2014 Volume 2 Issue 3 Pages 97-100
2014 Volume 2 Issue 3 Pages 97-100
Basilar artery dissection (BAD) presenting with subarachnoid hemorrhage (SAH) is life-threatening, but its treatment has not been established yet. We treated two patients with ruptured BAD. They were 40-year-old and 41-year-old women. Both of them were treated conservatively during the acute stage. In one patient, radiological abnormality of BAD improved spontaneously. In another patient, reconstructive endovascular treatment (stent with coiling) was required in the chronic stage because the lesion deteriorated morphologically. Neither of them suffered from rebleeding and both had favorable outcome. We reported two patients with ruptured BAD treated conservatively during the acute stage and their outcomes were favorable. We reviewed the literature of BAD presenting with SAH and discussed the management for these lesions.
Basilar artery dissections (BADs) are rare lesions and little is known about its natural history. The clinical presentations of BADs are subarachnoid hemorrhage (SAH), brain ischemia, and brainstem compression. Ruptured BADs presenting with SAH seemed to have higher mortality rate than unruptured ones.1–7) Rebleeding of ruptured BAD leads to poor outcome, and preventive treatment for rebleeding should be performed in the same manner for other intracranial arterial dissections such as vertebral artery dissections (VADs). Although treatment for ruptured VAD is established, treatment for ruptured BAD has not been established. Surgical trapping or endovascular intraluminal occlusion with coiling in the acute stage is the standard therapy for ruptured VAD, but these treatments cannot be applied to ruptured BAD due to inevitable ischemic complications. The other surgical or endovascular therapies for ruptured BAD during the acute stage are hazardous and do not always prevent rebleeding completely.
We report two patients with ruptured BAD. One patient underwent conservative treatment during the acute stage, and the lesion improved spontaneously. Another one was treated conservatively during the acute stage, but reconstructive endovascular treatment (RET), i.e., stent assisted coiling, was required in the chronic stage because the lesion deteriorated morphologically. We review the literature of BAD presenting with SAH and discuss the management for these lesions.
This 40-year-old woman was admitted to another hospital for consciousness disturbance following severe headache and vomiting. On admission, Glasgow Coma Scale (GCS) was 13 and no apparent hemiparesis was observed. Brain computed tomography (CT) showed diffuse SAH mainly in the basal and prepontine cisterns with mild ventricular dilatation (Fig. 1A). Cerebral angiography revealed moderate dilatation of the distal portion of the basilar artery (BA) (Fig. 1B). Under the diagnosis of ruptured BAD, she was treated conservatively with propofol (AstraZeneca, London, England) administration and blood pressure control. She was transferred to our hospital on Day 2 and the same conservative treatment was continued until Day 14. Rebleeding or symptomatic vasospasm did not develop. She had no apparent neurological deficit on Day 20. Three dimensional computed tomography angiography (3DCTA) on Day 20 showed enlarged dilatation of the lesion (Fig. 1C). Although we planned endovascular treatment, 3DCTA on Day 30 revealed improvement of the dilatation (Fig. 1D). The scheduled endovascular treatment was cancelled. She was discharged without any neurological deficit on Day 40. 3DCTA on Day 100 demonstrated normalization of the lesion (Fig. 1E). 3DCTA at 2 years also showed normal BA, and she was working at the previous office.
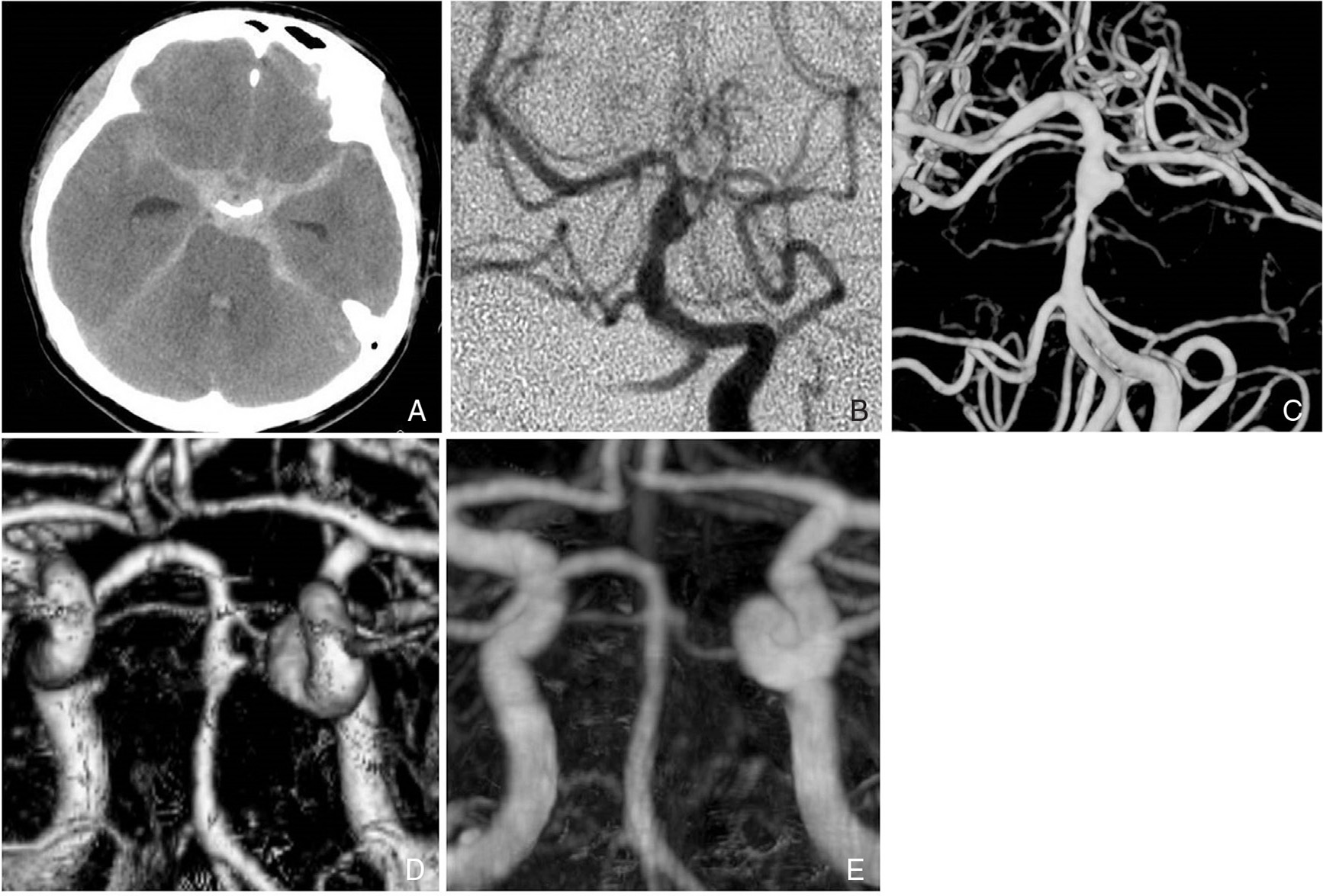
A: Computed tomography (CT) on Day 0 shows diffuse subarachnoid hemorrhage (SAH) mainly in the basal and prepontine cisterns. B: Vertebral angiography (AP view) on Day 0 shows moderate dilatation at the distal basilar artery (BA). C: Three-dimensional computed tomography angiography (3DCTA) (AP view) on Day 20 reveals enlargement of the dilatation at the distal BA. D: 3DCTA (AP view) on Day 40 demonstrates improvement of the dilatation at the distal BA. E: 3DCTA (AP view) on Day 100 shows normalization of the distal BA. AP: anteroposterior.
This 41-year-old woman was admitted to another hospital with restless confusion following severe headache and vomiting. On admission, GCS was 12 and no apparent hemiparesis was observed. CT showed diffuse SAH mainly in the basal and prepontine cisterns with marked ventricular dilatation (Fig. 2A). 3DCTA revealed moderate dilatation of the mid portion of the BA (Fig. 2B). Under the diagnosis of ruptured BAD with acute hydrocephalus, ventricular drainage was performed on the first day. She was treated conservatively with propofol administration and blood pressure control until Day 14. She suffered from no rebleeding or symptomatic vasospasm. 3DCTA on Day 20 showed aneurysmal dilatation of the lesion (Fig. 2C). She was transferred to our hospital on Day 25 for further treatment. On admission to our hospital, she had no apparent neurological deficit. Vertebral angiography also showed the aneurysmal dilatation of the mid portion of the BA (Fig. 2D). Dual antiplatelet premedication (aspirin and clopidogrel) was started on Day 30. Stent assisted coil embolization using Enterprise Vascular Reconstruction Device (VRD) (Johnson & Johnson, Miami, Florida, USA) was performed. Excelsior SL-10 (Stryker, Kalamazoo, Michigan, USA) was first introduced to the aneurysmal dilatation in the mid-BA. Then, Enterprise VRD 4.5 mm × 22 mm was deployed from P1 portion of the left posterior cerebral artery to the lower BA. Then, three coils (Orbit GALAXY, Johnson & Johnson, Miami, Florida, USA and Target 360 ULTRA, Stryker, Kalamazoo, Michigan, USA) were deposited in the lesion (Fig. 2E). Postoperative diffusion-weighted imaging showed small fresh infarction in the right pons and the left cerebellar hemisphere, but she had no neurological symptom. Postoperative course was uneventful and she was discharged without any neurological deficit on Day 60. Dual antiplatelet medication was continued for 6 months, and single antiplatelet medication (clopidogrel) was continued for another 6 months. Cerebral angiography at 1 year showed stable occlusion of the lesion compared to the outcome of the previous endovascular treatment (Fig. 2F), and she currently spends a normal life.

A: Brain CT on Day 0 shows diffuse SAH mainly in the basal and prepontine cisterns and hydrocephalus. B: 3DCTA (AP view) on Day 0 shows moderate dilatation at the mid BA. C: 3DCTA (AP view) on Day 20 reveals aneurysmal dilatation of the lesion. D: Preoperative vertebral angiography (AP view) on Day 30 shows aneurysmal dilatation of the lesion. E: Intraoperative plain X-ray film (AP view) shows the distal marker (arrow) and the proximal marker (short arrow) of Enterprise Vascular Reconstruction Device (VRD). The tail of the last coil is located between a vessel wall and Enterprise VRD (arrowhead). F: Postoperative vertebral angiography (AP view) at 1 year demonstrates disappearance of the aneurysmal dilatation with coiling. 3DCTA: three-dimensional computed tomography angiography, AP: anteroposterior, BA: basilar artery, CT: computed tomography, SAH: subarachnoid hemorrhage, 3DCTA: three-dimensional computed tomography angiography.
Although BAD presenting with SAH is life-threatening, the treatment for these lesions has not been established. Rebleeding of ruptured BAD leads to poor outcome, thus preventive treatment for rebleeding is ideally performed during the acute stage. There are some options for ruptured BAD: conservative therapy, surgical therapy, endovascular therapy, and their combinations.
Including our two cases, 68 BADs presenting with SAH have been reported.1–28) Morphologically, there were 44 dilated lesions, 12 pearl-and-string lesions, 9 stenotic lesions, and 3 completely occluded lesions. In the latter two groups of steno-occlusive lesions (9 stenotic lesions and 3 complete occluded lesions), 10 were treated conservatively and 2 were treated with single stent replacement during the acute stage. None of the patients with steno-occlusive lesions suffered rebleeding. Excluding these 12 stenoocclusive lesions, the remaining 56 ruptured BADs (44 dilated lesions and 12 pearl-and-string lesions) including our 2 cases were further reviewed (Table 1). Two patients (5%) died soon after admission. In 33 patients (59%) of 56 ruptured BADs, surgical or endovascular therapy was performed in the acute stage. Four had surgical wrapping of the lesion, 4 had endovascular flow reversal therapy, 8 had endovascular coiling, and 17 had RET with stentings with or without coiling. Two of 33 patients (6%) with acute surgical or endovascular treatment presented with rebleeding (one with surgical treatment and the other with endovascular flow reversal therapy). Surgically treated patients had poor outcome [GOS: good recovery (GR) 50% (2/4)] and patients with endovascular flow reversal therapy had poor outcome [GOS: GR 50% (2/4)], whereas patients treated with RET had favorable outcome [GOS: GR 88% (15/17)]. The patients with endovascular coiling had good outcome [GOS: GR 75% (6/8)], but recanalization was observed in 2 patients (25%). In 21 patients (38%) of 56 ruptured BADs, conservative therapy was performed during the acute stage. Five of these 21 patients suffered rebleeding, and rebleeding rate of ruptured BAD treated conservatively was 24% (5/21). As for the rebleeding rate, there were no significant differences between dilated lesions and pearl-and-string lesions [dilated lesions: 23% (3/13), pearl-and-string lesions: 25% (2/8), Fisher exact test: P = 0.738]. In 21 conservatively treated patients, 7 had surgical or endovascular treatment in the chronic stage because the lesions deteriorated morphologically and 9 had no further treatment because of stable or improved lesions. As for the clinical outcome of 56 ruptured BADs, 39 patients (70%) were ranked as GR, 3 (5%) as mild disability, 4 (7%) as severe disability, and 9 (16%) as death.
| Baseline characteristics | ||
|---|---|---|
| General | Mean age (years old) | 48.2 (17–78) |
| Woman | 34/56 (63%) | |
| H&K grade | 1 | 6 (11%) |
| 2 | 21 (38%) | |
| 3 | 11 (20%) | |
| 4 | 7 (13%) | |
| 5 | 6 (11%) | |
| n.s. | 5 (9%) | |
| Radiological finding | Dilatation | 44 (79%) |
| Pearl-and-string | 12 (21%) | |
| *Stenotic lesions and complete occluded lesions are excluded in this review. | ||
| Treatment | ||
| Acute stage | None | 2 (5%) |
| Conservative therapy | 21 (38%) | |
| Surgical wrapping | 4 (7%) | |
| Endovascular flow reverse therapy | 4 (7%) | |
| Endovascular coiling | 8 (14%) | |
| RET with stents with or without coiling | 17 (30%) | |
| Chronic stage | Surgical flow reverse therapy | 4 (7%) |
| Surgical clipping | 1 (2%) | |
| Endovascular coiling | 1 (2%) | |
| RET with stents with or without coiling | 1 (2%) | |
| Results | ||
| Rebleeding | Conservative treatment | |
| (dilated lesions) | 3/13 (23%) | |
| (pearl-and-string lesions) | 2/8 (25%) | |
| (total) | 5/21 (24%) | |
| Acute surgical or endovascular treatment | 2/33 (6%) | |
| GOS | Good recovery | 39 (70%) |
| Mild disability | 3 (5%) | |
| Severe disability | 4 (7%) | |
| Vegetative state | 0 (0%) | |
| Death | 9 (16%) | |
| n.s. | 1 (2%) | |
GOS: Glasgow Outcome Scale, H&K: Hunt & Kosnik, n.s.: not specified, RET: reconstructive endovascular treatment, SAH: subarachnoid hemorrhage, VRD: vascular reconstruction device.
The appropriate treatment of ruptured BAD depends on the anatomy of the lesion, and conservative therapy might be suitable for the steno-occlusive lesions. Treatment of the dilated lesions and the pearl-and-string lesions is controversial. According to our review, rebleeding rate of the dilated lesions and the pearl-and-string lesions treated conservatively was relatively high (24%). And the patients with acute surgical therapy had poor outcome, whereas the patients treated with acute RET had favorable outcome. Kim, et al. reported usefulness of acute RET with stenting with or without coiling.3) In their report, 6 of 7 patients with acute endovascular treatment recovered with complete or near-complete healing of the dissection on follow-up angiography. Jiang C, et al reported 18 ruptured BADs treated with acute endovascular therapy.2) In their report, coiling-only therapy without stenting was performed in 8 cases and RET with stenting with or without coiling was performed in 10 cases. Stented cases had better outcome than coiling-only cases and the coiling-only patients had a significantly higher recurrence rate than the patients with stent-assisted treatment. On the other hand, it remains unclear whether treatment should be performed in the chronic stage, when the lesions treated conservatively during the acute stage deteriorated morphologically. According to our review, all such cases underwent treatments in the chronic stage, and both surgically and endovascularly treated patients had good outcome.
Progress of endovascular treatment is ever-improving, and acute endovascular treatment for ruptured BAD becomes safer and more reliable recently. RET with stenting with or without coiling enables treatment of the lesions and preserve blood flow through the parent vessel and is suitable for dilated or pearl-and-string BAD presenting with SAH.
Although acute RET for ruptured BAD should be performed with great care to avoid ischemic complication, RET in the acute stage may be considered as a treatment option for ruptured BADs with high rebleeding risk, such as dilated lesions with bleb or pearl-and-string lesions.2,3)