2025 年 12 巻 p. 59-64
2025 年 12 巻 p. 59-64
The conventional transcranial approach for treating lower basilar artery aneurysms is challenging because the deep and narrow surgical field limits surgical maneuvering for clipping. We report a case of a 77-year-old female who presented with right hemiparesis caused by a partially thrombosed giant aneurysm in her lower basilar artery. We performed neck clipping and thrombus debulking using a combined transcranial and endonasal approach. This approach enabled us to secure the parent artery from the endonasal side, which is difficult to achieve with the transcranial approach alone. It also allowed for early thrombus removal, thereby widening the surgical field on the transcranial side. Additionally it compensated for the transcranial blind spot by observing the clip tip from the endonasal side. After surgery, the patient required 3 months of rehabilitation for residual right hemiparesis before being discharged. Follow-up imaging revealed a reduction in the size of the partially thrombosed aneurysm. To our knowledge, this is the first report of a combined transcranial and endonasal approach for the treatment of a basilar artery aneurysm. For lower basilar artery aneurysms, this combined approach may offer advantages in achieving safe parent artery control, thrombus debulking, and neck clipping.
The conventional transcranial approach for lower basilar artery (BA) aneurysms is challenging because the deep, narrow surgical field limits maneuverability during clipping and parent artery control.1,2) The transcondylar or transpetrosal approach is commonly used for lower BA aneurysms, but requires advanced skull base skills due to the limited visual field and working space, complex vascular anatomy, and proximity to cranial nerves and brainstem structures.3,4) In partially thrombosed lower BA aneurysms, the mass effect of the aneurysm significantly narrows the surgical field, complicating parent artery control. Endovascular treatment for partially thrombosed aneurysms has been reported, but the recurrence rate and residual mass effect must be considered.5,6) In our previous report, Sato et al.7) presented a combined transcranial and endonasal approach for internal carotid artery (ICA) aneurysms clipping, which facilitated easier parent artery control and maximized the use of the limited surgical field. However, no reports have described this combined approach for posterior circulation aneurysms. Here, we describe the application of this combined approach for treating a partially thrombosed giant aneurysm of the lower BA.
A 77-year-old female with hypertension was admitted to our hospital with worsening right hemiparesis that had persisted for several months. Magnetic resonance imaging revealed a heterogeneous lesion with a maximum diameter of 25 mm in the left pons, associated with mass effect and perilesional edema (Fig. 1A). Cerebral angiography and computed tomography angiography identified a partially thrombosed aneurysm at the BA-left anterior inferior cerebellar artery (AICA) bifurcation, with the left posterior inferior cerebellar artery (PICA) sharing a common trunk with the left AICA (Fig. 1B and C). The aim of the treatment was to prevent rupture of the aneurysm and reduce the mass effect. Achieving parent artery control using the conventional transcranial approach was difficult because of the limited surgical field. Consequently, neck clipping and thrombus debulking were performed using a combined transcranial and endonasal approach. The effectiveness of this combined approach has been reported in the removal of brain tumors,8) and we have already used this approach for ICA aneurysms clipping.7) Therefore, approval from the Institutional Review Board of Sapporo Medical University was not required.

Preoperative imaging. (A) T2-weighted image showing a heterogeneous lesion with a maximum diameter of 25 mm in the left pons with associated mass effect and perilesional edema. (B) Cerebral angiography showing an aneurysm at the BA—left AICA bifurcation, and the left posterior inferior cerebellar artery which share a common trunk with the left AICA. (C) 3-dimensional computed tomography angiography demonstrating the partially thrombosed giant aneurysm of the lower BA.
AICA: anterior inferior cerebellar artery; BA: basilar artery
The patient was first placed in the supine position, and an endoscope was inserted into the right nostril. A nasoseptal mucoperiosteal flap on the vascular pedicle was harvested for subsequent reconstruction of the skull base defect. Anterior sphenoidectomy and clivectomy were performed, allowing visualization of the BA union and proximal AICA. The patient was then repositioned laterally, and a left lateral suboccipital craniotomy was performed (Fig. 2A and B). The left occipital artery (OA) was anastomosed to the hemispheric branch of the left PICA, which shared a common trunk with the AICA, to prepare for temporary proximal artery occlusion during thrombus debulking. A temporary clip (Sugita No. 15; Mizuho, Aichi, Japan) was applied to the AICA from the endonasal side (Fig. 2D), and the thrombus was debulked through the peritrigeminal zone of the pons from the transcranial side, thereby widening the surgical field. Subsequently, using an endonasal endoscope for visualization, a permanent standard straight clip (Sugita No.15; Mizuho) was applied to the neck of the aneurysm (Fig. 2C-F). However, the AICA was injured during the application of the permanent clip; therefore, the proximal AICA was clipped together with the aneurysm neck using a permanent straight mini-clip (Sugita No.100; Mizuho) (Fig. 2E and F). The patency of the OA-PICA bypass was favorable, and the blood flow through the AICA-PICA common trunk was confirmed using Doppler ultrasonography and indocyanine green videoangiography. Based on these findings, we considered that blood flow to the AICA and PICA territories could be maintained via the OA-PICA bypass, even if the proximal AICA was occluded (Fig. 3A and B). After the wound was closed, the patient was repositioned in the supine position, and the defect in the skull base was reconstructed using a multilayer technique from the endonasal side. A fascia lata graft was placed as an intradural inlay graft followed by an extradural onlay collagen matrix graft (DuraGen; Integra LifeSciences, Princeton, NJ, USA). After a fat and fascial graft was used to obliterate the dead space, a nasoseptal mucoperiosteal flap was placed over the grafts. Fibrin glue was applied to each layer. A 12-French balloon catheter was inserted transnasally to provide support to the grafts to prevent graft migration, and a lumbar cerebrospinal fluid (CSF) drainage was used for several days. The operative video is provided in the Supplementary Material.

Intraoperative imaging. (A), (B) The patient was placed in the right lateral position, and the combined approach was performed by 2 independent neurosurgeons. (C) Intraoperative photograph of the transcranial side. The permanent standard clip was applied to the aneurysm neck. (D) Intraoperative photograph of the endonasal endoscopic view. The temporary clip was applied to the left AICA from the endonasal side, and the tip of the permanent clip can be seen. (E) Schematic drawings of the transcranial approach. The permanent standard clip was applied to the aneurysm neck, and the permanent mini clip was used to occlude the injured proximal AICA (illustrated within the square). (F) Schematic drawings of the endonasal endoscopic side, visualizing the tips of the transcranial clips.
AICA: anterior inferior cerebellar artery; AN: aneurysm; BA: basilar artery; CN: cranial nerve; OA: occipital artery; PICA: posterior inferior cerebellar artery
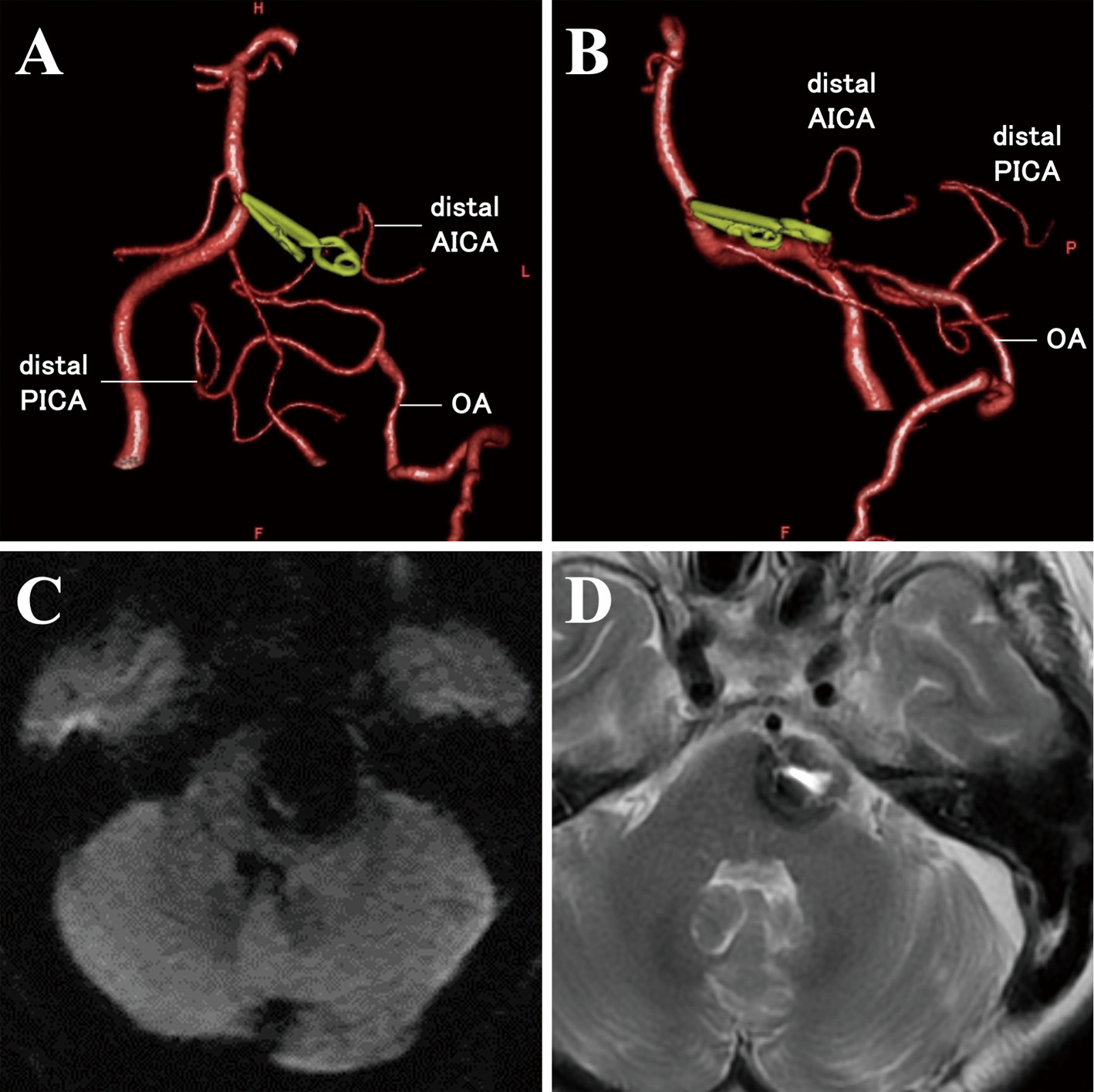
Postoperative imaging. (A) Frontal and (B) lateral view of 3-dimensional computed tomography angiography demonstrating the maintained blood flow to the distal AICA and the disappearance of the blood flow to the aneurysm. (C) Diffuse weighted image at the day next of operation showing no ischemic lesions. (D) T2-weighted image taken 12 months post-surgery, showing the shrunken thrombosed aneurysm and the disappearance of the pontine edema.
After surgery, no new neurologic deficits or ischemic lesions appeared (Fig. 3C), but the patient required 3 months of rehabilitation for residual right hemiparesis before being discharged. Magnetic resonance imaging at 12 months post-surgery showed that the partially thrombosed aneurysm was shrinking and the pontine edema had disappeared (Fig. 3D).
We identified 2 important clinical issues: the merits of this approach and surgical risk control. For a partially thrombosed lower BA aneurysm, the combined transcranial and endonasal approach allows for easier parent artery control and a favorable clip position.
A combined transcranial and endonasal approach can compensate for the shortcomings of the individual approaches. Although several useful transcranial approaches exist, they are particularly challenging for lower BA aneurysms.1,2,4) In cases of partially thrombosed giant lower BA aneurysms, transcondylar approaches are typically effective in establishing a surgical field; however, in this case, the distal BA remained obscured by the aneurysmal dome.9,10) Applying direct pressure to the aneurysmal dome to widen the surgical field carries the risks of rupture, thrombus migration, or brainstem compression. Conversely, while the subtemporal or transpetrosal approach provides easier access to the distal BA, it presents challenges in securing the proximal BA. Some studies have combined these skull base approaches to facilitate control of the parent artery.11) However, naturally, such combinations increase operative time, invasiveness, and require advanced skull base skills. In addition, within the limited transcranial surgical field, it is difficult to visualize the aneurysm neck, parent artery, perforating arteries, cranial nerves, or clip tips, which can lead to severe complications due to unfavorable surgical procedures.12) In contrast, the endonasal approach can directly access the lower BA through the clivus without confronting critical structures, facilitating parent artery control.13,14) However, depending on the position of the aneurysm, the endonasal approach may not be suitable for neck clipping or thrombus debulking. Therefore, we considered a combined transcranial and endonasal approach for treating the partially thrombosed giant aneurysm of the lower BA. This combined approach allowed for easier parent artery control from the endonasal side and enabled favorable clip positioning by visualizing the aneurysm from different angles. Additionally, this approach compensates for the limitations of each individual method, thereby reducing the need for advanced skull base expertise.
To the best of our knowledge, this is the first report of a combined transcranial and endonasal approach for treating a BA aneurysm. Although this combined approach has been used for skull base tumors,8,15) there are a few reports on its application to intracranial aneurysms. A literature review in PubMed revealed only 5 cases that were treated with this approach-4 cases of ICA aneurysms and 1 case of a vertebrobasilar artery aneurysm (Table 1).7,16) Transcranial and endonasal approaches were performed in all cases: simultaneously in 4 cases of ICA aneurysms and separately in 1 case of a vertebrobasilar artery aneurysm. In the cases reported by Sato et al.,7) the endonasal approach was used for parent artery control at the same time as the transcranial approach, as in our case, and no patients experienced perioperative complications. In contrast, in the case reported by Plitt et al.,16) the endonasal approach was used for thrombus debulking after parent artery occlusion using transcranial and endovascular techniques. This review suggested that simultaneous transcranial and endonasal approaches may be less invasive and time-saving, allowing for rupture prevention, mass reduction, and parent artery control in a single surgical stage. Particularly in vertebrobasilar artery aneurysms, as previously noted, this approach compensated for the blind spot by enabling visualization of the tip of the transcranial clip from the endonasal side.
Summary of intracranial aneurysms treated with transcranial and endonasal approaches
| Author (year) | Age/ Sex | Location | Size (mm) | Thrombosed | Operation | Timing | |
|---|---|---|---|---|---|---|---|
| Transcranial | Endonasal | ||||||
| BA: basilar artery; F: female; ICA: internal carotid artery; M: male; PAO: parent artery occlusion; VB: vertebrobasilar | |||||||
| Sato et al. 7) (2023) | 70/F | ICA | 8.0 | No | Neck clipping | Proximal artery securing | Simultaneously |
| 23/F | ICA | 4.0 | No | Neck clipping | Temporary proximal clipping | Simultaneously | |
| 75/M | ICA | 7.5 | No | Neck clipping | Temporary proximal clipping | Simultaneously | |
| 76/M | ICA | 8.0 | No | Neck clipping | Temporary proximal clipping | Simultaneously | |
| 45/F | ICA | 4.0 | No | Distal ligation | Proximal ligation | Simultaneously | |
| Plitt et al. 16) (2019) | 44/F | VB junction | 45 | Yes | Distal ligation (with endovascular PAO) | Thrombus debulking | Separately |
| Our case | 77/F | BA | 25 | Yes | Bypass, thrombus debulking, and neck clipping | Temporary proximal clipping and observation of the transcranial blind spot | Simultaneously |
Bypass surgery for temporary proximal artery occlusion can be performed using the transcranial approach. In our case, by securing blood flow in the AICA-PICA through bypass surgery from the transcranial side, and subsequently applying a temporary clip to the proximal AICA-PICA common trunk from the endonasal side, we were able to debulk the thrombus widely from the transcranial surgical field during the subsequent procedure. In the final step, the bypass helped prevent postoperative ischemic complications, despite permanent occlusion of the proximal AICA-PICA with a clip. Although bypass surgery is not always necessary for short-term temporary occlusion of the parent artery, it plays a critical role in ensuring safety during surgery for giant aneurysms.
The endonasal approach alone for clipping vertebrobasilar artery aneurysms is feasible but has limitations. Many researchers have reported endonasal clipping,14,17) and in the cadaveric study by Montaser et al.,18) the feasibility of clip placement was shown at the vertebral artery, PICA, BA, AICA, superior cerebellar artery, P1 segment of posterior cerebral artery, and posterior communicating artery. The endonasal approach can access the vertebrobasilar arteries through the clivus but has anatomical limitations. First, the lateral limits are formed by the cavernous segment of the ICA in the upper two-thirds and the occipital condyles in the lower one-third.13) The cranial limit is normally the sella turcica but can be extended to the dorsum sellae by pituitary transposition.19) The caudal limit is defined as the superior articular facet of the first cervical vertebra.20) These anatomical limitations do not account for instrument maneuverability, and the endonasal surgical field becomes narrower depending on the location and size of the aneurysm.19) Furthermore, endonasal clips can protrude through the clivus and displace the reconstructive multilayer grafts, causing CSF leakage. Newly refined low-profile clips may help overcome this disadvantage. However, to date, clipping from the transcranial side, assisted by endonasal observation, remains the best option for treating lower BA aneurysms.
In summary, combined transcranial and endonasal approaches could be useful for treating giant aneurysms of the lower BA, because this combined approach allows for easy parent artery control.
None of the authors received any financial assistance for this research.
The patient signed informed consent regarding publishing her data and photographs.
Author Nobuhiro Mikuni is one of the Editorial Board members of the Journal. This author was not involved in the peer-review or decision-making process for this paper.
All authors have no conflict of interest.