and new extravascular leakage was detected at the frontal branch of the superficial temporal artery, which was also embolized with n-butyl-2-cyanoacrylate. The patient had physical findings characteristic of neurofibromatosis type 1, such as café-au-lait spots, and was subsequently diagnosed with neurofibromatosis type 1. No obvious neurofibroma or any other subcutaneous lesion associated with neurofibromatosis type 1 was identified in the affected area. Massive idiopathic arterial bleeding in the scalp, although infrequent, can be fatal. Neurofibromatosis type 1 should be considered when a subcutaneous scalp hematoma is observed without a history of trauma, even if the facial skin structure appears normal. Neurofibromatosis type 1 is also known to have multiple sources of hemorrhage. Thus, it is important to repeatedly evaluate vascular structures via cerebral angiography, contrast-enhanced computed tomography, and magnetic resonance imaging, if necessary.
Neurofibromatosis type 1 (NF1) presents with cutaneous findings such as neurofibromas, café-au-lait spots, and freckling. NF1, which has an autosomal dominant inheritance, may also present with systemic complications, such as optic gliomas, iris nodules, and bony deformities.1) Vascular disorders have been associated with NF1 in 0.4%-6.4% of patients. These disorders systemically occur from the proximal aorta to the small arteries and are associated with vascular vulnerability.1) This report describes repeated idiopathic rupture of a superficial temporal artery (STA) pseudoaneurysm associated with NF1 that was successfully treated with endovascular therapy. Only a few such cases are reported in the literature.
A 44-year-old man with no known personal or family history of NF1 had sudden-onset right temporal swelling without trauma, which progressed over time. Upon arrival at our institution, a 10-cm subcutaneous anterolateral temporal hematoma and more than six café-au-lait spots were observed on the trunk. The blood test results indicated no coagulation abnormalities. Head computed tomography (CT) revealed a right zygomatic arch defect (Fig. 1A), atrophy of the masticatory muscles (Fig. 1B), and extravasation from the STA within the subcutaneous hematoma (Fig. 1C, D); consequently, endovascular treatment was chosen.
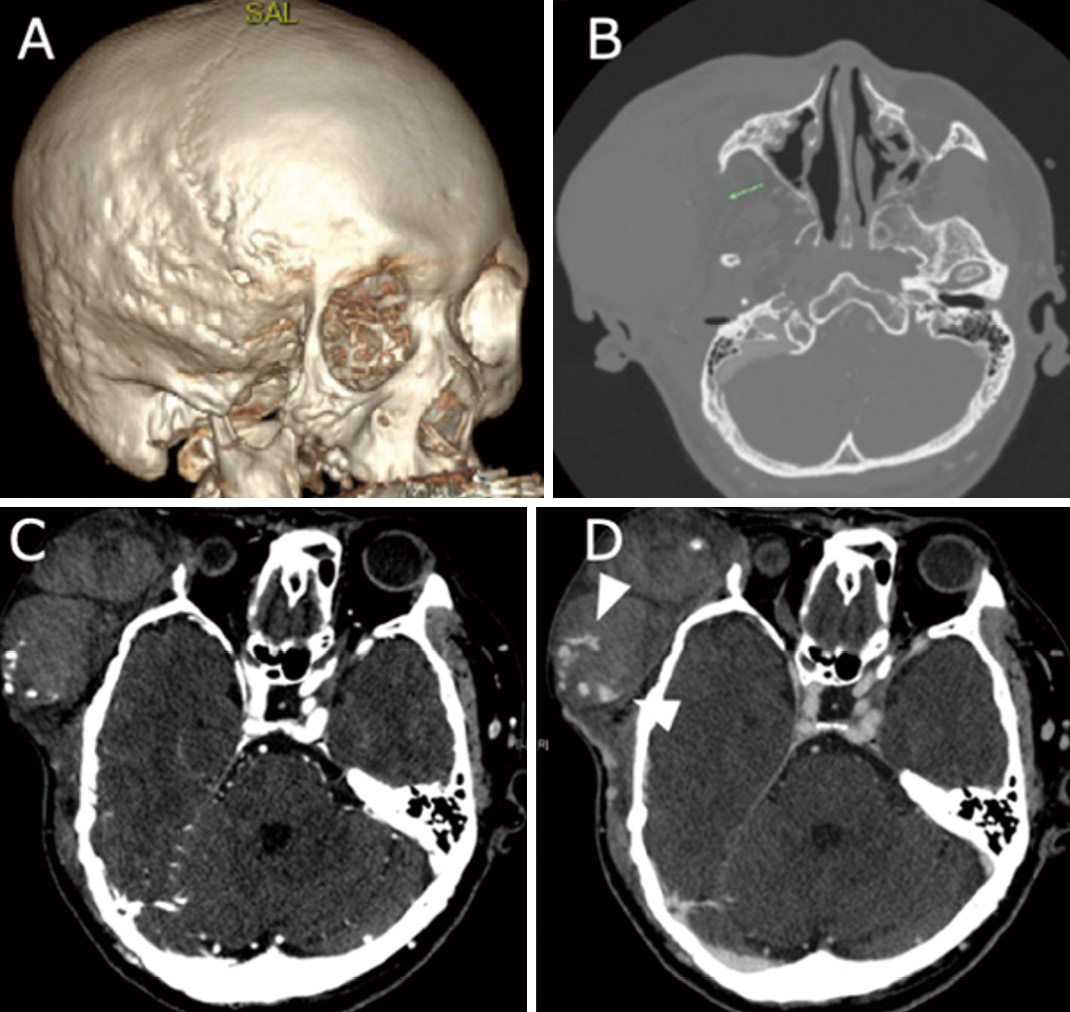
Contrast CT showing (A) right zygomatic arch defect, (B) atrophy of the right masticatory muscle, (C) arterial phase, and (D) venous phase. Extravascular leakage (arrowhead) from the right STA is noted. CT, computed tomography; STA, superficial temporal artery
After puncturing the right femoral artery under local anesthesia, a 6-Fr guiding catheter was placed in the proximal right external carotid artery. A distal access catheter and a microcatheter were guided to the right STA. A pseudoaneurysm was observed in the parietal branch of the right STA (Fig. 2A, B). A microcatheter was distally guided to the rupture site, and the distal segment was embolized with two coils (Fig. 2C). Subsequently, the segment including the aneurysm was obliterated with n-butyl-2-cyanoacrylate (NBCA) (Fig. 2D). At the end of the procedure, we embolized the proximal segment of the artery with coils due to the potential arterial stretch injury related to the massive hematoma (Fig. 2E).

Cerebral angiography was performed on the (A) frontal, (B) lateral, and extravascular leakage in the right STA parietal branch. (C) Coil embolization distal to the bleeding site, (D) NBCA administration, and (E) coil embolization of the proximal side were observed on angiography. NBCA, n-butyl-2-cyanoacrylate; STA, superficial temporal artery
However, we observed an enlarged subcutaneous hematoma on postoperative day 1 and confirmed a new extravascular leak by CT (Fig. 3A, B). Angiography was performed, and the already embolized parietal branch of the STA was occluded. Furthermore, the frontal branch of the STA was confirmed to be bleeding, which was not observed in the digital subtraction angiography performed the previous day (Fig. 3C, D). Microcatheter guidance to the bleeding branch was difficult. Accordingly, the frontal branch distal to the bleeding site was coil embolized (Fig. 3E), and subsequently, the NBCA was proximally injected, which successfully reached the affected branch and blocked blood flow to the bleeding location (Fig. 3F). The patient had no further bleeding and was discharged. NF1 was subsequently diagnosed based on characteristic physical findings, such as café-au-lait spots and zygomatic arch defects, at an outpatient clinic.
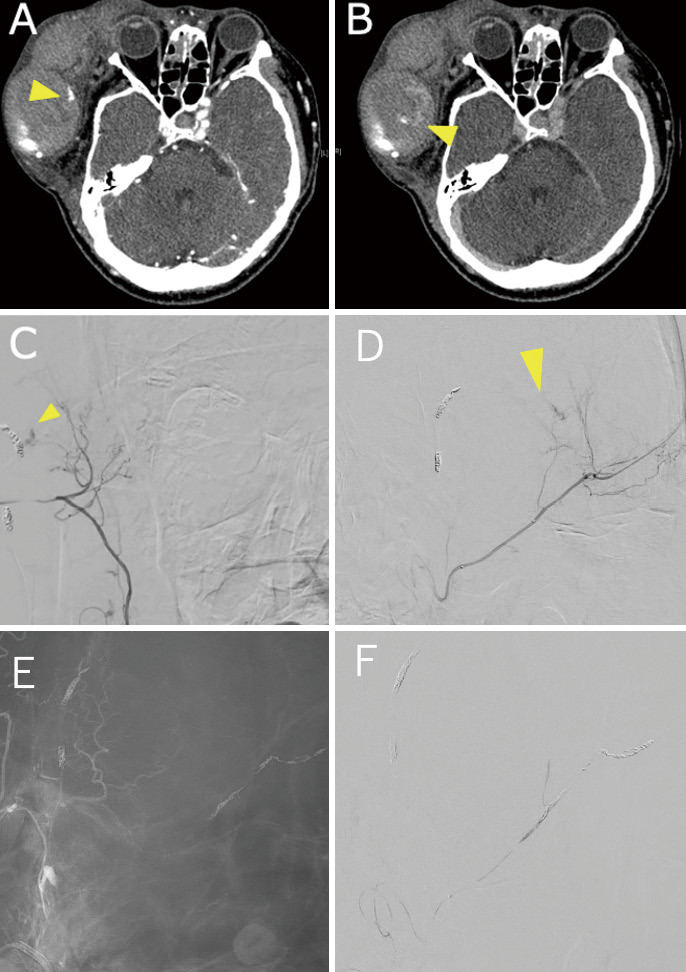
A new extravascular leakage anterior to the site of the previous hemorrhage is shown by (A) arterial and (B) venous phase contrast CT. Cerebral angiography of the (C) frontal and (D) lateral views are also shown, revealing the new extravascular leakage at the right STA frontal branch. (E) Coil embolization distal to the bleeding branch of the frontal branch and (F) NBCA embolization proximal to the bleed were performed. CT, computed tomography; NBCA, n-butyl-2-cyanoacrylate; STA, superficial temporal artery
Several theories exist regarding the mechanism by which vascular fragility occurs in patients with NF1. Pathologically, vascular fragility results from the direct infiltration of the neurofibroma into the vascular intima or is caused by other causes such as compression of the vascular nutrient vessels by neurofibromas and weakness of the endoplasmic plate due to the proliferation of spindle-shaped cells in the intima.2) Vascular lesions of the head and neck associated with NF1 include occlusive cerebrovascular disease.2) Other reported cases include aneurysms, arterial stenosis, arterial dissection, and arteriovenous fistulas, all of which are rare.3) Idiopathic arterial bleeding in the scalp is infrequent and can be fatal.4) Eight cases of severe subcutaneous hemorrhage in the craniofacial region have been reported,5-9) and all were associated with obvious neurofibromas of the scalp, plexiform neurofibromas, schwannomas, and other tumors.5-8,10) However, there are no reports of severe bleeding from normal facial subcutaneous tissue, as in this case. Some may assume an association of the zygomatic arch defect with bleeding. However, the enhanced magnetic resonance (MR) images and physical examination did not reveal any neurofibromas or tumors in the affected region. The defect could also be considered characteristic of bone dysplasia associated with NF-1.11) The massive subcutaneous bleeding in the present case could rather be associated with the systemic vascular fragility described in the literature.1)
Furthermore, our case had distinctive features as follows: First, the patient did not have extravascular leakage from the second hemorrhage site at the initial transcatheter arterial embolization. The frontal branch of the STA, the site of the second hemorrhage, was poorly delineated on preoperative 3D-CTA due to the thickness of the hematoma (Fig. 4A-C). Thus, it is possible that the latent hemorrhage was temporarily stopped by pressure from the hematoma from the other bleeding site and became apparent after the initial treatment. In addition, we believe that the vessel wall of the second bleeding site was stretched by the initial subcutaneous hematoma and collapsed.
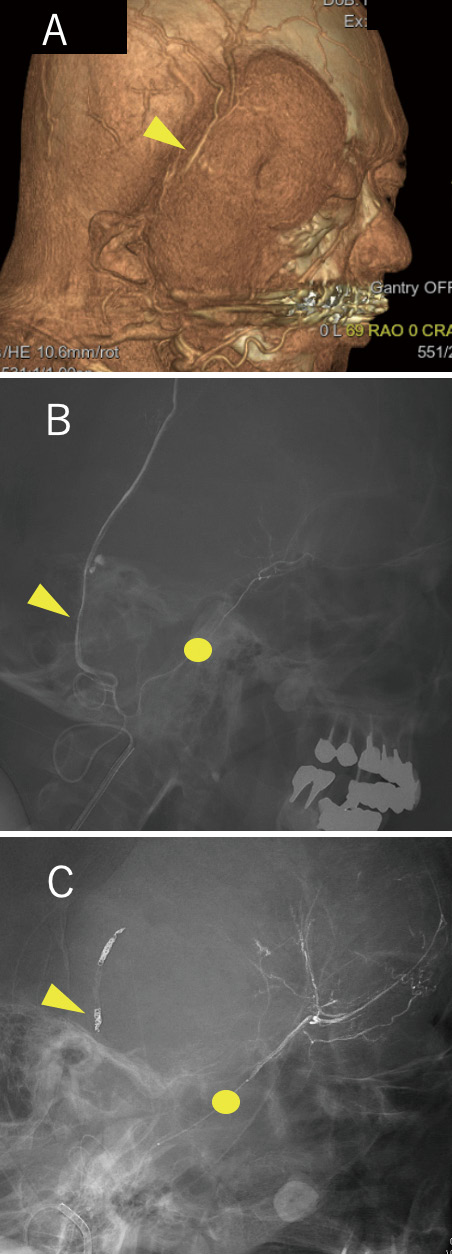
(A) 3D-CTA before the first treatment shows the parietal branch of the STA, the source of bleeding; however, the frontal branch was just below the thick hematoma and was poorly delineated. (B) Cerebral angiography at the first treatment showed the parietal branch of the STA as the source of bleeding; however, bleeding from the frontal branch of the STA could not be confirmed. (C) Cerebral angiography at the second treatment confirmed bleeding from the frontal branch of the STA. CTA, computed tomography angiography; STA, superficial temporal artery
Second, the patient had been diagnosed with NF1, with the current episode as momentum. Patients with NF1 often have characteristic cutaneous findings that may be overlooked in an emergency setting. NF1 should be considered when percutaneous bleeding is observed, particularly from multiple sites, in the absence of trauma. The characteristic bone dysplasia, as observed in the current case, would be a diagnostic clue.
Surgical treatment of NF1 is challenging due to vascular fragility, suturing difficulty, and bleeding.10) Endovascular therapy, however, allows immediate assessment of vascular architecture and prompt treatment. When scalp hematoma extends into the neck, there is a risk of airway obstruction. Endovascular therapy can provide rapid and reliable treatment. Regarding the embolization technique, embolization of the distal portion with a coil and proximal short segment embolization with NBCA are considered safe and reliable methods for reducing the risk of distal NBCA migration leading to skin damage. However, evaluation of the potential anastomosis with the ophthalmic and internal carotid or any intramural arteries in advance is essential.
In conclusion, NF1 should be considered in patients presenting with a sudden subcutaneous hematoma with no history of trauma. Investigation of the presence of characteristic skin and bone findings is also important. Even if bleeding appears to stop at one site, the possibility of bleeding elsewhere exists due to vascular fragility. Therefore, repeated evaluation of the vascular structures with cerebral angiography, contrast-enhanced CT, and MR imaging is important. Accumulation of atypical cases such as ours will increase awareness of NF1 and contribute to future clinical management.
CT computed tomography
NBCA n-butyl-2-cyanoacrylate
NF1 neurofibromatosis type 1
STA superficial temporal artery
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
All authors have no conflict of interest.