2014 Volume 2 Issue 3 Pages 85-87
2014 Volume 2 Issue 3 Pages 85-87
A 44-year-old male with Aarskog syndrome (AS) presented with subarachnoid hemorrhage secondary to ruptured posterior communicating artery aneurysm. AS, also known as faciogenital dysplasia, is an X-linked, autosomal dominant or autosomal recessive congenital developmental disorder. This syndrome is characterized by short stature in association with a variety of multiple anomalies in musculoskeletal, neurological, and urogenital systems. Cerebrovascular abnormalities such as anomalous cerebral venous drainage, dysplastic internal carotid artery, and basilar artery malformation have been reported to be associated with AS. To our knowledge this represents the first case of a ruptured intracranial aneurysm in a patient with AS.
Aarskog syndrome (AS), also known as faciogenital dysplasia, was first described by Dagfinn Aarskog, a Norwegian pediatrician in 1970.1) With an X-linked dominant or recessive inheritance pattern, AS is characterized by short stature in association with a variety of structural anomalies including characteristic craniofacial appearance, typical shawl scrotum, cryptorchidism, musculoskeletal, and neurological anomalies. The spectrum of AS includes behavioral problems in addition to abnormalities in teeth, eyes, and congenital heart defects. A significant amount of attention has been recently placed on investigating the association between vascular anomalies and AS. Various reports describe the occurrence of AS in association with congenital heart and cardiovascular conditions such as atrial and ventricular septal defects, coarctation of the aorta, aortic valve stenosis, aortic root dilatation, and sub-valvular aortic stenosis.2) Additionally, association of AS with neuro-ophthalmological and cerebrovascular anomalies has been previously reported.3–6) There have been no reports of intracranial aneurysms (IAs) occurring in association with AS. Here, we report the very first case of a posterior communicating artery (Pcom) aneurysm presenting with subarachnoid hemorrhage (SAH) in a 44-year-old male with AS.
A 44-year-old male presented with a severe headache to a local hospital in July of 2012. He was a non-smoker with no history of hypertension, alcohol, or drug abuse nor had he a family history of IAs or connective tissue disorders. He had been evaluated and diagnosed with AS during his childhood at a clinical genetics center of the University of Wisconsin-Madison. He had a history of surgical repair for bilateral cryptorchidism. His facial appearance was characterized by a round face, broad nasal bridge, and stubby nose with anteverted nostrils, widow’s peak hair anomaly, fleshy ear lobes, higher arched palate, thickened and down turned superior helices, dental malocclusion, micrognathia, hypertelorism, and ptosis (Fig. 1a, b). He also had classic musculoskeletal manifestations of AS such as short stature with broad hands, brachydactyly, cutaneous syndactyly (Fig. 1c), and short toes. He was found to have an overriding scrotum and hypospadias on genitourinary examination.

Photograph demonstrating characteristic craniofacial appearance of the patient, a round face, broad nasal bridge, and stubby nose with anteverted nostrils, widow’s peak hair anomaly, micrognathia, and hypertelorism (a and b). Characteristic broad hands, brachydactyly, cutaneous syndactyly of the patient (c).
On arrival to the hospital, his examination and initial computed tomography (CT) revealed a diffused SAH (Fig. 2a).7,8) On neurological examination, he was intubated and was localizing pain but was not following commands. Further work-up with computed tomography angiography (CTA) revealed a 5-mm Pcom aneurysm (Fig. 2b, c).

Computed tomography scan of the head demonstrating diffuse subarachnoid hemorrhage and enlarged lateral ventricles (a). Computed tomography angiography (CTA) of the head (b) and CTA with three-dimensional reconstruction (c), demonstrating an irregular saccular aneurysm (arrows) at the origin of the right posterior communicating artery that measures approximately 5 mm in greatest dimension and 3 mm at its base.
The patient underwent clip-occlusion of the Pcom aneurysm via right pterional craniotomy. Of note, there was no exceptional fragility of the extra- or intracranial vasculature as seen in some other connective tissue disorders. Postoperative angiogram showed the complete occlusion of the aneurysm with preservation of the Pcom artery (Fig. 3). The postoperative period was uneventful and the patient eventually regained his consciousness and extubated. The patient’s neurological condition kept improving and two weeks after surgery he was discharged to rehabilitation center. He was neurologically intact and able to return to his work. Postoperative follow up angiogram within 1 year showed no recurrent or residual aneurysm and no formation of de novo aneurysm.
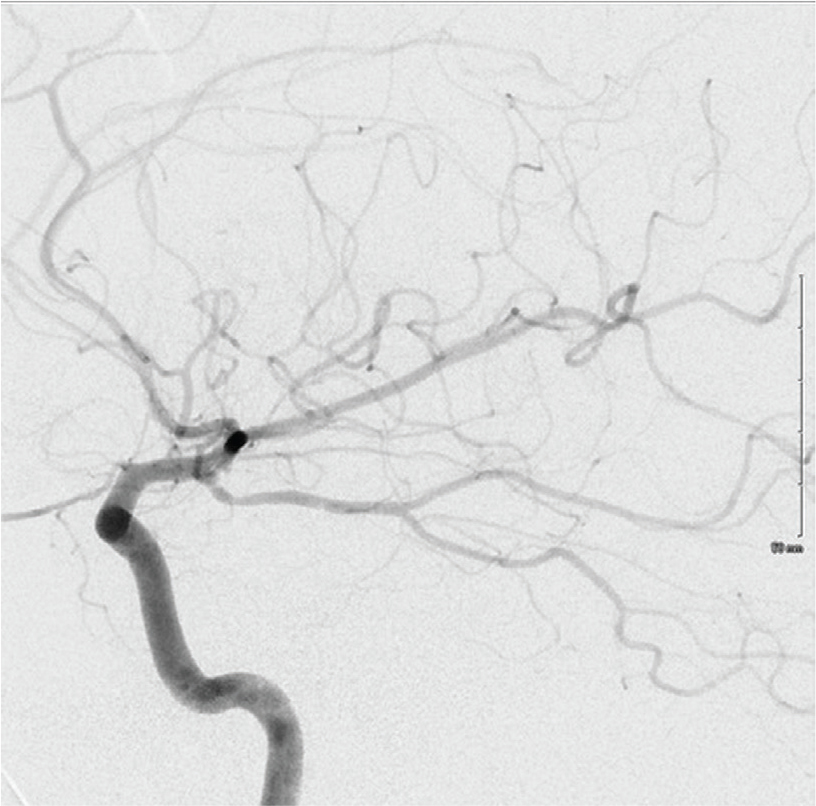
Postoperative digital subtraction angiography showing obliteration of the aneurysm without residual filling along with preservation of the posterior communicating artery.
In 1970, Dagfinn Aarskog reported a familial syndrome of short stature associated with facial dysplasia and genital anomaly, which later became known as AS.1) AS is thought to be genetically heterogeneous with X-linked recessive, autosomal dominant, or autosomal recessive inheritance patterns.9–13) More recently, faciogenital dysplasia 1 (FGD1) gene mutations on Xp11.21 have been shown to be associated with AS.14) This gene encodes a guanine nucleotide exchange factor for guanosine triphosphate (GTP)-binding proteins which are involved in cytoskeletal organization, skeletal formation, and morphogenesis.15) More than 15 mutations of FGD1 gene have been reported in AS.16,17) However in a Chinese family with several members having manifestations of AS and different limb anomalies with additional characteristics, FGD1 gene sequencing and linkage analysis failed to identify an FGD1 mutation suggesting a second locus for this condition.18) We were unable to obtain genetic testing in our case since the patient refused to get tested.
The major craniofacial manifestations of AS are round face, maxillary hypoplasia, broad nasal bridge, stubby nose with anteverted nostrils, long philtrum, widow’s peak hair anomaly, fleshy ear lobes, higher arched palate, thickened and down-turned superior helices, dental malocclusion, micrognathia, hypertelorism, and ptosis.16,19,20) Musculoskeletal manifestations of AS including short and broad hands, cutaneous syndactyly, short toes, short stature, and pectus excavatum were apparent in our case.19,20) All characteristic musculoskeletal anomalies of AS were also apparent in our case. Pathognomonic urogenital anomalies of AS such as cryptorchidism, overriding scrotum, and hypospadias were found in our case as well.6,16,19,20)
Only few cerebrovascular anomalies with AS have been reported, including retinal venous tortuosity,3,4) an anomalous cerebral venous drainage,5) and dysplastic right internal cerebral artery in association with basilar artery malformation.6) Diluna et al.6) reported a 13-year-old male with headache, anorexia, and concentration difficulties. In this report,6) while the authors suspected an aneurysm because of a hyperintense mass in magnetic resonance (MR) angiography conventional angiogram did not reveal any aneurysm.
Elasticity and stability of intracranial arteries originates from the extracellular matrix of the arterial wall of which impairment is a prominent factor in the IAs development.21–23) Strong association of the IA with some of the inheritable connective tissue diseases has been reported, including Ehlers-Danlos syndrome Type IV, Loeys-Dietz syndrome, Marfan’s syndrome, neurofibromatosis Type 1, pseudoxanthoma elasticum, and autosomal dominant polycystic kidney disease.24,25) Multiple IAs in younger ages are expected in patients with the inheritable connective tissue diseases, however, there are reports of single lesions found in older ages.22,26)
Evaluation of candidate genes identified on the basis of function or through prior linkage analysis (positional candidate genes), which are suspected of being involved in the disease, can be performed by association studies. Whole exome sequence analysis has the capability to identify DNA sequence coding variants which may contribute to pathogenicity for IA. Variants identified need to be evaluated further to demonstrate pathogenicity. Genome-wide linkage studies in families and sib pairs with IAs have detected several loci on chromosomes.21) Four loci (1p34.3–p36.13, 7q11, 19q13.3, and Xp22) have been reported to be reproducible in different populations although locus 7q11 was not confirmed in all evaluated populations.27) An association between IA and positional candidate genes have also been demonstrated for the perlecan locus in the 1p34.3–p36.13 region and for collagen type 1 A2 gene locus in 7q11 region.27) FGD1 has been hypothesized to play a role in endothelial cell repair, which could provide an explanation for the aneurysm observed in the patient reported in this paper and may contribute to vascular disorders at the population level.28)
So far there has not been any report of IA and SAH in conjunction with AS. In this case, the association of these conditions may be coincidental and additional reports are necessary to confirm an association between these two conditions. Our experience indicates that IAs should be considered in any patient with AS presenting with headache or any other complaints that make us suspicious of SAH diagnosis. Moreover we did not experience fragility of intracranial vasculature during surgery in our case which is a common feature of other connective tissue disorders in association with IAs. Based on this case, we suggest that vascular pathologies associated with AS can be dealt safely with invasive procedures such as clipping or coiling.
The authors report no conflicts of interest.