2024 Volume 11 Pages 377-382
2024 Volume 11 Pages 377-382
Although rare, penetrating cervical vascular injury poses significant challenges with a poor patient prognosis, often attributed to severe hemorrhage and accompanying injuries. We encountered a case of hemorrhagic shock resulting from a penetrating injury to the common carotid artery (CCA), which was successfully managed using a combination of endovascular therapy and direct surgical intervention.
A 23-year-old man presented with a self-inflicted stab wound on the left side of his neck from a kitchen knife. This injury resulted in hemorrhagic shock and coma. Initial management included fluid resuscitation and transfusion, with continuous manual compression to control profuse bleeding. Contrast-enhanced neck and brain computed tomography (CT) showed a left CCA injury that was challenging to directly address due to its low anatomical location and continuous bleeding. Neurosurgeons initiated endovascular treatment by placing a guiding balloon catheter proximal to the left CCA for occlusion. Despite this, pulsatile bleeding persisted, prompting the distal placement of a balloon catheter to achieve better bleeding control. Cardiovascular surgeons then performed direct surgery, clearly identifying damage to the anterior and posterior walls of the CCA. The repair involved the use of a self-made cylindrical bovine pericardial patch, which resulted in successful revascularization.
Following surgery, the patient regained independent mobility and was discharged. This case emphasizes the importance of a prompt and reliable approach involving endovascular intervention for initial bleeding control followed by precise repair through direct surgery, especially in challenging bleeding scenarios.
Penetrating neck trauma is a rare occurrence, with a frequency of 1.3 cases per 100,000 individuals.1) Globally, the primary causes of these injuries are stab wounds from assailants, gunshot wounds, and traffic accidents.2) Vascular injuries are the leading cause of mortality, followed by airway obstruction, cerebral infarction, and sepsis.2)
Historically, acute cervical vascular injuries have had a high mortality rate of 66%.3) Even with surgical intervention, mortality rates are approximately 20%,3,4) although recent reports from specialized centers suggest an improvement to approximately 15%.5) The risk of stroke following trauma remains high despite the advancements, affecting approximately 20% of the cases.5)
Emergency surgical intervention is crucial in cases with significant neck vessel injuries, given the vulnerability of the circulatory system.2) However, due to the rarity of acute neck trauma and the intricate anatomy of the neck, a consensus on the optimal surgical approaches remains elusive.
In the present case, we treated a patient with hemorrhagic shock due to a penetrating injury to the common carotid artery (CCA). Our approach involved endovascular balloon occlusion to halt bleeding proximally and distally from the injury site, followed by direct CCA repair. The outcome of this intervention was favorable, emphasizing the efficacy of this hybrid approach.
A 23-year-old man with a history of depression and adjustment disorder attempted suicide at home while intoxicated and inflicted a wound on the left side of his neck with a kitchen knife. Upon hearing him fall, his family intervened, removing the knife and promptly calling for emergency medical assistance. Emergency responders arrived 16 min later, finding the patient lying on the floor in a pool of blood. His neck was compressed with a towel to control the bleeding. He reached the hospital 42 min post-injury and presented with gasping, a systolic blood pressure of approximately 60 mmHg, and coma with a Glasgow Coma Scale score of E1V1M1. Examination showed a 3-cm penetrating wound near the cricoid cartilage of the left neck, with no active bleeding at the time.
Immediate interventions were intubation, fluid resuscitation, and rapid transfusion. As his blood pressure improved, arterial blood gushed from the wound (Fig. 1-A), prompting a contrast-enhanced computed tomography (CT) scan while maintaining manual compression. The scan showed a leakage point of contrast medium approximately 8 cm toward the head from the origin of the left CCA, at the level of the inferior part of the thyroid gland or the seventh cervical vertebra, with prominent tracheal deviation due to a hematoma and pneumomediastinum (Fig. 1-B, C). The imaging also showed collateral circulation via the anterior and bilateral posterior communicating arteries, except in the territory on the left side of the superior trunk of the middle cerebral artery (MCA) (Fig. 1-D), with an embolic source from the suspected neck vessel injury (Fig. 1-E). The evaluation of brain ischemia tolerance could not be conducted since the patient was in severe shock. The patient's hemoglobin levels remained stable (14.2 g/dL), and abnormal coagulation (activated partial thromboplastin time [APTT], 46.9 s; prothrombin time-international normalized ratio [PT-INR], 1.30; D-dimer, 1.1 μg/mL) and severe acidosis (pH, 6.87; anion gap, 34.6) were noted.

(A) Preoperative photograph of the patient with severe bleeding from the left cervical wound. (B) Frontal view of the neck on contrast-enhanced computed tomography (CT). The arrow indicates the injured left common carotid artery (CCA). The trachea (intubation tube shown in light blue) and thyroid gland (shown in green) are significantly displaced to the right due to the hematoma. (C) Lateral view. The injured left CCA (arrow) is located 8 cm distal to the aortic arch and 6.5 cm proximal to the cervical carotid bifurcation, near the lower thyroid and close to the mediastinum. (D) Axial view of contrast-enhanced CT at the level of the CCA injury. The common carotid artery is injured (arrowhead). (E) Axial view of the intracranial contrast-enhanced CT. No vessels visible in the region of the superior trunk of the left middle cerebral artery.
In the present case, both neurosurgeons and cardiovascular surgeons considered direct surgical repair risky due to profuse bleeding, as the CCA injury was too low to be identified in the surgical field. Thus, an intra-arterial shunt was not used. A thoracotomy was also possible. Consequently, the neurosurgeons planned to promptly initiate endovascular treatment to control bleeding, followed by direct repair of the injured CCA by cardiovascular surgeons in a hybrid operating room.
Endovascular therapy was administered through the right femoral artery. A balloon-guided catheter (Flowgate2 8F; Stryker, Tokyo, Japan) was inserted and proximal blood flow in the left CCA was managed. Common carotid angiography showed leakage of contrast medium from the injured CCA with no observable progressive blood flow beyond the injury point (Fig. 2-A). However, persistent gushing bleeding due to retrograde blood supply was observed. We could successfully navigate past the lesion using a micro guidewire (CHIKAI 0.014 in.; ASAHI, Aichi, Japan) whose tip was bent into a small J-shape, allowing it to traverse the injured segment smoothly and without snagging the damaged vessel wall. The endovascular surgeon carefully monitored for any unusual resistance felt through the micro guidewire and closely observed the imaging to ensure that there was no deviation from the intended path while passing through the injury site. A distal balloon occlusion with a balloon catheter (Sterling 4.5 mm/30 mm; Boston Scientific Japan, Tokyo, Japan) was deployed, which effectively controlled the bleeding (Fig. 2-B). Bleeding control was achieved 37 min after entering the hybrid operating room.
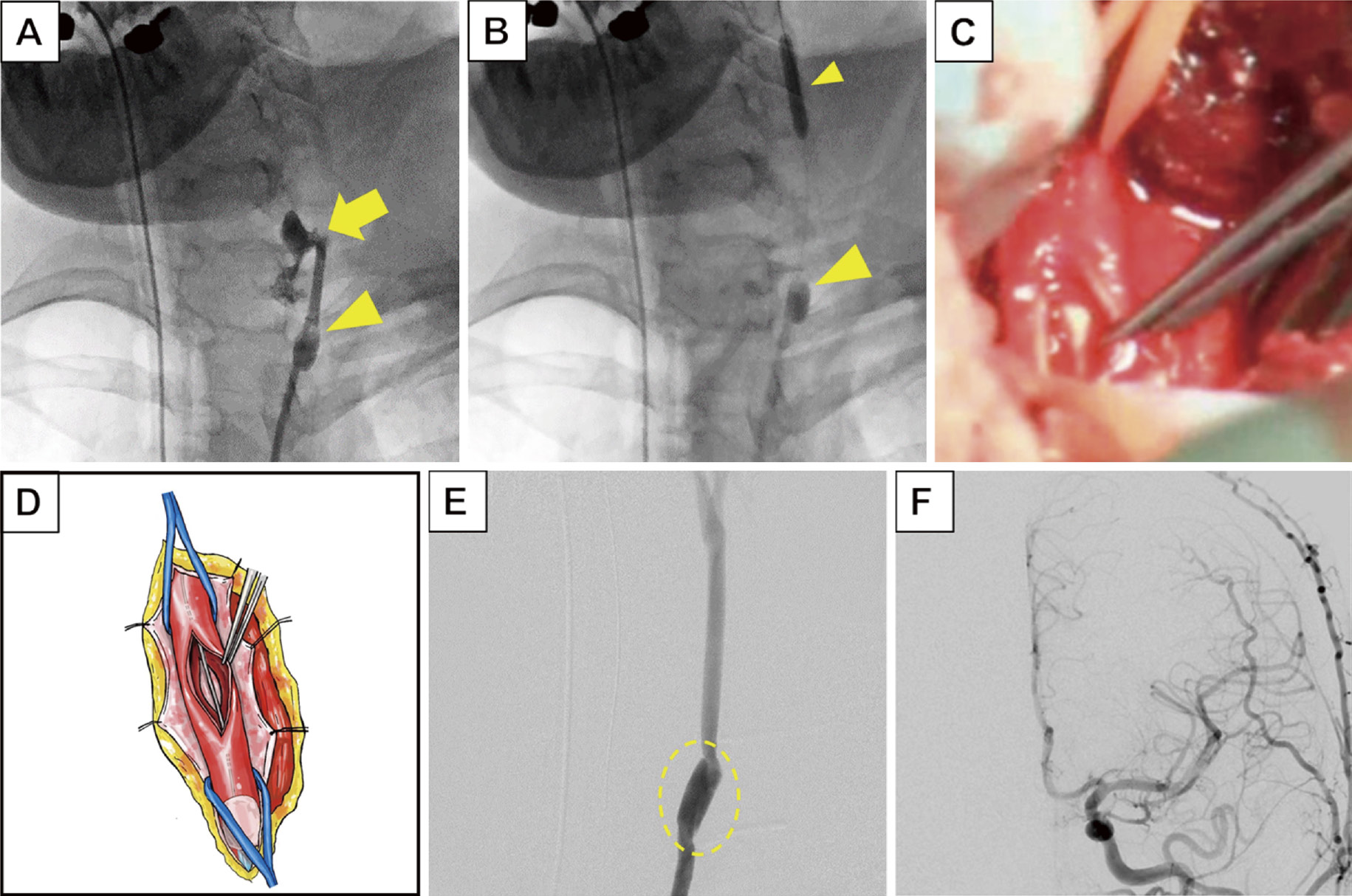
(A) Frontal view of the left common carotid angiography, with blood flow controlled using a balloon-guided catheter (large arrowhead). Contrast medium leakage from the injured common carotid artery (CCA) is indicated (arrow). (B) Balloon occlusion of the proximal (large arrowhead) and distal (small arrowhead) sites of the injured left CCA. (C) Intraoperative view of the penetrated left CCA. (D) Schematic representation of the CCA within the operative field, illustrating the anterior and posterior wall injury and the presence of a balloon catheter. (E) A bovine pericardial patch crafted into a conduit used as an interposition graft for the injured CCA (dotted box) and restoration of antegrade blood flow. (F) Postoperative left CCA, showing no apparent new intracranial vascular occlusion compared with his preoperative computed tomography scan.
The cardiovascular surgeons then performed direct surgery. An incision was made along the sternocleidomastoid muscle, and a perforating injury of approximately 15 mm was found through the anterior and posterior walls of the CCA (Fig. 2-C, D). After deflating and removing the distal balloon catheter, the distal portion of the CCA was occluded with a vascular clamp. Due to the difficulty of exposing the proximal portion of the CCA, proximal balloon occlusion was maintained throughout the procedure. Repair with simple closure could lead to CCA stenosis, or using an artificial vessel posed a risk of infection. Therefore, a bovine pericardial patch (Edwards bovine pericardial patch model 4700; Edwards Lifesciences Irvine, California, USA) was shaped into a conduit with 5-0 Pronova suture (Ethicon, Inc., Somerville, New Jersey, USA), matching the CCA diameter (6 mm) to be used as an interposition graft for the injured CCA. Moreover, 2500 units of heparin were administered to prevent embolic complications during the procedure. We then performed an end-to-end anastomosis at both ends of the graft using 6-0 Pronova sutures. Before completing the proximal anastomosis, the clamp blocking blood flow on the distal side was removed, allowing debris to be flushed out with retrograde blood flow. Final suturing of the proximal side was then completed. After confirming that the color and pulsation were satisfactory, the proximal balloon was slowly deflated, and successful recanalization of CCA was verified (Fig. 2-E). The left CCA was occluded for 2 h and 19 min, with progressive circulation resuming approximately 5 h and 30 min after injury. Left common carotid angiography showed occlusion of the left superior trunk of the MCA, for which no intervention was performed due to matching preoperative CT findings (Fig. 2-F). No damage to the esophagus or airway was noted in the field of view. The vagus nerve was identified near the carotid sheath, and it was located away from the injury site. The total blood loss was estimated at approximately 2600 mL, with an intraoperative blood loss of 600 mL. The patient was intubated and transferred to the intensive care unit (ICU) under sedation.
A CT scan conducted the day after surgery showed cerebral infarction only in the territory of the left MCA superior trunk. On the second postoperative day, treatment with aspirin (100 mg) and heparin (10,000 units/day) was initiated. Heparin was continued for 7 days, whereas aspirin was continued for 3 months in consideration for the short length of the replacement. Extubation was performed on the 6th postoperative day. The patient then regained independent mobility and was transferred to a rehabilitation hospital on the 18th postoperative day with mild paralysis and aphasia. At this time, the patient's GCS was E4V5M6, and Glasgow Outcome Scale was 3. After being discharged from the rehabilitation facility, the patient visited the outpatient clinic independently.
In the present case, the patient arrived comatose and in a hemodynamically unstable state, posing a high risk of mortality.3-5) In addition, initial contrast-enhanced CT scans indicated an embolism of the left MCA, probably resulting from a thrombus formed at the wound site. Rapid bleeding control from the penetrating neck injury was imperative to save the patient's life. Given the high mortality rate associated with ligation,4) the fact that only an hour had passed since the injury, and the absence of early ischemic signs on the CT, revascularization surgery was considered, although the patient's ischemic tolerance remained uncertain.6) However, the location of the injury and persistent severe bleeding led to an unclear surgical field, posing challenges. Consequently, endovascular treatment was performed to manage the bleeding. Using a balloon occlusion solely proximal to the injured CCA was insufficient to achieve hemostasis. Incorporating a distal occlusion proved effective in providing adequate bleeding control and facilitating maneuverability within a complex surgical field with thoracic restrictions.
The neck has a complex anatomy with vital structures such as the airway, esophagus, nerves, and major blood vessels, leading to diverse complications depending on the site of injury. Traditionally, surgical management has been categorized into three zones based on the wound height. However, because the skin puncture site may not always align with the deeper injury point,7) a recent approach advocates tailoring surgical strategies to the specific injury site guided by evaluation with multidetector computed tomography-angiography (MDCT-A) scans.8,9) Severe cases of acute CCA injury typically require vascular repair during direct surgery.5) However, lesions near the subcricoid cartilage pose the highest mortality risk due to the constraints imposed by the bony thorax and clavicle, which hinder surgical field visibility.10,11) In the present case, direct surgery without adequate bleeding control posed a substantial risk of damaging vital structures. Hence, we prioritized bleeding control through endovascular treatments performed by neurosurgeons. The duration from the initiation of endovascular treatment to balloon occlusion of the proximal parent vessel was 20 min, during which time direct compression and transfusion effectively maintained the circulatory dynamics.
Achieving hemostasis in carotid artery injury often requires not only controlling the proximal blood flow but also addressing the retrograde distal blood flow. Although reports have highlighted the effectiveness of proximal balloon tamponade in controlling bleeding,12,13) exploration of combined proximal and distal balloon tamponade techniques for CCA injuries has been limited, including those from trauma and tumor-related diseases, such as carotid blowout syndrome. In zone 3 CCA injuries, techniques involving distal balloon catheter insertion through a small incision in the internal carotid artery have been used to manage bleeding when retrograde blood flow poses a challenge.14) In the present case, both proximal and distal balloon tamponade were achieved, highlighting the enhanced efficacy of endovascular hemostasis before vessel repair.
Direct surgery is useful not only for detecting vascular damage but also for identifying other types of injuries. The detection of pharyngoesophageal injuries through MDCT-A is not always guaranteed, with reported mortality rates of 20% for pharyngotracheal trauma15) and 22% for pharyngoesophageal injuries.16) Therefore, direct surgical observation is highly beneficial to identify complications and enable immediate intervention.
In recent years, endovascular treatment has been favored over direct surgery.17-19) Du Toit et al. reported a mortality rate and stroke incidence of 5%, indicating a favorable prognosis compared with that with direct surgery.17) Endovascular treatments, such as coil embolization and various types of stenting,18) are increasingly used, particularly in cases of pseudoaneurysms or arteriovenous fistulas. However, inadequate hemostasis after endovascular treatment may necessitate direct surgery, as observed in some cases of hemorrhagic shock.19-21) In this situation, catastrophic bleeding from the wound makes it impractical to use covered stenting due to the uncertainty regarding complete hemostasis and the unavailability of stenting devices within the limited timeframe of an emergency setting.
Stenting requires the administration of antiplatelet agents to prevent in-stent occlusion, with guidelines recommending dual antiplatelet therapy for at least 3 months, followed by lifelong monotherapy.22-24) In contrast, in the present case, a bovine pericardial patch was cylindrically shaped to replace the injured CCA, with heparin administered for 1 week and aspirin administered for 3 months. Despite the absence of established guidelines regarding the administration of antithrombotic in such cases, our decision was based on the cardiovascular surgeon's standard practice at our institution. Direct surgical reconstruction may be beneficial in cases in which medication compliance is a concern.
This case emphasizes the fortunate convergence of several critical factors, such as the availability of a hybrid operating room, the prompt involvement of cardiovascular surgeons, and favorable patient-related conditions, all of which played a crucial role in achieving a successful outcome.
We effectively treated a patient with hemorrhagic shock and penetrating CCA injury by combining endovascular balloon occlusion at both the proximal and distal injury sites with direct surgical repair. The endovascular technique swiftly and precisely controlled bleeding, whereas the direct approach allowed us to address accompanying trauma during vascular repair. This treatment strategy can minimize surgical complications. Further studies are needed to confirm the effectiveness of this hybrid approach in additional cases and broader clinical applications.
APTT, activated partial thromboplastin time
CCA, common carotid artery
CT, computed tomography
ICU, intensive care unit
MCA, middle cerebral artery
MDCT-A, multidetector computed tomography-angiography
PT-INR, prothrombin time-international normalized ratio
Informed consent for the publication of this case report and accompanying images was obtained from the patient.
The authors declare no conflicts of interest.