2016 Volume 3 Issue 4 Pages 129-131
2016 Volume 3 Issue 4 Pages 129-131
We report the case of a 49-year-old man with underlying hypertension who developed diplopia lasting 2 months. Magnetic resonance imaging and digital subtraction angiography showed multi-lobular unruptured aneurysms in the P2 portion of the posterior cerebral artery (PCA) migrating into the interpeduncular cistern of the midbrain. Because the shapes of the aneurysms were serpentine fusiform and the posterior communicating artery (PCoA) was the fetal type, we planned anastomosis of the occipital artery to the P4 portion of the PCA followed by endovascular obliteration of the parent artery including the aneurysms. Endovascular treatment was performed via a femoral approach one week after the anastomosis. Super-selective balloon test occlusion (BTO) of the PCoA was performed by using an occlusion balloon microcatheter before endovascular treatment. Occlusion of the proximal segment of the PCoA induced disturbance of consciousness of the patient. Occlusion of the distal segment other than the first point of the PCoA did not induce any neurological symptoms. The information from this super-selective BTO helped us to perform precise endovascular obliteration. The aneurysm was successfully obliterated, and the diplopia almost disappeared in a few months. Super-selective BTO of the PCoA might be a useful method for preventing ischemic complications due to occlusion of invisible perforators.
Aneurysms of the posterior cerebral artery (PCA) are uncommon lesions accounting for 0.7–2.3% of all intracranial aneurysms.1,2) PCA aneurysms can be treated by both direct surgery and endovascular therapy. Because the proximal segment of the PCA is especially deep in the operative field and close to cranial nerves and perforating arteries, direct surgery has some risks of brain injury due to brain retraction or vascular injury. Endovascular therapy has been developed as a safer and more effective alternative treatment method for PCA aneurysms.3–5) When the aneurysm is treated by occlusion of the endovascular parent artery of the PCA, it still remains controversial whether balloon test occlusion (BTO) of the PCA is necessary or not. Here, we describe the effectiveness of super-selective BTO of the posterior communicating artery (PCoA) in the treatment of a PCA aneurysm with a fetal type PCoA.
This 49-year-old man had been taking medication to treat hypertension for 2 months before the development of diplopia. Because the symptoms were gradually getting worse, the patient was admitted to our hospital. The patient exhibited left oculomotor nerve palsy, which was probably caused by a multi-lobular unruptured aneurysm at the P2 segment of the left PCA. Magnetic resonance (MR) angiography revealed that the aneurysm contacted the midbrain around the origin of left oculomotor nerve (Fig. 1A). The aneurysm had a serpentine, multi-lobular configuration and had no thrombosed component. Digital subtraction angiography showed the aneurysm was approximately 6 mm in diameter. Three-dimensional rotational angiography showed the aneurysm to be of the fusiform type (Fig. 1B, C). Vertebral angiogram under compression of the left carotid artery indicated aplasia of the left P1 segment of the PCA and that blood was supplied to the PCA only through the fetal type PCoA via the ICA (Fig. 1D). Based on these findings, simple internal trapping of the aneurysm had the risk of ischemia of the left occipital lobe. We planned to perform occipital artery (OA) to PCA anastomosis followed by endovascular obliteration of the parent artery including the serpentine fusiform aneurysms.

(A) Magnetic resonance angiography showing an unruptured aneurysm of the left fetal-type posterior cerebral artery (PCA) contacting the midbrain with no thrombosed component. (B) Cerebral angiography showing a 6 mm aneurysm. (C) Three-dimensional rotational angiography showing the fetal type posterior communicating artery (arrow), multi-lobular aneurysms (arrowheads), and distal posterior cerebral artery (asterisk). (D) Vertebral angiography with left carotid compression did not show filling of the left internal carotid artery through the left posterior communicating artery or the left PCA.
The operation was carried out in a prone position under general anesthesia. The OA branches were carefully dissected under a surgical microscope. The OA branches were anastomosed to the calcarine and parieto-occipital arteries of the PCA in an end-to-side fashion. The patency of the anastomosis was confirmed by indocyanine green videoangiography during surgery. The patient underwent endovascular treatment via a femoral approach under local anesthesia 1 week after the anastomosis. The patient was given heparin to achieve a periprocedural activated clotting time of about 250 seconds. Thereafter, the left internal carotid artery was engaged with a 6-Fr ENVOY (Cordis, Miami Lakes, FL) guiding catheter. To prevent the PCoA from mechanical injury, a 4 × 7 mm HyperForm (Covidien/Medtronic, Irvine, CA, USA) highly conformable occlusion balloon microcatheter was chosen and carefully advanced to the main trunk of the PCoA. Because we were not able to confirm the anterior thalamoperforating arteries (ATPAs) by angiography, we did not know where we should perform embolization of the proximal part. When BTO was performed with occlusion of the proximal segment of the PCoA, the patient lost consciousness immediately after inflation (Fig. 2A). Next, we changed the site of BTO. BTO was performed with preservation of blood flow in the proximal segment of the PCoA, and he remained stable and exhibited no neurological deficits for 20 minutes (Fig. 2B). Therefore, we performed proximal occlusion with coils to preserve the proximal portion of the PCoA (Fig. 3A). A left internal carotid angiogram showed successful embolization with no neurological deficit due to the ATPAs and patency of the OA-PICA anastomosis (Fig. 3B). Because there was a stenosis in distal PCoA, we were able to no longer insert a microcatheter (Fig. 3C). The aneurysms were embolized roughly, and the distal part of the PCoA was embolized tightly to improve oculomotor nerve palsy (Fig. 3D). The diplopia improved slightly after the treatment. The patient followed up in our hospital for 6 months following the procedure.
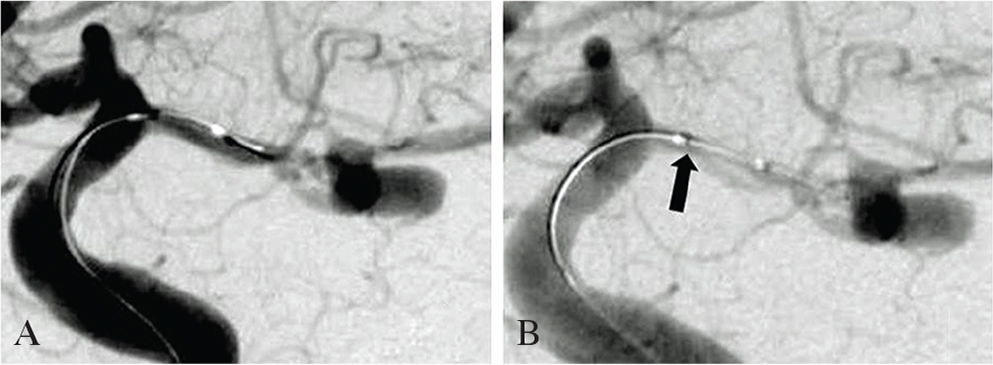
Left internal carotid angiography. (A) Occlusion balloon microcatheter insertion to the origin of the posterior communicating artery (PCoA). The patient had disturbance of consciousness due to occlusion of perforators. (B) Catheter insertion to a depth of 2.0 mm from the origin of the PCoA (arrow). The patient had no neurological symptoms.

(A) Left internal carotid angiography (ICAG) showing the remaining posterior communicating artery (PCoA) (arrowhead). (B) Left external carotid angiography showing good occipital artery patency to the posterior cerebral artery anastomosis. (C) Left ICAG from the cranial angle showing a stenosis at the distal portion of the PCoA (white arrow). (D) Radiogram showing rough packing of the aneurysms and tight packing of just the distal portion of the PCoA.
In the present case, the border of the fetal type PCoA and P2 segment was unclear due to aplasia of the P1 segment. When parent artery occlusion (PAO) was performed for the PCoA-P2 segment, it was difficult to determine where we could perform endovascular obliteration of the proximal part to preserve the perforators of the PCoA. Kim et al. reported that the first arising points of the ATPAs were often within 2 mm of the ICA and rarely located distally such as the distal PCoA or proximal PCA in their series.6) ATPAs supply the mammillary bodies, subthalamus, posterior hypothalamus, anterior thalamus, optic tract, and tuber cinereum. Various neurological symptoms including disturbance of consciousness develop due to occlusion of these perforators.7,8) The ATPAs are important, but these perforators are not often shown by angiography during endovascular treatment. In the present case, we were able to confirm these symptoms by BTO of the PCoA using an occlusion balloon microcatheter before endovascular treatment. This information helped us decide where to perform endovascular obliteration. One limitation of the present case was that only neurological symptoms were checked. If neurophysiological monitoring, such as a somatosensory evoked potential test, would be used for objective evaluation, the BTO of the PCoA might become a more useful examination.
Because BTO sometimes has false positive or false negative results, previous studies reported that BTO was not performed before procedures such as PAO and that PAO was safe for P2 segment aneurysms without any anastomosis surgery.3–5) On the other hand, some studies recommended angiography to find collateral arteries of the ipsilateral ICA after BTO of the PCA and to evaluate whether the collateral supply was enough.9,10) It is controversial whether or not PAO should be performed before anastomosis surgery. We suggested that anastomosis surgery should be considered without BTO to prevent ischemic complications. Super-selective BTO for PCoA has not been reported thus far. In the present case, we were able to evaluate the patency of the anastomosis by performing BTO of the PCoA before PAO. It is well known that the anterior choroidal artery (AChA) could be occluded with none of the classic symptoms due to the anastomosis between the AChA and the lateral posterior choroidal artery.11,12) When BTO of the proximal parent artery was performed, it could be confirmed that the aneurysms were not receiving a retrograde blood supply. This information was useful for preventing ischemic complications and performing complete obliteration of the aneurysms. We suggest that anastomosis patency and hemodynamic changes should be confirmed by using BTO when performing anastomosis surgery followed by PAO.
Therapeutic management for P2 segment aneurysms is conventionally performed with both direct surgery and endovascular treatment. Because the proximal segment of the PCA is especially deep in the operative field and close to the cranial nerves and perforating arteries, direct surgery is challenging and has risks of brain injury due to retraction or vascular injury.13,14) Because of progress in the field of neurointervention, recent reports have suggested that endovascular treatment might be useful for PCA aneurysms.3,5,9,15) Specific thromboembolic events are related to BTO and endovascular treatment. The administration of heparin may help avoid these events. Because of the increased risk of vascular dissection when expanding a balloon in a thin vessel such as the PCoA, super-selective BTO should be performed by experienced specialists. In the present case, serpentine fusiform aneurysms of the PCoA-P2 junction were successfully treated by endovascular treatment with OA-PCA anastomosis. Super-selective BTO of the PCoA might be a useful method for preventing ischemic complications due to occlusion of invisible perforators such as the ATPAs.
The authors declare that there are no conflicts of interest.