2024 Volume 11 Pages 243-247
2024 Volume 11 Pages 243-247
Neurosarcoidosis is a condition that is characterized by the occurrence of noncaseating epithelioid granulomas in various organs throughout the body, including the lungs, heart, and central nervous system. It is particularly prevalent in cases of noncommunicating hydrocephalus. While its clinical presentations may vary, neurological deficits such as hemiparesis are extremely uncommon. We herein present a case of unilateral hydrocephalus resulting from neurosarcoidosis presenting with hemiparesis. A 58-year-old woman exhibited right hemiparesis, altered mental status, and aphasia persisting for 1 month. Magnetic resonance imaging showed unilateral hydrocephalus of uncertain etiology. The patient underwent external ventricular drainage, endoscopic fenestration of the septum pellucidum (septostomy), and lesion biopsy, which led to a histopathological diagnosis. Hemiparesis can accompany unilateral hydrocephalus caused by neurosarcoidosis. Endoscopic procedures provide an effective option for the diagnosis and treatment of noncommunicating hydrocephalus caused by neurosarcoidosis.
Sarcoidosis is an autoinflammatory disorder known to involve various organ systems.1) While it commonly affects the lung, skin, liver, eyes, and lymph nodes, it rarely affects the central or peripheral nervous system, accounting for only 5% of the total cases of systemic sarcoidosis. A retrospective study and a systematic review have indicated that hydrocephalus is present in 9% of patients with neurosarcoidosis.2,3) An unusual presentation, such as acute unilateral hydrocephalus leading to hemiparesis, is exceptionally rare and poses diagnostic challenges. To our knowledge, reports on hemiparesis caused by neurosarcoidosis accompanied by unilateral hydrocephalus and on the effectiveness of endoscopic surgery as a diagnostic and treatment option are scarce.
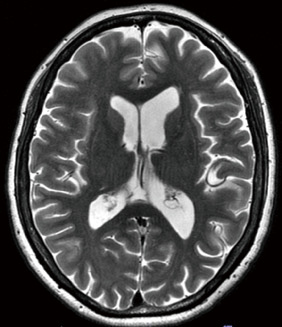
A 58-year-old Japanese woman with diabetes mellitus and hypertension was referred to our hospital due to progressive disturbances of consciousness, mild weakness of the right upper and lower limbs, and difficulty of speech for 3 weeks. She had been experiencing incoherent speech in the preceding month and difficulties to accomplish her job. On admission, her Glasgow Coma Scale score was 14[E (4) V (4) M (6) ], and she exhibited mild right hemiparesis (manual muscle test: 4/5) and transcortical aphasia. Barre's sign on the right side was positive, and mildly elevated deep tendon reflexes were observed. Brain magnetic resonance imaging (MRI) revealed enlargement of the left lateral ventricle and periventricular hyperintensity on T2-weighted imaging (Fig. 1A). There was no obvious mass lesion or leptomeningeal enhancement on gadolinium-enhanced T1-weighted imaging (Fig. 1B). Furthermore, no apparent lesions were found on heavily T2-weighted imaging during that emergency situation (Fig. 1C). Chest radiography revealed no evidence of a mass lesion or hilar lymphadenopathy. No abnormalities were observed in the serum levels of angiotensin-converting enzyme (ACE) or soluble Interleukin 2 receptor (sIL-2R). Considering the clinical course, urgent external ventricular drainage (EVD) and septostomy with endoscopy were planned. Retrospectively, a slight lesion in the foramen of Monro, which could cause mechanical obstruction, was noted on three-dimensional reconstruction heavily T2-weighted imaging (Fig. 1D).

Findings of the magnetic resonance imaging.
(A) Enlargement of the left lateral ventricle and periventricular hyperintensity on T2-weighted imaging. (B) No obvious tumors, cysts, and leptomeningeal enhancement on gadolinium-enhanced T1-weighted imaging. (C) No apparent membranous structures in the foramen of Monro on heavily T2-weighted imaging. (D) Membranous lesion on the coronal view of heavily T2-weighted imaging (red arrows).
A burr hole was created 1 cm anterior from the coronal suture and 4 cm lateral from the midline. Subsequently, a flexible neuroendoscope was introduced into the anterior horn of the left lateral ventricle. An obstruction with a yellowish-white membranous structure was found at the foramen of Monro (Fig. 2A), and it was excised and collected for histopathological analysis (Fig. 2B). Considering insufficient cerebrospinal fluid passage through the foramen of Monro, septostomy was performed with dilation of the balloon, followed by EVD tube replacement (Fig. 2C). Histopathological findings of the biopsy indicated noncaseating epithelioid cell granuloma with multinucleated giant cells and lymphocytic infiltration (Fig. 3); therefore, a diagnosis of neurosarcoidosis was confirmed.

Intraoperative findings of the foramen of Monro.
(A) Membranous tissue stuck in the foramen of Monro (white arrows). (B) Biopsy of the lesion using endoscopy. (C) Fenestration of the septum pellucidum, followed by balloon dilation.

Pathological findings of the membranous lesions of the foramen of Monro. White circles reveal noncaseating epithelioid cell granuloma and lymphocytic infiltration with hematoxylin and eosin staining. White arrows show multinucleated giant cells.
Neurological symptoms including hemiparesis immediately improved after the surgical intervention, and the manual muscle test result returned to normal on postoperative day 5. Furthermore, imaging studies revealed no complications or aggravation of the hydrocephalus; thus, the EVD tube was removed on the aforementioned day. Further investigation showed 18F-fluorodeoxyglucose positron emission tomography accumulation in hilar and mesenteric lymph nodes. Methylprednisolone sodium succinate 1,000 mg/day for 3 days was administered, followed by prednisone 40 mg/day for 1 month. Serial MRI showed progressive improvement of the hydrocephalus (Fig. 4). Higher brain function responded well to the treatments (Table 1). The prednisone dosage was gradually tapered considering the clinical status improvement. Finally, the patient was discharged with a prescription of prednisone 30 mg/day and went home with no neurological symptom.
An imaging study 2 months later revealed improvement in hydrocephalus.
Test results for higher brain function
| Postoperatively (weeks) | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|
| WAIS-IV, Wechsler Adult Intelligence Scale-IV; IQ, Intelligence Quotient; TMT, Trail Making Test; MMSE, Mini Mental State Examination. | |||||
| WAIS-IV | |||||
| General IQ | 72 | 95 | |||
| Verbal comprehension | 94 | 100 | |||
| Perceptual reasoning | 62 | 84 | |||
| Working memory | 82 | 100 | |||
| Proceeding speed | 75 | 108 | |||
| TMT (second) | |||||
| A | 50 | 33 | |||
| B | 115 | 72 | |||
| MMSE | 28 | 30 | |||
The prevalence of sarcoidosis is 10-20 per 100,000 population, with neurosarcoidosis being particularly rare (5%-7%).2-4) Epidemiological studies on neurosarcoidosis are nearly nonexistent due to the rarity of this condition.
Sarcoidosis affecting the central nervous system can lead to meningeal lesions (meningitis, hypertrophic pachymeningitis), granulomatous lesions in brain parenchyma or spinal cord, hydrocephalus, vascular lesions (vasculitis, periventricular white matter lesions, and venous sinus thrombosis), and encephalopathy. The diagnosis is based on clinical symptoms, cerebrospinal fluid analysis, and imaging studies, with a definitive diagnosis requiring biopsy of the affected area. Cerebrospinal fluid analysis may reveal lymphocytosis as well as elevated protein and elevated ACE and sIL-2R levels, but these findings are nonspecific.4) Imaging studies are also nonspecific; however, the affected areas exhibit low-to-faint high signal intensity on T1-weighted images and localized-to-diffuse high signal areas on T2-weighted images, with a strong gadolinium enhancement effect. At present, there are no standard therapy options or major clinical trials on the treatment modality for this condition. Steroids are used as the primary treatment, with 71% of patients reported to have yielded favorable results with steroid monotherapy.2)
The etiology of hydrocephalus is categorized into two types: communicating and noncommunicating. The former arises from impaired cerebrospinal fluid absorption due to chronic meningitis,5) whereas the latter is believed to occur due to granulomatous compression of the aqueduct of Sylvius or the fourth ventricle.6) Improvement in consciousness disturbance with endoscopic third ventriculostomy and steroid administration due to noncommunicating hydrocephalus has been reported.7)
In the present case, it was presumed that the granulomas obstructed the foramen of Monro, isolating one lateral ventricle. Perforation of the transparent septum relieved the isolation, resolving the hydrocephalus.
This case exhibited two notable features: the development of hemiplegia due to noncommunicating hydrocephalus affecting only one lateral ventricle and the ability to perform both hydrocephalus resolution and histopathological diagnosis through perforation of the transparent septum neuroendoscopically. Further details on these two aspects are described below.
First, neurosarcoidosis can lead to unilateral hydrocephalus, resulting in hemiparesis. Nervous system involvement is observed in 5%-7% of patients with sarcoidosis,2-4) encompassing cranial and peripheral nerve lesions such as facial nerve palsy, optic neuritis, aseptic meningitis, hypothalamic and pituitary dysfunction, hearing abnormalities, seizures, cognitive dysfunction, small fiber neuropathy, and polyneuropathy.2,3,8,9) Hydrocephalus, a rare condition, is present in 9% of patients with neurosarcoidosis and carries a poor prognosis.10) The diagnosis of hydrocephalus caused by neurosarcoidosis is challenging due to limited sensitivity and specificity in clinical presentations and ancillary investigations. Typically, clinical symptoms manifest as headache, vertigo, gait abnormalities, decreased visual acuity, and altered mental status.2,8) Unilateral hydrocephalus is caused by mechanical obstruction of the foramen of Monro. There are reports on unilateral hydrocephalus, which are commonly caused by neoplasms or infectious conditions, such as gliomas, choroid plexus papillomas, craniopharyngiomas, tuberculomas, neurocysticercosis, brain abscesses, or meningitis.11,12) Notably, there are no reported cases of unilateral hydrocephalus caused by neurosarcoidosis. In the present case, right hemiparesis immediately improved postoperatively before starting the immunosuppressive therapy for neurosarcoidosis. Thus, the neurological symptoms should be caused by progressive unilateral hydrocephalus. While functional imaging studies, such as diffusion tensor imaging, were not conducted in the present case due to urgency, temporary dysfunction may result from motor fiber compression.13)
Second, endoscopic surgery plays a pivotal role in the diagnosis and treatment of this condition. Over the past decades, endoscopic surgery for hydrocephalus associated with neurosarcoidosis has been reported.14-17) Simple cerebrospinal fluid shunt procedures provide only partial solutions for noncommunicating hydrocephalus. The endoscopic approach, which involves the removal of obstructive structures, septostomy, and third or fourth ventriculostomy with shunt procedures, has been proven to be more effective.16,17) In terms of surgical invasiveness, this procedure requires only a small burr hole in the skull, comparable in size to those required for EVD or ventriculoperitoneal shunt. Moreover, a study by Reddy et al. in 201118) reported the etiology of noncommunicating hydrocephalus in 468 patients with adult-onset disease, revealing tumors and cysts as the most common causes (45%), followed by postcraniotomy (16%) and post-trauma (15%). Most patients with neurosarcoidosis also exhibit systemic sarcoidosis. In acute clinical scenarios such as the present case, there may be insufficient time for extensive investigations, and it can be challenging to clearly distinguish obstructive lesions from normal structures, such as the choroid plexus. When the etiology of acute hydrocephalus remains unclear, endoscopic surgery provides a suitable option for immediate treatment and biopsy, enabling tailored medical interventions postoperatively. If the clinical symptoms rapidly progress, obstructive hydrocephalus should be considered irrespective of the findings on imaging studies and endoscopic intervention should be selected rather than ventricular drainage. Preoperative MRI cerebrospinal fluid flowmetry might have facilitated the prediction of obstructive mechanisms.
In the present case, the hydrocephalus resulted from membranous tissue obstruction attributed to neurosarcoidosis; however, all patients presenting with aqueductal stenotic lesions or unidentified etiologies are potential candidates for this procedure. Various reports have emphasized the application of endoscopy for the diagnosis and treatment of obstructive hydrocephalus.19)
Interestingly, neurosarcoidosis can present with hemiparesis caused by unilateral hydrocephalus as the primary symptom. In the present case, endoscopic surgery yielded favorable results. The endoscopic procedure is presumed to serve as a suitable option for the diagnosis of noncommunicating hydrocephalus, while also providing a minimally invasive and effective treatment.
Consent from the participant was obtained.
None