2015 Volume 2 Issue 1 Pages 9-11
2015 Volume 2 Issue 1 Pages 9-11
Bow Hunter’s syndrome is an unusual symptomatic vertebrobasilar insufficiency resulting from intermittent mechanical compression of the vertebral artery, and is rarely a trigger for cerebral infarction following thrombus formation on the damaged endothelial vessels (Bow Hunter’s stroke). The authors present an extremely rare case of a 45-year-old man showing Bow Hunter’s stroke due to congenital vertebral artery fenestration stretching and sliding between C1 and C2 after head rotation to the right. Congenital vertebral artery anomaly rarely causes cerebral infarction, but could cause embolic strokes by mechanical stretching without bony abnormalities.
Bow hunter’s syndrome is defined as symptomatic, vertebrobasilar insufficiency caused by mechanical occlusion of the vertebral artery (VA) at the atlanto-axial level during head rotation, and was coined by Sorensen in 1978.1) It is generally associated with hemodynamic changes, often leading to vertigo and faintness.2) This condition sometimes causes artery-to-artery embolism due to endothelial damage by osseous process or thick fibrous band surrounding the VA at occipital/C1 or C1/C2, which is called Bow hunter’s stroke.3–10) We herein present an extremely rare case showing Bow hunter’s stroke due to stretching and sliding of the VA fenestration between C1 and C2, and discuss its clinical implications with a literature review. To our knowledge, this is the first report of Bow hunter’s stroke associated with stretching and sliding of a congenital VA fenestration without bony abnormalities.
A 45-year-old man complained of repeated vertigo associated with head rotation to the right for 2 years. Magnetic resonance imaging (MRI) previously revealed multiple cerebellar infarctions, and the patient was transferred to our institute for further examination and treatment since the etiology of stroke was not clear. On admission, his physical and neurological examination showed no abnormalities. MRI showed multiple acute infarctions in the bilateral cerebellar hemispheres (Fig. 1). Magnetic resonance angiography and computed tomography angiography (CTA) showed no apparent stenosis or vessel occlusion in the posterior circulation, and only showed congenital anomalies including VA fenestration on the left side and the persistent first inter-segmental artery (FIA) on the right side. We further performed dynamic rotational angiography to assess the possibility of Bow hunter’s stroke. Interestingly, digital subtraction angiography (DSA) showed segmental elongation of the lower limb of the left VA fenestration (Fig. 2A), with a focal defect of the contrast media in the early phase and delayed pooling of the contrast media after head rotation to the right (Fig. 2B). Moreover, CTA clearly showed marked stretching and sliding of the left VA fenestration, and the lower limb was compressed between the C1 transverse process and C2 lateral mass in head rotation to the right (Fig. 3). We concluded that rotational stretching and sliding of the left VA fenestration contributed to this multiple cerebellar infarction, with endothelial damage and mural thrombus formation in the lower limb. After 38 days from last stroke, the patient underwent C1/C2 posterior fusion using C1/C2 transarticular screws and bone graft for prevention of further stroke. Postoperative course was uneventful and there was no longer compression of the inferior limb of the VA between C1 and C2 during head rotation after the surgery (Fig. 4). No symptoms or recurrent stroke have been observed in the patient to date, 24 months after the surgery.
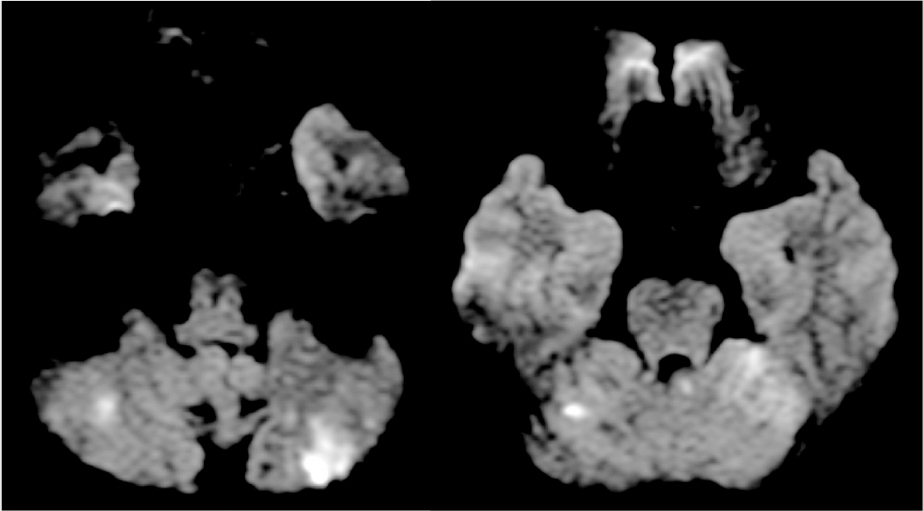
Diffusion weighted magnetic resonance imaging showing multiple fresh infarct spots in both cerebellar hemispheres.
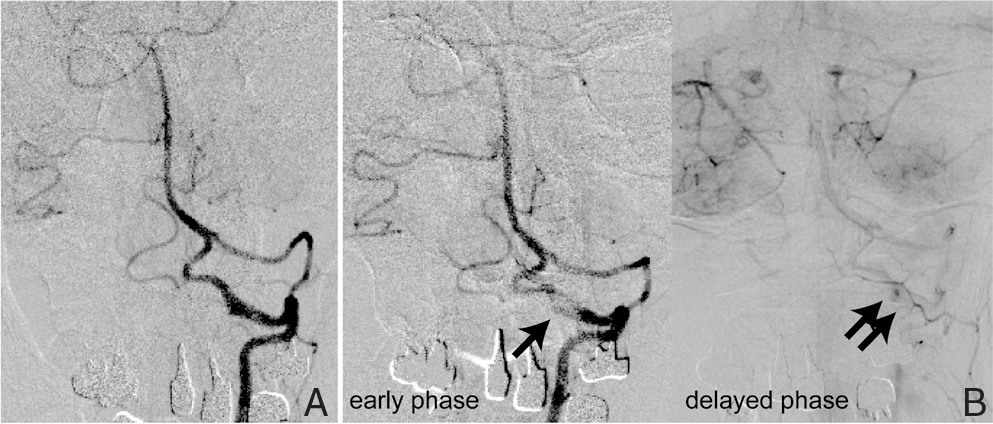
Left vertebral artery angiogram showing segmental elongation of the lower limb of the left VA fenestration (A), which showed a focal defect of the contrast media in the early phase (arrow) and delayed pooling of the contrast media (double arrows) after head rotation to the right (B).
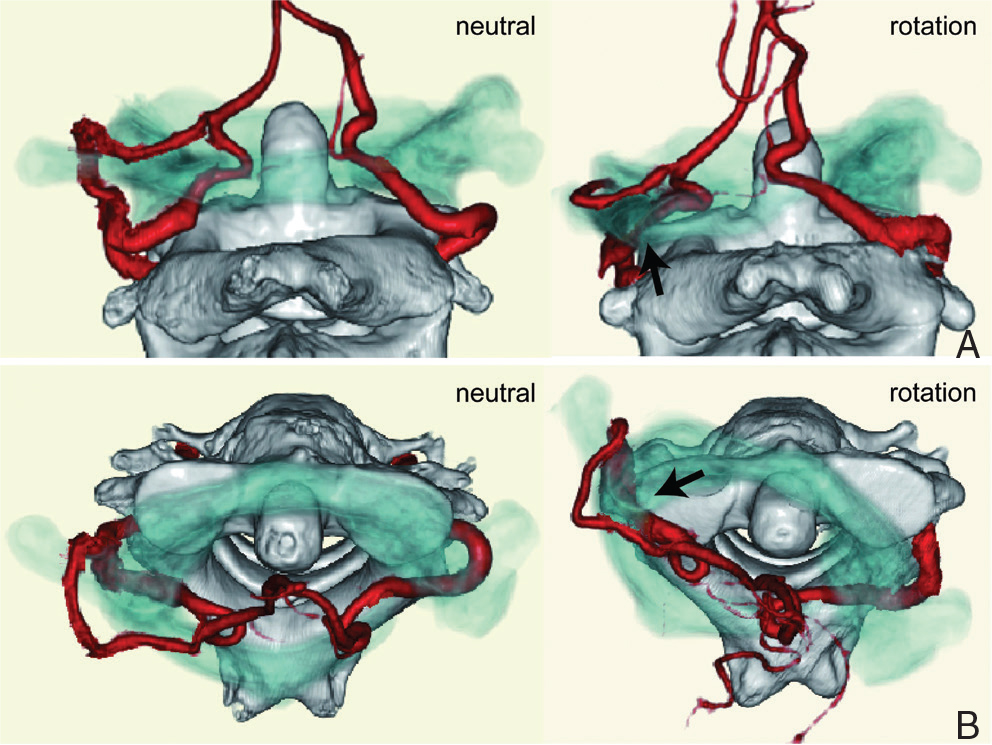
Computed tomographic angiogram (A: posterior to anterior view, B: axial view) showing the marked stretching of the left VA fenestration, and the lower limb was compressed between C1 transverse process and C2 lateral mass in head rotation to the right (arrow). Note that bony structure of C1 is a translucent image (blue) so that it enables to view the VA stretching clearly.

Postoperative computed tomographic angiogram (A: posterior to anterior view, B: axial view) showing that the lower limb of VA was no longer compressed between C1 transverse process and C2 lateral mass in head rotation to the right (arrow). Note that bony structure of C1 is a translucent image (blue).
According to a previous report, congenital anomaly of VA at the C1/C2 level has three types: VA fenestration, persistent FIA, and posterior inferior cerebellar artery of C1/C2 origin.11) These congenital VA anomalies were found in 2.3–5.4% of patients.11–13) Extracranial VA fenestration is a well-known variation and most frequently seen at a C1/C2 level. This VA fenestration contains two limbs, an upper limb running between occipital bone and C1, and a lower limb running between C1 and C2, which was observed in 0.5–0.9% of patients.12,13) This is a very rare case showing both unilateral VA fenestration and contralateral persistent FIA, which is reported in 0.1% of patients.12) These VA anomalies are mostly found incidentally, especially in the examination of cervical spinal disorder.12–15) These VA anomalies are usually asymptomatic,13) although some authors have reported an associated aneurysm and subarachnoid hemorrhage.15–17)
II. Etiologies of strokeWe provided details of eight case reports showing Bow hunter’s stroke (Table 1).3–10) Interestingly, Bow hunter’s stroke occurred at a relatively younger age (mean 24.4 ± 7.2 years old), indicating that aging-related vessel change or bony change does not always contributed to Bow hunter’s stroke, contrary to expectations. Moreover, all the cases had associated bony abnormalities including congenital anomaly. In all the cases, the mechanism for Bow hunter’s stroke is reported as a compression or occlusion of the VA due to osseous process in head rotation. Interestingly, this case has some unique characteristics, which have not been reported so far. First, the patient had no existing bony abnormalities compressing the VA. Second, the patient had a congenital vessel anomaly affecting the Bow hunter’s stroke. Some reports showed mobile mural thrombus in the damaged vessel due to repeated VA compression by head rotation.7,10) This case also supports the mechanism of Bow hunter’s stroke as mural thrombus. MRI showed multiple infarcts in the area of the posterior circulation indicating embolic stroke. Further, DSA showed pooling of the contrast media in lower limb indicating endothelial damage. Stroke occurred at a middle age in this case and cervical spine radiographs showed no atlanto-axial instability or cervical spondylosis (Fig. 5).

Lateral cervical spine radiograph showing no atlanto-axial instability or cervical spondylosis. (A: neutral view, B: extension view, C: flexion view.)
| Author (year) | Age, sex | Location | Associated bony abnormality | Associated vessel abnormality | Mechanism | Treatment |
|---|---|---|---|---|---|---|
| Shimizu et al. (1988)9) | 37, M | Occipital-C1 | Thickened membrane | None | Compression and occlusion of VA | Surgical decompression |
| Tominaga et al. (2002)10) | 34, M | Occipital-C1 | Osseous process | None | Compression and occlusion of VA | Surgical decompression |
| Lu et al. (2009)6) | 12, M | Occipital-C1 | Osseous process | None | Compression and occlusion of VA | Surgical decompression |
| Greiner et al. (2010)5) | 15, M | Occipital-C1 | Osseous process | None | Compression of VA | Surgical decompression |
| Saito et al. (2010)7) | 7, M | C1-C2 | Atlantoaxial subluxation | None | Compression of VA | C1-C2 fusion |
| Sakamoto et al. (2011)8) | 16, M | Occipital-C1 | Occipitalization of atlas | None | Compression of VA | Endovascular VA occlusion |
| Andereggen et al. (2012)3) | 66, M | C5-C6 | Osseous process | None | Compression of VA | Surgical decompression |
| Cornelius et al. (2012)4) | 8, M | C1-C2 | C1-C2 bony malformation | None | Compression and occlusion of VA | Surgical decompression |
| Present case | 45, M | C1-C2 | None | VA fenestration | Stretching and sliding of VA | C1-C2 fusion |
VA: vertebral artery.
The rotational movement in lower cervical vertebrae is limited due to degenerative changes caused by aging. By this limitation, excessive rotation in atlanto-axial joint is forced and lead to the stress of surrounding structure including ligaments.18) In our case, excessive rotation stretched VA, and this VA was compressed between C1 posterior arch and C2 lateral mass because of narrowing the space caused by excessive rotation. Repeated compression also causes sclerotic changes of VA.10) This stretching and compression damaged the intima of the sclerotic VA.
Regarding treatment strategies for Bow hunter’s stroke, surgical decompression such as C1/C2 fusion or endovascular VA occlusion was reported.3–10) In the present study, we performed C1/C2 fusion and the postoperative course was uneventful. Endovascular occlusion of the lower limb of VA is less invasive and could be a favorable option, but remains unclear whether an occluded vessel with coils remains stable against remaining repeated compression. Further accumulation of new cases is required to discuss the treatment option.
To our knowledge, this is the first report of Bow hunter’s stroke associated with stretching and sliding of the congenital VA fenestration between C1 and C2. This case indicates that patients with VA fenestration have a risk of cerebral infarction due to stretching and sliding into bony structures.
None.