2015 Volume 2 Issue 1 Pages 12-15
2015 Volume 2 Issue 1 Pages 12-15
A 31-year-old woman with pure red cell aplasia presented with motor aphasia and right homonymous hemianopia due to a left temporal and parietal lobe infarction. Magnetic resonance angiography revealed an occlusion of the left anterior and middle cerebral artery, with the development of moyamoya vessels. She was diagnosed with quasi-moyamoya disease and subsequently underwent direct and indirect anastomosis surgery, while continuing steroid and immunosuppressant therapy for pure red cell aplasia. The postoperative course was uneventful, and follow-up cerebral angiography 6 months after the surgery revealed the development of neovascularization through an indirect anastomosis. Neovascularization can be induced while the patient is receiving steroid and immunosuppressant therapy in quasi-moyamoya disease.
Moyamoya disease is a progressive occlusive cerebrovascular disease of the internal carotid artery and its main branches within the circle of Willis, which is accompanied by the development of a fine collateral network at the base of the cerebral hemisphere.1,2) Although it is sometimes manifested by hemorrhagic stroke in adults, moyamoya disease often causes cerebral ischemia; for some of these patients who have cerebral ischemia, surgical revascularization is beneficial. Moyamoya disease with several underlying disease, which include hematological disorders, is categorized as quasi-moyamoya disease.
We report a case of quasi-moyamoya disease associated with pure red cell aplasia, and discuss about the relation between immunosuppressant and neovascularization. This patient presented with cerebral ischemia and was treated with combined direct and indirect anastomosis surgery, and her postoperative angiography revealed good neovascularization despite continuous administration of prednisolone and cyclosporine.
A 31-year-old Japanese woman was admitted to our hospital because of motor aphasia and right homonymous hemianopia. She had a previous history of pure red cell aplasia and had been treated with prednisolone, cyclosporine, and erythrocyte transfusion for 12 years. The magnetic resonance imaging (MRI) performed at the patient’s admission confirmed an infarction in the left temporal and parietal lobe (Fig. 1a, b). Magnetic resonance angiography (MRA) revealed an occlusion of the left anterior and middle cerebral arteries, with moyamoya vessels at the base of the cerebral hemisphere. The patient’s hemoglobin concentration was 6.2 mg/dL, and her red blood cell count was 1.62 × 106/L. Anti-platelet therapy was started as per the current treatment protocol for patients with acute ischemic stroke. Digital subtraction angiography (DSA) confirmed the diagnosis of moyamoya disease (Fig. 2). 123I-IMP single-photon emission computed tomography (SPECT) revealed that the cerebral blood flow (CBF) was severely decreased particularly in the left middle and posterior cerebral artery territory (Fig. 1c).

A diffusion-weighted magnetic resonance imaging on admission (a, b) confirmed an infarction in the left temporal and parietal lobe. 123I-IMP single-photon emission computed tomography (c) revealed severely decreased cerebral blood flow in the left middle and posterior cerebral artery territory.
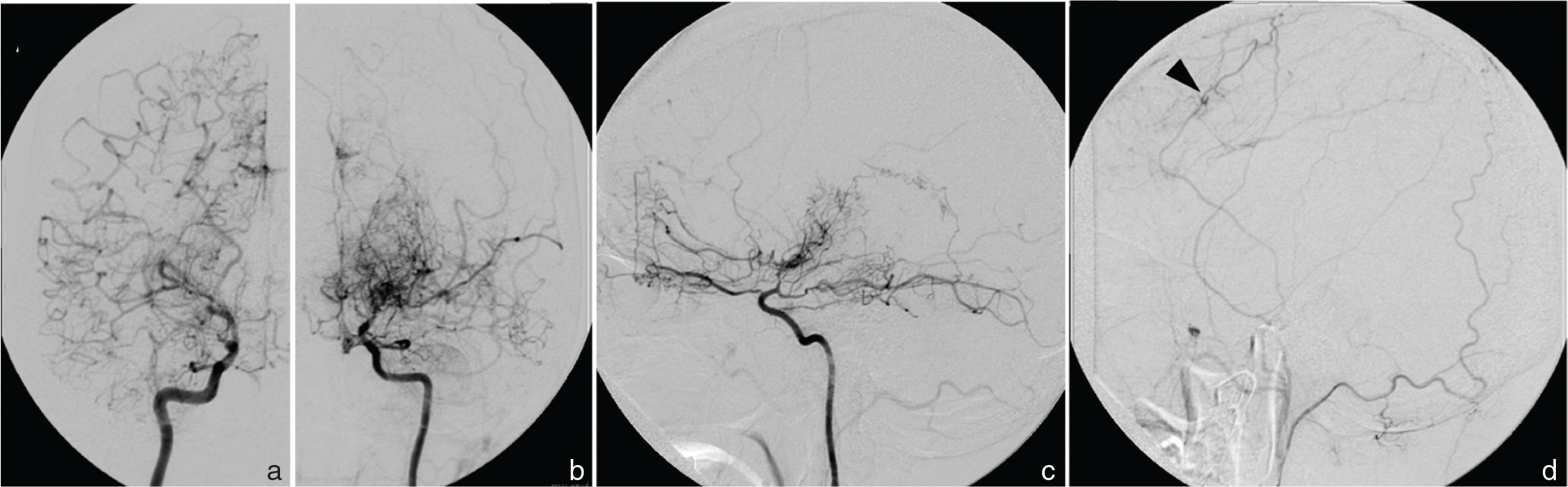
Anterior-posterior views of the left (a) and right (b) internal carotid arteriography, and the lateral view of the left internal carotid arteriography (c) show that they were occluded at the supraclinoid portion, and the anterior and middle cerebral arteries are reconstituted by collaterals from ophthalmic artery and pial collaterals along the convexity of the brain. Left external carotid arteriography (d) shows that the frontal branch of the superficial temporal artery (arrowhead) has collateral blood supply to the middle cerebral artery territory.
Thus, the infarction was determined to be a hemodynamic compromise due to moyamoya disease, and the patient underwent encephalo-duro-arterio-myo-synangiosis (EDAMS) with superficial temporal artery-middle cerebral artery (STA-MCA) and occipital artery (OA)-MCA anastomosis. The frontal branch of the STA was preserved because it has collateral blood flow to the MCA territory through the transcranial anastomosis. For good control of pure red cell aplasia, prednisolone and cyclosporine were continued as recommended by the treating hematologist. The patient, whose body weight was 56 kg, had been taking prednisolone 25 mg/day and cyclosporine 300 mg/day, and same dose of these drugs were continued since the onset of the infarction and during perioperative period. The postoperative course was uneventful, and there were no ischemic attacks after surgery. The MRA performed 2 weeks after the operation showed good patency of both anastomoses, and the patient returned to her job after rehabilitation.
A follow-up DSA was performed 6 months after surgery, which revealed that the neovascularization was well developed especially from the meningeal arteries, while the donors of the direct anastomoses (OA and the parietal branch of STA) had decreased their calibers (Fig. 3).

Left-anterior oblique view of postoperative magnetic resonance angiography (a), the left occipital arteriography (b) and the external carotid arteriography (c) taken 6 months after the operation. The neovascularization (asterisks) developed well especially from the meningeal arteries. However, the anastomosed arteries, the branch of the occipital artery (arrows), and the parietal branch of the superficial temporal artery (arrowhead), decreased in caliber and their anastomosed sites could not be detected.
Moyamoya vessel formation is associated with various diseases. These conditions are distinguished from moyamoya disease according to the statement from the research committee on moyamoya disease, and are classified as quasi-moyamoya disease.3) Hematological disorders such as sickle cell anemia, beta-thalassemia, and hereditary spherocytosis are well-known causes of moyamoya vessel formation. These anemic disorders are characterized by hemolysis and structural abnormalities of the red blood cell membrane. It has been hypothesized that anemia and abnormal erythrocyte morphology could induce endothelial proliferation, possibly from occluding the vasa vasorum, and progressive narrowing of the major arteries.4,5) Hemolysis may also contribute to endothelial injury and activate oxidative damage through nitric oxide scavenging. The hypoxic state by anemia may compound these effects by promoting the release of proinflammatory and proadhesive mediators, and may inhibit other protective mediators.6)
Pure red cell aplasia is a rare, generally chronic condition of profound anemia characterized by a severe reduction in the number of reticulocytes in the peripheral blood and the virtual absence of erythroid precursors in the bone marrow.7) Usually, it does not accompany hemolysis and abnormal erythrocyte morphology, but the chronic anemia and its corollary hypoxia can induce the development of abnormal vasculature. It is considered as an autoimmune disease that is often refractory; thus, patients with pure red cell aplasia require long-term immunosuppressant treatment with drugs such as cyclosporine, cyclophosphamide, and prednisolone,8,9) which could be a rare cause of quasi-moyamoya disease.10) Considering these predisposing conditions, our patient should be categorized as quasi-moyamoya disease, although pure red cell aplasia has never been reported with moyamoya disease.
Revascularization surgery is recommended for patients with moyamoya disease especially in ischemic cases,11) and it is also recommended for those with quasi-moyamoya disease.3) Surgical procedures for moyamoya disease can be classified into two categories: direct and indirect revascularization, which are performed in various combinations. Direct anastomosis can augment the blood flow from the moment the anastomosis is established, whereas indirect anastomosis can cover a large area and can develop according to the demand for the blood flow. Indirect anastomosis requires at least two processes, angiogenesis and arteriogenesis.12,13) Angiogenesis is the generation of new vessels in the newly formed connective tissue between the pediculate donor tissues and arachnoid membrane.14) This fibrous coat consists mainly of a matrix of collagen fiber, fibroblast, and macrophages, and as a result, angiogenesis resembles wound healing associated with the repair processes. Arteriogenesis is the remodeling of pre-existing interconnecting arterial networks, which results from a pressure gradient. Thus, the extended area of revascularization depends largely on the degree of the hypoperfusion of the cortex.13) In adult patients, the efficacy of the indirect anastomosis is ambiguous, and it has been reported that indirect anastomosis does not develop collateral pathways in about 40% to 50% of adult patients, while indirect anastomosis does provide extensive collaterals in pediatric patients.15,16)
In our patient, the cerebral infarction was presumably induced by the poor perfusion due to moyamoya disease and also by hypoxic state due to anemia caused by pure red cell aplasia. To prevent further ischemic strokes, surgical revascularization seemed beneficial in addition to other medical treatments, such as transfusion and immunosuppressant therapy. The drugs for pure red cell aplasia have multiple anti-inflammatory properties,17) inhibiting cell chemotaxis, activities of vascular endothelial cells, proteolytic activities, and plasminogen activator. As a result, they represent anti-angiogenic effect by inhibiting immunologically mediated neovascularization as well as disrupting fully formed capillaries in vivo and in vitro.18–20) Therefore, we were concerned that they might prevent both angiogenesis and induction of an indirect anastomosis. That is one reason why we recruited direct bypass in this case.
Contrary to our expectations, however, the follow-up angiography showed that collateral vessels had developed from the middle meningeal artery (MMA) and the OA as a result of EDAMS. There was severe hypoperfusion in the patient’s left hemisphere, as was revealed preoperatively using SPECT. Thus, the large CBF demand may have helped in the formation of the indirect anastomosis, or the doses of prednisolone and cyclosporine were insufficient to inhibit the formation of an indirect anastomosis. On the other hand, it is unclear why the direct anastomosis donor vessels, which were well depicted in postoperative MRA, decreased in caliber, as revealed using DSA. Development of indirect bypass might have diminished the demand for the direct bypass.
Combined anastomosis surgery to treat a patient with quasi-moyamoya disease associated with pure red cell aplasia is efficacious. Administration of the steroids or immunosuppressant agents did not affect the neovascularization of indirect anastomosis in this patient.
The authors have no personal, financial, or institutional interest in any of the drugs, materials, or devices in the article. All authors who are members of The Japan Neurosurgical Society (JNS) have registered online Self-reported COI Disclosure Statement Forms through the website for JNS members.