2014 Volume 2 Issue 3 Pages 88-92
2014 Volume 2 Issue 3 Pages 88-92
A 69-year-old man consulted our department regarding further examination because abnormal venous ectasia of the basal vein of Rosenthal (BVR) was accidentally found on magnetic resonance imaging. Angiography revealed a dural arteriovenous fistula (DAVF) in the left sphenoid wing; the fistula was supplied by the ophthalmic artery and the middle meningeal artery. Venous drainage from the fistula consisted of a large collector vein located in the temporal tip, which drained into the BVR. We selected open surgery because this lesion may be difficult to access and is associated with significant risks through an endovascular approach. After temporal clip ligation of the drainer, the superficial middle cerebral vein became the main drainage route directly in connection with the fistula. Therefore, both were ligated, after coagulation of feeding arterial networks on the dura around the sphenoid wing. The patient experienced no complications from the surgical procedure, and postoperative angiography demonstrated obliteration of the fistula. DAVF in the sphenoid wing with deep drainage is believed to carry a high risk of hemorrhage or venous infarction because of the presence of Galenic drainage, varix, and cortical venous reflux. Treatment is strongly recommended even if the symptoms are minimal. Open surgery appears to be safe and often the best therapeutic option.
Dural arteriovenous fistulas (DAVFs) in the sphenoid wing are rare1–4) and can be easily confused with other types of DAVF in the middle cranial fossa, partly because of the complexity of the anatomical nomenclature.1,2) Most sphenoid wing DAVFs are fed by the middle meningeal artery (MMA) and drain into the sphenoparietal sinus and/or the superficial middle cerebral vein (SMCV).2,4) Here we describe a case of DAVF in the sphenoid wing draining via the bridging anterior temporal vein (BATV) into the basal vein of Rosenthal (BVR) and the vein of Galen; we successfully treated this patient with craniotomy. The anatomical features and treatment strategies in this region, in the presence of a unique drainage pattern, are discussed based on a literature review.
A 69-year-old man consulted our department regarding further examination because cerebrovascular abnormalities were accidentally found during a medical checkup of the brain (brain dock). He did not have any history of head trauma or hypertension. Physical examination yielded completely normal results. Magnetic resonance imaging during the brain dock revealed anomalous venous ectasia of BVR (Fig. 1). Subsequent catheter angiography revealed a DAVF in the left sphenoid wing; the fistula was supplied by direct collateral from ethmoidal branches of the ophthalmic artery (Fig. 2A) and MMA (Fig. 2B). Venous drainage from the fistula mainly consisted of a large collector vein located in the temporal tip (referred to as BATV), draining in an anterograde manner into the BVR and subsequently into the vein of Galen (Fig. 2A, B). Some part of the venous drainage from BATV flowed into the deep middle cerebral vein (DMCV), refluxed into SMCV in the capillary phase, and finally flowed into the cavernous sinus (CS; Fig. 2C). Considering the angiography findings, the venous route may not have been accessible for transvenous embolization (TVE), and the risks of incomplete obliteration or damage to the central retinal artery that are associated with transarterial embolization (TAE) should not be ignored. This lesion may be easily accessible by a usual craniotomy procedure. We decided to proceed with open surgery rather than the endovascular approach. A left-sided frontotemporal craniotomy was performed. After flattening of the sphenoid ridge with the usual drilling procedure, MMA was extradurally interrupted and a dural incision was made. The Sylvian fissure was completely opened. Feeding arterial networks were observed on the dura around the sphenoid wing. In addition, we noticed the large ectatic arterialized BATV from the dural margin of the lesser sphenoid wing (Fig. 3A). Furthermore, the color of SMCV changed to red and blue in lockstep with the heartbeat, pointing to a small amount of cortical venous reflux. When BATV was temporally occluded using a titanium clip, SMCV was expanded and noticeably turned red (Fig. 3B). The sound of the retrograde arterial flow in the SMCV could be detected using Doppler ultrasound. After BATV and the connection between SMCV and the fistula were temporally occluded, SMCV finally shrank and returned to normal color. Accordingly, both were ligated after coagulation of feeding arterial networks on the dura around the sphenoid wing (Fig. 3C). Postoperatively, the patient experienced no complications from the surgery. Postoperative angiography demonstrated obliteration of the fistula (Fig. 4A, B), and the drainage flow direction of SMCV was diverted from CS to DMCV, subsequently flowing into BVR (Fig. 4C).

Preoperative T2-weighted magnetic resonance imaging revealing aberrant venous ectasia of the basal vein of Rosenthal.
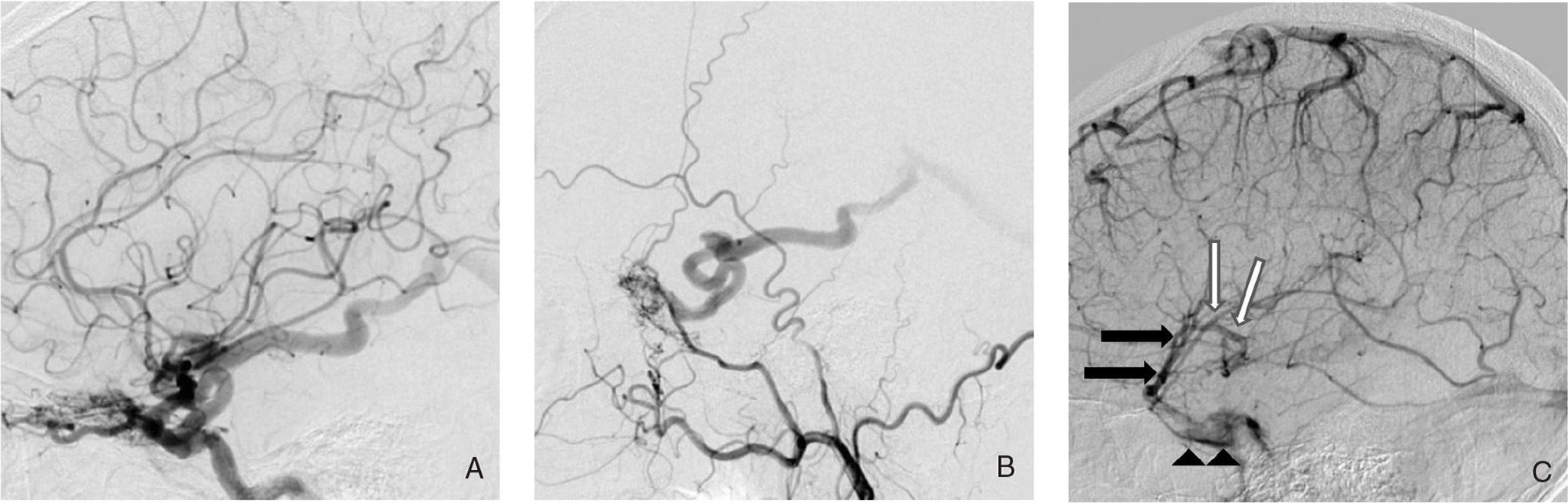
Angiographic images (lateral view). A: Preoperative left internal carotid angiography (ICAG) showing the dural arteriovenous fistula (DAVF; in the left sphenoid wing) fed by ethmoidal branches of the ophthalmic artery (OA). B: Preoperative left external carotid angiography (ECAG) showing DAVF fed by the middle meningeal artery (MMA). The main drainer of DAVF is the bridging anterior temporal vein (BATV) draining in an anterograde manner into basal vein of Rosenthal (BVR) and subsequently into the vein of Galen. C: Preoperative left ICAG in the venous phase demonstrating the superficial middle cerebral vein (SMCV, black arrows), deep middle cerebral vein (DMCV; white arrows), and cavernous sinus (CS, arrowheads). There is a retrograde flow into SMCV through DMCV. SMCV drains into the CS.
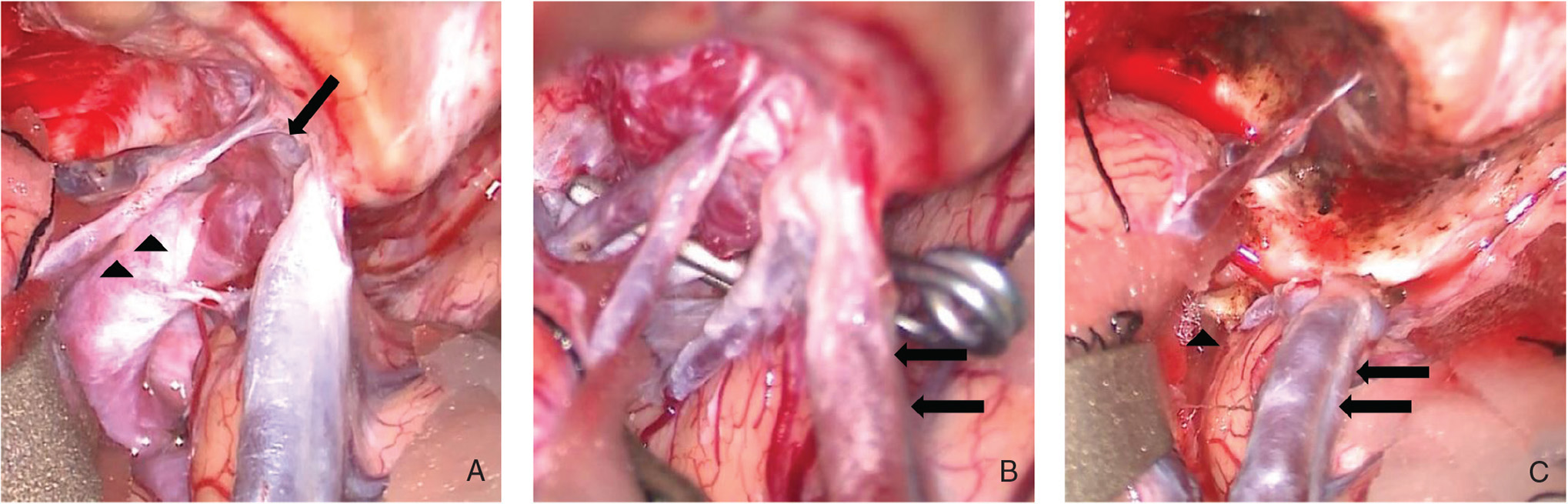
A: An intraoperative photograph of a fistula location in the sphenoid wing (arrow) and the ectatic arterialized bridging anterior temporal vein (BATV; arrowheads). B: An intraoperative photograph showing clip ligation of BATV. Superficial middle cerebral vein (SMCV; arrows) expanded and turned red. C: A photograph after surgical obliteration of dural arteriovenous fistula (DAVF) demonstrated the disconnected BATV (arrowhead) and SMCV (arrows). Feeding arterial networks on the dura around the sphenoid wing are coagulated. SMCV returned to normal color.

A, B: Angiographic images (lateral view). Postoperative internal carotid angiography (ICAG; panel A) and external carotid angiography (ECAG; panel B) revealing disappearance of the dural arteriovenous fistula (DAVF). C: Postoperative ICAG in the venous phase showing the superficial middle cerebral vein (SMCV; black arrows), deep middle cerebral vein (DMCV; white arrows), and the basal vein of Rosenthal (BVR; arrowheads). The drainage flow of SMCV is diverted from cavernous sinus to DMCV, subsequently flowing into BVR.
DAVF in the sphenoid wing with deep venous drainage is rare.1,2) To the best of our knowledge, only eight cases including ours have been reported in the literature (Table 1).1–3,5–8) All cases involved middle-aged men, from 40 years to 69 years of age. These fistulas are fed by the meningeal branch of the external carotid artery (MMA, the accessory meningeal artery, and the artery of the foramen rotundum) and the meningeal branch from the internal carotid artery (the recurrent meningeal branch of the ophthalmic artery, the meningohypophyseal trunk, and the inferolateral trunk). The venous side of these fistulas showed the presence of cortical venous reflux in all cases. In addition, large venous ectasia or varix has been noted in seven cases (7/8, 87.5%). Description of anatomical features of the deep venous drainage appears to be ambiguous or inaccurate in some cases probably because of the complexity of the anatomical nomenclature. Clinical manifestations include ptosis,5) global amnesia,6) headache,7) visual field defects,1,2,8) dizziness,3) and asymptomatic course (our case). Although none of these patients exhibited aggressive presentation, such as intracranial hemorrhage or progressive neurological deficits, treatment is strongly recommended because of the presence of Galenic drainage, varix, and cortical venous reflux.1–9) The eventual curative treatment was a surgical procedure in three cases, TAE + surgery in two, TAE + TVE in two, and TAE in one. Good results were obtained in all cases.
| Author (year) | Age / sex | Symptom | Arterial supply | Venous drainage | Treatment | |||
|---|---|---|---|---|---|---|---|---|
| ICA | ECA | Pattern | Cortical veins | Varix | ||||
| Thompson et al. (1994)5) | 44 / M | ptosis | MHT | MMA | BVR, SMCV | yes | no | TAE + surgery |
| Ezura et al. (1996)6) | 40 / M | global amnesia | OA | MMA | BVR, SPS, Labbe | yes | yes | TAE + surgery |
| Rezende et al. (2006)7) | 45 / M | headache | OA, MHT | MMA, AMA, FRA | BVR, SMCV, CS, SPS | yes | yes | TAE (Onyx) |
| Tanaka et al. (2012)8) | 61 / M | quadrianopsia | MHT | MMA | BVR, SMCV | yes | yes | Surgery |
| Shi et al. (2013)1) | 62 / M | homonymous hemianopsia | OA, MHT | MMA, AMA, FRA | BVR, SMCV, Trolard, SSS | yes | yes | TAE + TVE |
| Osbun et al. (2013)2) | 55 / M | hemianopsia | OA | MMA | ATV, BVR | yes | yes | Surgery |
| Fukuda et al. (2014)3) | 58 / M | dizziness | OA, MHT, ILT | MMA, AMA, FRA | uncal, BVR, SMCV | yes | yes | TAE + TVE |
| Our case | 69 / M | incidental | OA | MMA | ATV, BVR, SMCV | yes | yes | Surgery |
AMA: accessory meningeal artery, ATV: anterior temporal vein, BVR: basal vein of Rothental, CS: cavernous sinus, ECA: external carotid artery, FRA: foramen rotundum artery, ICA: internal carotid artery, ILT: inferolateral trunk, M: male, MHT: meningohypophyseal trunk, MMA: middle meningeal artery, OA: ophthalmic artery, SMCV: superficial middle cerebral vein, SPS: superior petrosal sinus, SSS: superior sagittal sinus, TAE: transarterial embolization, TVE: transvenous embolization.
DAVF in the lesser sphenoid wing is often considered to be an abnormal connection between MMA and the sphenoparietal sinus.1) However, San Millán Ruíz et al. stated that the sphenoparietal sinus may represent an artificial combination of two venous structures (the parietal portion of the anterior branch of the middle meningeal veins and a dural channel located under the lesser sphenoid wing, the sinus of the lesser sphenoid wing).10) They suggested that SMCV drains into CS or the paracavernous sinus (the laterocavernous sinus or a combination of the sphenobasal and sphenopetrosal sinuses) rather than into the venous structures described here (or sphenoparietal sinus) in association with the sphenoid wing. DAVF in the lesser sphenoid wing could connect through the lesser sphenoid wing sinus, which drains into CS and its efferents. The development of DAVF in SMCV is also possible because of its occasional attachment to the dura overlying the lesser sphenoid wing.7) Based on this, fistulas located under the lesser sphenoid wing can be classified according to the involvement of either SMCV or the sinus of the lesser sphenoid wing. The first step in the therapeutic strategy is the characterization of DAVF because DAVFs involving SMCV are associated with venous hypertension.7)
In our case, parts of the fistula occupy the dura of the lesser sphenoid wing and then predominantly drain into the ectatic BATV through the sinus of the lesser sphenoid wing, and subsequently into BVR (Fig. 5). This drainage pattern is almost identical to the case reported by Osbun and Baltsavias.2,11) The sinus of the lesser sphenoid wing was not opacified (apparently because of local thrombosis, a usually observed finding), and only the ectatic BATV was opacified.11) BATV normally drains into the lesser sphenoid wing sinus (or sphenoparietal sinus).12) Although SMCV initially had a normal drainage pattern in our case, SMCV became the main drainage route in direct connection with the fistula after ligation of BATV. Therefore, our case involved two drainage routes: BATV through the lesser sphenoid wing (primary route) and SMCV in direct connection with the fistula (secondary route), which was not identified at first. These findings should be considered during planning of the treatment. Ligation of BATV may be an incomplete treatment, and the connection between SMCV and the fistula must also be ligated. Postoperative angiography showed that SMCV was draining into BVR through DMCV.
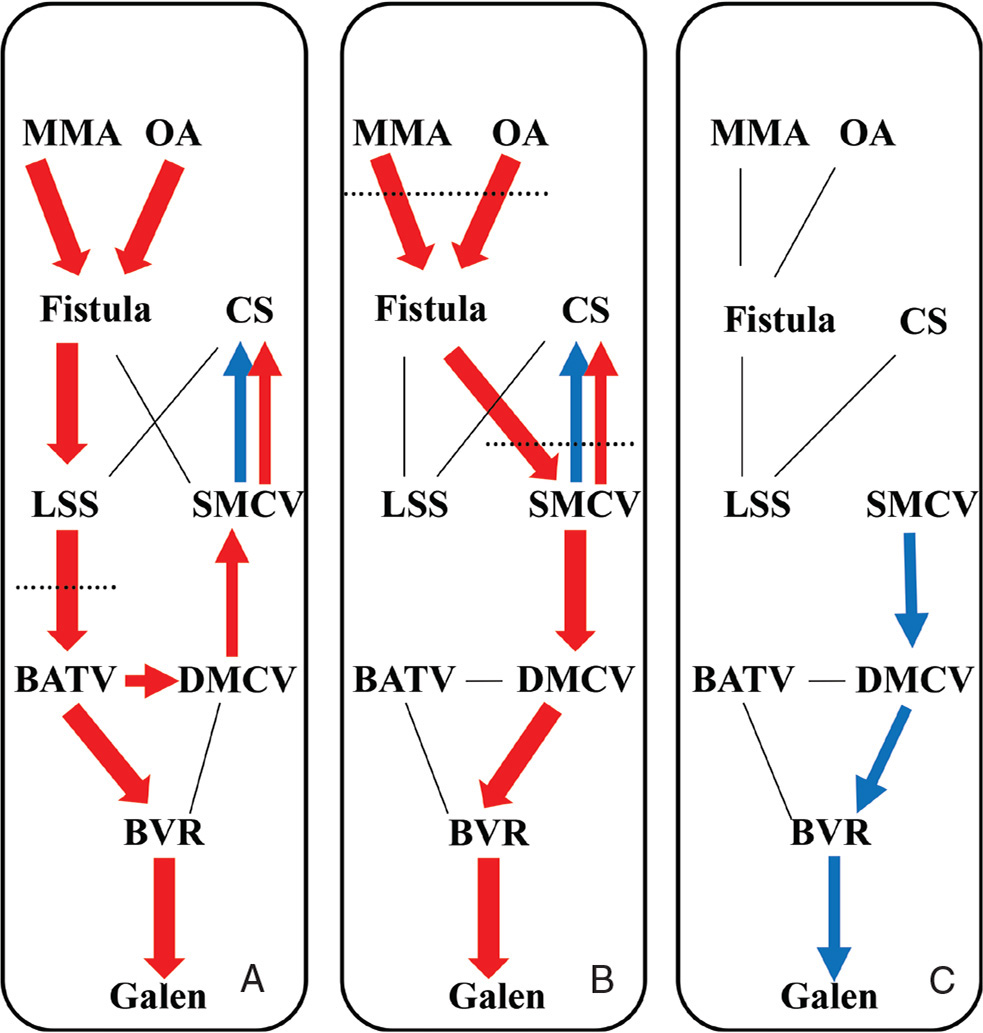
A: Diagram of the venous drainage pattern of our case. B: Diagrammatic representation after the temporal clip ligation of the bridging anterior temporal vein (BATV) showing the secondary superficial middle cerebral vein (SMCV) route. C: Diagrammatic representation after ligation of both the BATV and SMCV routes following coagulation of feeding arterial network demonstrating the final drainage pattern. Red and blue arrow indicates arterial and venous flow, respectively. LSS: lesser sphenoid sinus.
In the current era of the Onyx for curative embolization of DAVFs, TAE of a fistula’s connections is becoming a standard treatment technique.1,7) Flow control using coils or temporary balloon occlusion of the internal carotid artery are necessary for high-flow shunts to decrease the likelihood of distal migration of the embolic material.1,3,7) During embolization of the MMA branches with embolic material, occlusion of the cavernous and petrosal branches may result in ischemic injury of the trigeminal or facial nerves.1,3) TVE continues to be a safe and an effective option if the fistula locations can be approached; however, incomplete fistula occlusion or CS packing alone should be avoided because of the risk of flow diversion into cortical or deep veins.1) Endovascular treatment of DAVF in the sphenoid wing may be considered a satisfactory option if an experienced endovascular neurosurgeon participates in the treatment.
However, open surgery remains a good option for obliteration of DAVF in the sphenoid wing.2,8) We could not detect secondary SMCV routes until SMCV was expanded and turned red after ligation of BATV. Although detection of the full outline of the fistula was difficult with the endovascular route, we could confirm obliteration of the fistula by monitoring the venous color and by means of Doppler ultrasound during the operation. Change of reflux pattern might be observable more accurately and easily by intraoperative angiography or indocyanine video angiography, if possible.
An approach to the sphenoid wing is easy for a general neurosurgeon, and the surgical procedures involved are not difficult. Open surgery is advantageous and is likely to lead to a complete cure of DAVF in the sphenoid wing.