2018 Volume 5 Issue 4 Pages 91-94
2018 Volume 5 Issue 4 Pages 91-94
The occurrence of cerebral vasospasm secondary to bacterial meningitis is relatively rare. Furthermore, there is no specific treatment cerebral vasospasm. Endovascular treatment may be essential for cases with the advanced clinical course. Balloon angioplasty or intra-arterial injection of verapamil, nicardipine, or nitroglycerin has been previously reported. We experienced successful treatment using intra-arterial infusion of fasudil hydrochloride. To our knowledge, this is the first case to report the intra-arterial injection of fasudil hydrochloride for treating cerebral vasospasm secondary to bacterial meningitis. A 37-year-old female who presented with dizziness had a right cerebellar tumor that was excised and diagnosed as glioblastoma. On postoperative day 10, Streptococcus oralis meningitis was detected. On postoperative day 20, the patient developed right hemiparesis with a severe vasospasm of the bilateral middle cerebral artery and anterior cerebral artery. Intra-arterial fasudil hydrochloride injection was performed for 3 days, following which the patient’s symptoms improved. Symptomatic cerebral vasospasm secondary to bacterial meningitis is relatively rare and difficult to treat; in selected cases, intra-arterial fasudil hydrochloride injection was an effective treatment for cerebral vasospasm secondary to bacterial meningitis.
The occurrence of cerebral vasospasm secondary to bacterial meningitis is relatively rare compared with that after subarachnoid hemorrhage (SAH). Cerebral vasospasm that concurrently occurs after meningitis is not often detected as promptly as that after SAH, and it can cause severe complications.1) Furthermore, there is no specific and definitive treatment strategy for this condition, and this is similar to SAH. We treated patients with cerebral vasospasm secondary to bacterial meningitis using intra-arterial infusion of fasudil hydrochloride.
A 37-year-old female presented with dizziness. Mild cerebellar ataxia was observed in the right upper limb. MRI revealed an enhanced cystic mass lesion in the right cerebellar hemisphere (Fig. 1A). A gross total tumor excision was performed, the pathological diagnosis was glioblastoma (isocitrate dehydrogenase; wild-type, WHO grade IV). Intraoperative bleeding was not excessive (Figs. 1B and 1C), and the postoperative course was relatively good. However, Streptococcus oralis meningitis was detected on postoperative day 10. Ventricular drainage was performed on postoperative day 17 because of hydrocephalus (Fig. 1D); the meningitis had resolved by antimicrobial therapy. On postoperative day 20, the patient developed consciousness disturbance and right hemiparesis, and diffusion-weighted MRI showed a high-intensity region in the left parietal lobe (Fig. 1E). Magnetic resonance angiography showed poor visualization of bilateral middle cerebral artery and anterior cerebral artery (Fig. 1F), which was consistent with severe vasospasm by digital subtraction angiography (Figs. 2A and 2B). Fasudil hydrochloride (Asahi Kasei Corp., Tokyo, Japan) was intra-arterially administered to preserve antegrade blood flow and prevent further infarction.
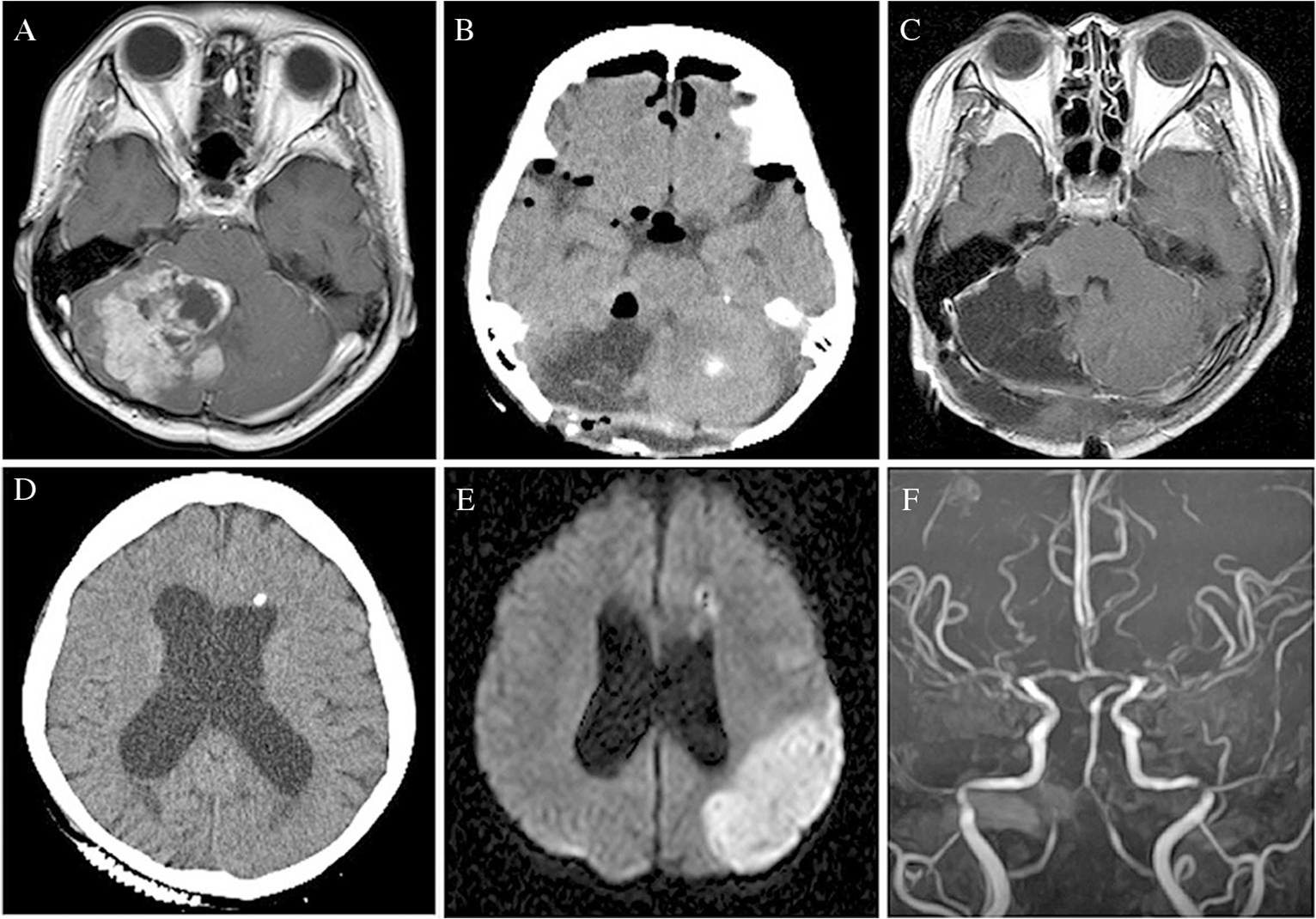
Preoperative T1-weighted MRI shows a large mass in the right cerebellar hemisphere with homogeneous enhancement with gadolinium contrast medium (A). Postoperative CT shows no subarachnoid hemorrhage in the basal cistern (B). Postoperative MRI shows no residual tumor (C). A shunt tube was inserted in the left lateral ventricle; no infarction was detected (D). Diffusion-weighted imaging shows a high-intensity area in the left parietal lobe (E). Magnetic resonance angiography shows bilateral narrowing of the anterior cerebral and middle cerebral arteries (F).
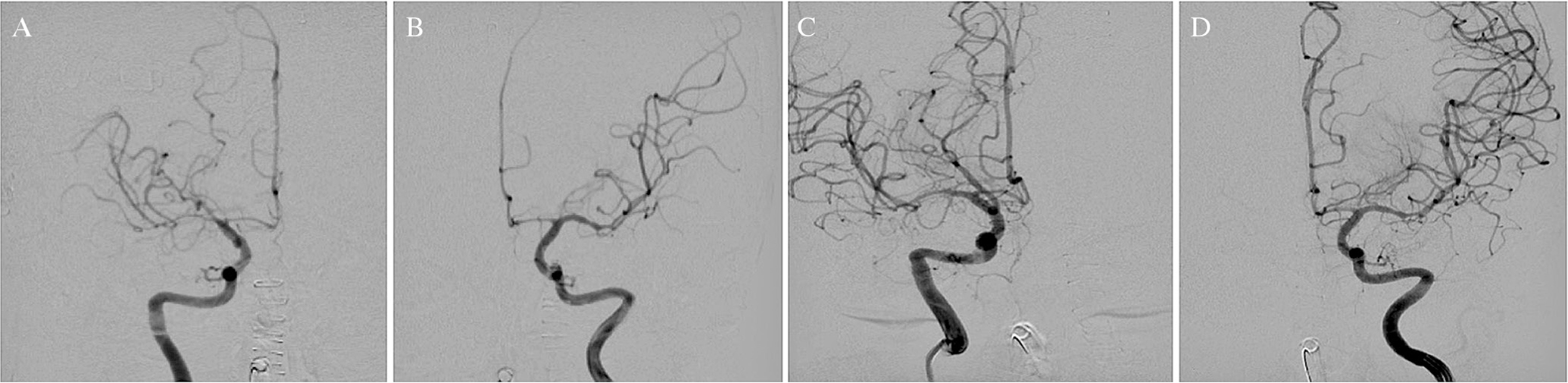
Carotid angiography (CAG) shows narrowing of the anterior cerebral artery (ACA) and middle cerebral artery (MCA) (A, right; B, left). CAG after fasudil hydrochloride injection shows good dilatation of bilateral ACA and MCA (C, right; D, left).
The patient was placed under local anesthesia, and a 5-French sheath was inserted in the right femoral artery. After systematic heparinization, a 5-French guiding catheter was positioned in the left internal carotid artery (ICA) and a microcatheter (Excelsior SL-10; Stryker, Kalamazoo, MI, USA) was navigated to the distal ICA. Thereafter, fasudil hydrochloride (15 mg) was injected for 10 min (1.5 mg/min). A similar procedure was performed on the right side, and the same amount of fasudil hydrochloride was injected. After natural reversal of heparin, CT revealed no new infarction after treatment. Cerebral vasospasm was improved by 3 days of fasudil hydrochloride injection (Figs. 2C and 2D). The patient’s symptoms gradually improved, and she was discharged with mild hemiparesis (modified Rankin Scale 2).
Despite improvements in antimicrobial therapy, bacterial meningitis still has clinically significant morbidity and mortality.2,3) The clinical outcomes of bacterial meningitis are often affected by intracranial consequences, such as cerebral edema, hydrocephalus, and cerebrovascular complications.2,4) Cerebrovascular complications are common, but severe cerebral vasospasm that causes ischemic injury is rarely reported.5) Conversely, postmortem histopathological evaluation of patients who died of acute bacterial meningitis suggests that the occurrence of cerebral vasospasm is more frequent than reported.6) The pathogenesis of cerebral vasospasm in bacterial meningitis has not been elucidated and it is likely that inflammatory cytokines, leukocytes in the cerebrospinal fluid, and spasm-induced free radicals are involved.7–9)
The onset, duration, and recommended treatment of cerebral vasospasm associated with SAH are well known. Conversely, vasospasm associated with meningitis is relatively rare and treatment strategies are not well known.2) Hypervolemia, hypertension, and hemodilution (triple H) therapy can prevent ischemic deficit after cerebral vasospasm associated with meningitis but it is not always effective.10) Triple H therapy may also be harmful to patients because of the risk of cerebral hemorrhage in central nervous system infections.6)
Balloon angioplasty is regarded as an effective treatment for local cerebral vasospasm; however, inflammation weakens the arterial wall and increases the risk of vessel rupture during balloon inflation.1) Conversely, intra-arterial vasodilation is safe and extensively effective and results in a mild-to-moderate improvement in vessel diameter and distal flow. The treatment stabilizes the clinical condition and does not cause vascular rupture.7)
Nimodipine, nicardipine, papaverine, verapamil, and fasudil hydrochloride have been reported as intra-arterial vasodilator for vasospasm.11–17) Nimodipine and nicardipine have been associated with decreased arterial blood pressure.6) Papaverine is associated with the risk of injury to the vascular endothelium and media and should be used with caution. Furthermore, the risk of severe adverse effects, such as respiratory depression, tachycardia, systemic hypotension, cerebral hypertension, and brainstem symptoms must also be considered for papaverine.15,16) Fasudil hydrochloride is a novel and potent vasodilator. It inhibits protein kinases, such as Rho kinase, myosin light chain kinase, protein kinase C, and myosin light chain phosphorylation.18) Fasudil is as or more effective than nimodipine for the prevention of cerebral vasospasm and subsequent ischemic injury in patients undergoing SAH surgery.18) Fasudil hydrochloride is relatively safe, has little effect on blood pressure, has a dose-dependent effect on the relaxation of convulsive vascular tone, few effects on vascular endothelium or media, and contributes to its relative safety.19)
Recently, five cases of endovascular treatment for vasospasm secondary to bacterial meningitis have been reported (Table 1). All patients were male with an average age of 42 (20–57) years. Only one case was associated with postoperative meningitis.20) Two cases were treated with intra-arterial verapamil,5,7) one with intra-arterial nicardipine,7) and one with intra-arterial nitroglycerin and balloon angioplasty.21) All patients showed good recovery; therefore, an intra-arterial vasodilator, especially fasudil hydrochloride, might be a better option for vasospasm secondary to bacterial meningitis.
| Author (year) | Age(y)/Sex | Strain | Cause | Timing (days) | Place of spasm | Treatment | Outcome |
|---|---|---|---|---|---|---|---|
| Chaichana (2007)20) | 49/M | Gram-positive cocci | Post-operation | 14 | ICA/ACA/MCA | Triple H | GR |
| Buechner (2012)21) | 20/M | Staphylococcus aureus | Sphenoid sinusitis | 11 | ICA and MCA | Nitroglycerin, PTA | GR |
| Taqui (2014) | 38/M | Streptococcus pneumoniae | Mastoiditis | 9 | VBA/PCA/ICA | Verapamil | GR |
| Taqui (2014)7) | 57/M | Streptococcus pneumoniae | Pneumoniae | 10 | ICA/MCA/ACA | Nicardipine | GR |
| Nussbaum (2015)5) | 46/M | Streptococcus viridans | Sinusitis | 14 | PCA | Verapamil, Bypass | GR |
| Present case | 37/F | Streptococcus oralis | Post-operation | 14 | ACA/MCA | Fasudil hydrochloride | GR |
ACA: anterior cerebral artery, GR: good recovery, ICA: internal carotid artery, MCA: middle cerebral artery, PCA: posterior cerebral artery, triple H: hypervolemia, hypertension, and hemodilution therapy, VBA: vertebrobasilar artery.
Symptomatic cerebral vasospasm secondary to bacterial meningitis is relatively rare and difficult to treat. Endovascular treatment could be considered in selected cases of symptomatic cerebral vasospasm after meningitis. Intra-arterial vasodilator injection may be safer compared with balloon angioplasty. Fasudil hydrochloride should be considered for use as a vasodilator.
We would like to thank Dr. Takashi Maruyama and Dr. Syunsuke Tsuzuki for the initial treatment of this case.
The authors have no financial conflicts of interests. All authors who are members of The Japan Neurological Society have registered online self-reported COI Disclosure Statement Forms through the JNS member website.