2019 Volume 6 Issue 3 Pages 71-74
2019 Volume 6 Issue 3 Pages 71-74
Spontaneous cervical internal carotid artery dissection (CICAD) is occasionally treated with conservative management, mainly using antithrombotics. However, we have to consider emergency interventions for bilateral CICAD occurring simultaneously and accompanied by progressive cerebral ischemia. A 46-year-old woman was brought to our hospital with a complaint of left-handed clumsiness, blurred vision in the left eye, and right hemiplegia. Acute cerebral infarction in bilateral cerebral hemispheres was evident on brain magnetic resonance imaging. Bilateral internal carotid arteries were barely visible on time-of-flight magnetic resonance angiography. Subsequent cerebral angiography demonstrated that cervical internal carotid arteries on both sides were tapered off immediately after the bifurcations, indicating CICAD. Despite management with intravenous antithrombotic agents and hydration, neurological status gradually deteriorated. After insertion of a transvenous temporary pacemaker, we performed simultaneous bilateral carotid artery stenting (sbCAS) 3 days after admission. The patient first suffered slight right-sided hemiplegia and hoarseness, but symptoms resolved after rehabilitation, and modified Rankin Scale was 0 as of 2 years after the procedure. Bilateral CICAD causes severe insufficiency of cerebral blood flow, and symptoms often persist even after administration of antithrombotic agents. In such refractory cases, early intervention should be considered, and sbCAS can be safely performed. During the procedure, a transvenous temporary pacemaker maintains hemodynamic stability and might be a favorable option.
Arterial dissections cause stroke in relatively young population and result in various neurological sequalae. According to the Cervical Artery Dissections and Ischemic Stroke Patients study, one of the largest observational studies evaluating extracranial artery dissection, bilateral internal carotid dissections are found in 10% of patients with spontaneous cervical internal carotid artery dissection (CICAD)1); however, CICAD that is bilaterally simultaneously diagnosed and treated has rarely been reported. We herein describe a case of simultaneous bilateral CICAD which was successfully treated with bilateral carotid artery stenting (CAS) and speculation about this clinically challenging condition.
A 46-year-old woman was brought to our hospital complaining of left-handed clumsiness and blurred vision in the left eye, both of which emerged 3 days before the visit, followed by the development of right hemiplegia. Her past medical history was unremarkable. While magnetic resonance imaging (MRI) was being performed, the patient became obtunded, and imaging showed cerebral infarction in bilateral white matter and faint bilateral carotid arteries (Figs. 1A–1C). Glasgow Coma Scale score on admission was E3V4M6, and the patient showed right mild hemiplegia and paraphasia. Since this patient was thought to have suffered non-cardiogenic moderate-sized cerebral ischemia, we initiated continuous infusion of argatroban. The following day, catheter angiography was performed to assess the bilateral internal carotid stenosis: the image showed tapered stenosis from bilateral carotid bifurcations, suggesting internal carotid dissection. In the left side, the ICA was depicted in a considerably delayed phase compared with the external carotid artery. Also, retrograde flow from the ophthalmic artery to the carotid siphon was confirmed, and the anterograde flow appeared in a delayed phase, which indicated insufficient intracranial perfusion. In the right side, the carotid siphon was also visualized via retrograde flow from the ophthalmic artery, but the anterograde carotid flow was barely visible. Right vertebral artery angiography showed strong collateral circulation anteriorly to bilateral carotid arteries via bilateral posterior communicating arteries. In addition, we performed contrast-enhanced computed tomography (CT) of the whole trunk in consideration of the possibility of fibromuscular dysplasia, but no features suggestive of that disease were apparent. Despite aggressive rehydration and administration of argatroban, neurological symptoms deteriorated and follow-up MRI revealed enlarging bilateral cerebral infarction (Fig. 1D). Two days after admission, we decided to perform bilateral CAS under dual antiplatelet therapy, and inserted a temporary pacemaker from the right femoral vein to prevent intraoperative bradycardia and hypotension prior to CAS. We chose local anesthesia with a small amount of propofol. After puncture of the left common femoral artery, a guiding catheter (9Fr Optimo 90 cm; Tokai Medical Products, Kasugai, Aichi, Japan) was navigated to the left common carotid artery. Left common carotid artery angiography (CCAG) showed that the stenotic region was limited to the cervical portion of the ICA (Figs. 2A and 2B), so we decided to deploy a Carotid Wallstent (Boston Scientific, Marlborough, MA, USA). We used proximal balloon protection, inflating Optimo balloon during the lesion-cross. Since the lesion was highly stenotic, we selected Carotid Guardwire (Carotid Guardwire; Boston Scientific, Marlborough, MA, USA) due to its low profile. Additionally, as thromboembolism migrating from the dissection cavity should have been prevented during angioplasty and stent placement, we chose distal balloon protection. After the lesion-cross by Guardwire, we confirmed that the tip of Guardwire was inside the true lumen. The Guardwire balloon was then inflated at the level of the external auditory meatus. After pre-stenting angioplasty with a balloon (Coyote ES 3.0 mm × 4.0 cm; Boston Scientific, Marlborough, MA, USA), a Wallstent (10 mm × 31 mm) was deployed (Fig. 2C). We did not perform post-stenting angioplasty. A whitish thrombus was captured by a suction catheter. Even after left-side CAS, right CCAG still showed significantly delayed blood flow to the right middle cerebral artery. Judging from this finding, we decided to perform right-side CAS. The right CCAG demonstrated that the proximal end of the stenosis was immediately distal to the carotid bifurcation (Fig. 2D). The distal end of the stenosis was the petrous portion of the ICA, and angiography depicted intracranial vessels in a significantly late phase (Fig. 2E). After the pre-stenting angioplasty at two consecutive sites, we attempted to deploy a Wallstent (10 × 31 mm2) from the petrous portion. However, we could not pass the stent through the stenotic area. Then we deployed Wallstent (6 mm × 22 mm) from the petrous portion and subsequently deployed Wallstent (10 mm × 31 mm), partly overlapping the first stent (Fig. 2F). No bradycardia or hypotension appeared during the procedure. Postoperative 123I-iodoamphetamine single photon emission computed tomography (IMP-SPECT) showed significantly increased cerebral blood flow (Fig. 3A); the patient was started on sedation with propofol to avoid hyperperfusion. On postoperative day (POD) 1, the temporary pacemaker was removed, and diffusion-weighted imaging (DWI) revealed expansion of bilateral watershed white matter infarctions, but magnetic resonance angiography showed excellent depiction of bilateral ICAs (Figs. 3B and 3C). On POD 3, normalized cerebral blood flow was recognized via IMP-SPECT, so sedation was stopped. The patient started oral intake from POD 17 and was transferred to a rehabilitation facility with slight right-sided hemiplegia and hoarseness on POD 32. Three months after transfer, she was discharged from the facility, and modified Rankin Scale was 0 as of 2 years after the procedure.
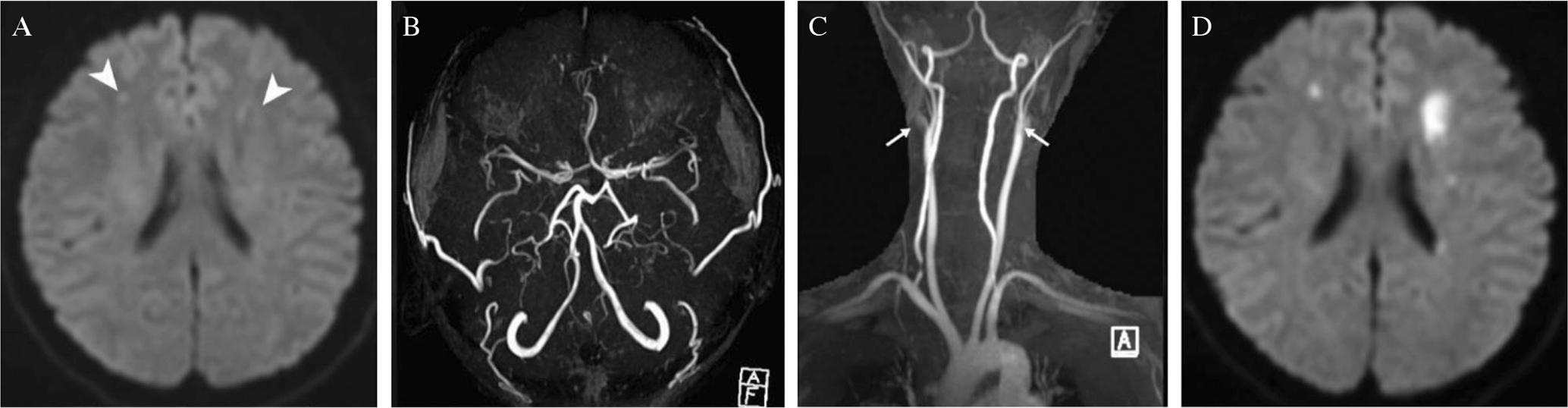
Magnetic resonance imaging performed on admission (A–C) and follow-up imaging (D): (A) diffusion-weighted imaging (DWI); (B) Magnetic resonance arteriography (MRA) of the head, and (C) MRA of the next: (A) High-intensity spots are seen in bilateral watershed areas of white matter (white arrowheads). (B) The internal carotid arteries proximal to the posterior communicating arteries are faint. Signals are less intense for the anterior circulation than for the posterior circulation. (C) Origins of bilateral internal carotid arteries are hazy (white arrows). (D) Follow-up DWI performed 2 days after admission shows enlarged white matter infarction.
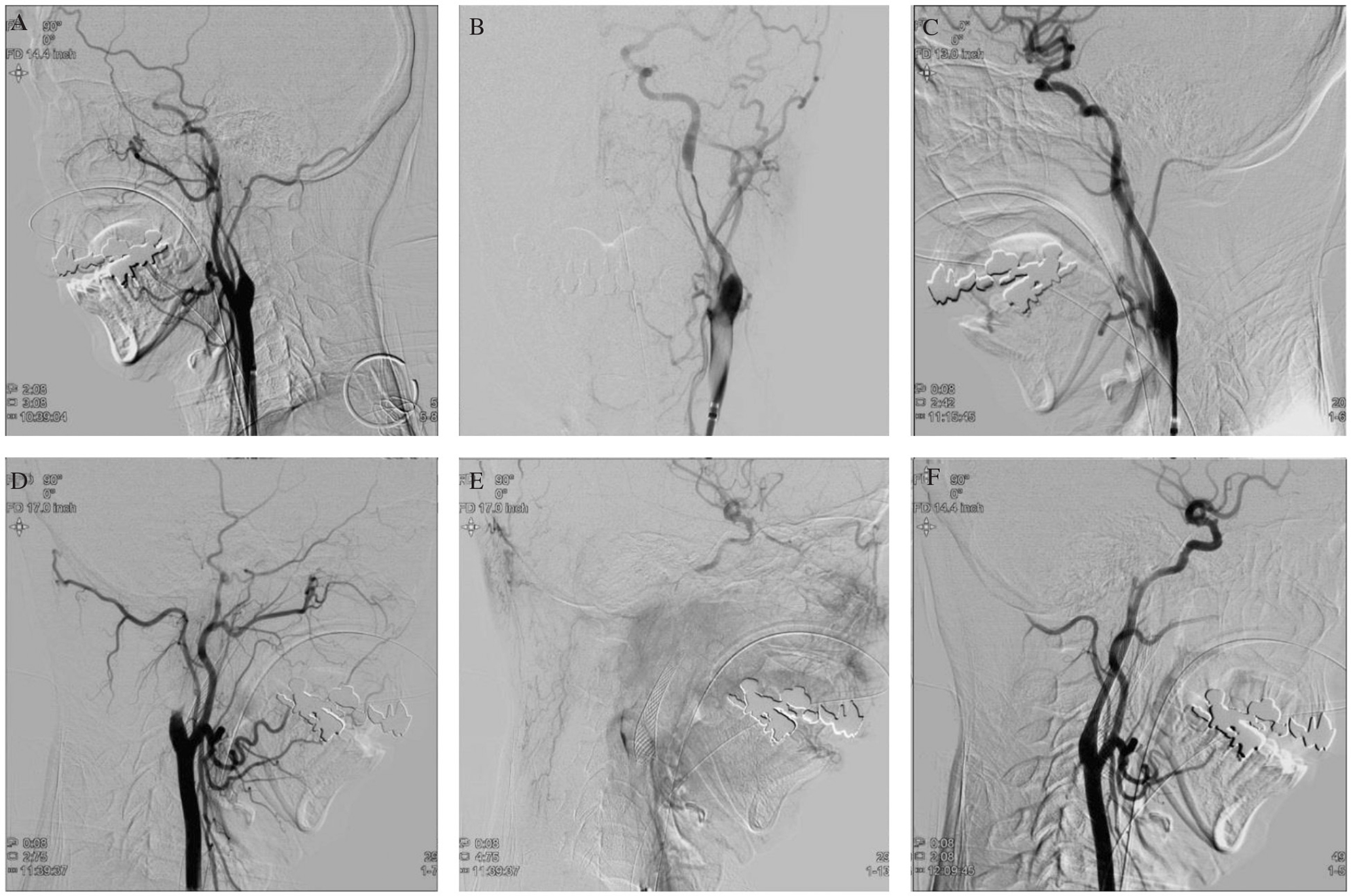
Cervical carotid angiographies: (A) Left-side preoperative angiography (lateral view). (B) Left-side preoperative angiography (anteroposterior view) shows proximal and distal ends of the dissection. (C) Left-side postoperative angiography (lateral view). (D) Right-side preoperative angiography (lateral view) demonstrates the proximal end of dissection. (E) Right-side preoperative angiography (lateral view) in the late phase demonstrates the distal end of the dissection and anterograde flow to the intracranial internal carotid artery. (F) Right-side postoperative angiography (lateral view).
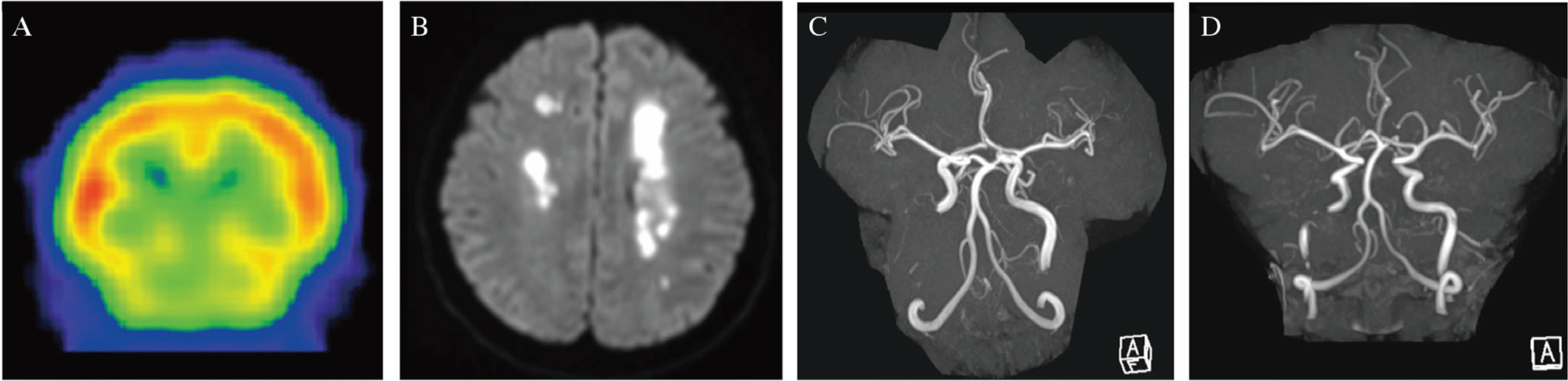
123I-iodoamphetamine single photon emission computed tomography (IMP-SPECT) performed on postoperative day 1 (A) and magnetic resonance imaging performed on postoperative day 1 (B and C) and 3 months after the procedure (D): (A) IMP-SPECT coronal imaging shows relatively hyperperfused cerebral hemispheres compared with the cerebellum. (B) Diffusion-weighted imaging shows enlargement of bilateral white matter infarctions. (C) Magnetic resonance arteriography (MRA) demonstrates strong signal intensities in the anterior circulation, indicating hyperperfusion. The right internal carotid artery is partly invisible due to metal artifacts from the carotid stents. (D) MRA performed three months after the procedure confirms intact intracranial perfusion.
Observational data suggest that CICAD can result from trauma (up to 40% of all cases), fibromuscular dysplasia (15–20%), Ehlers–Danlos syndrome type IV (<2%) and other connective tissue and vascular disorders.1,2) The present patient had no history of head or neck trauma, and no signs of systemic vascular disease were seen, including fibromuscular dysplasia on whole-trunk CT angiography. We were unable to identify a definitive etiology in this case.
Approximately 10% of patients with CICAD have bilateral lesions,1) but the safety and effectiveness of CAS for simultaneous bilateral CICAD have barely been discussed. CAS for CICAD is indicated under the following conditions: (1) symptoms persist or worsen under antiplatelet therapy; (2) significant hemodynamic insufficiency appears; or (3) contraindications exist for antithrombotic therapy.3) Endovascular stenting, compared with medical treatment, carries a substantial advantage in immediate vascular reconstruction.4) Since this patient met criteria 1 and 2 mentioned above, we decided to conduct emergency bilateral CAS. Although many reports have described simultaneous bilateral CICAD in the past, treating both lesions simultaneously is impossible in most cases due to various limitations or a lack of indications (e.g., complete occlusion or mild stenosis of the cervical carotid artery). Such cases are observed conservatively, treated on only one side, or undergo staged CAS. As far as we have been able to ascertain from online searches, only two cases of simultaneous bilateral CAS (sbCAS) for CICAD have been reported.5,6) Keilani et al. described a case involving the formation of pseudoaneurysm after trauma, which did not improve after administration of antithrombotic drugs. They therefore performed sbCAS 9 days after injury.5) On the other hand, Sedat et al.6) performed sbCAS for nontraumatic bilateral CICAD in which the stenosis gradually deteriorated. Unlike the above two cases, symptoms of cerebral ischemia associated with high-grade stenosis were marked in our case.
Bilateral CICAD with sudden onset probably involves hemodynamic compromise that is more severe than atherosclerotic lesions as the collateral circulation has not sufficiently developed. CICADs are considered to resolve spontaneously in a high proportion of cases,7) but, in cases with bilateral CICAD, active intervention is necessary if at least one of the abovementioned three conditions is present. According to a report by Jiang et al.,8) hemodynamic depression triggered by carotid sinus reflex, and hyperperfusion syndrome require attention after simultaneous bilateral CAS, although that report was about atherosclerotic internal carotid stenosis. Unlike the condition of atherosclerotic change, bilateral carotid dissection involves sudden hemodynamic compromise, and the risk of hyperperfusion is probably lower. Simultaneous bilateral CAS is thus probably a reasonable alternative to staged procedures.
Hemodynamic depression is another risk of simultaneous bilateral CAS due to bilateral activation of the carotid sinus reflex. Jiang et al. reported the simultaneous bilateral CAS group showed hemodynamic depression more frequently than the unilateral CAS group. Bradycardia or hypotension occurred in more than 30% of patients, and vasopressor support was required in 19.2% after simultaneous bilateral CAS according to the literature.8) Another report verified the effectiveness of prophylactic, albeit transcutaneous, temporary pacemakers.9) According to that report, postprocedural sinus bradycardia was rarely observed in any patient. They concluded that temporary pacemakers can be removed after the procedure. To preclude intra- and postoperative hemodynamic depression, transvenous insertion of a temporary pacemaker might represent a favorable option, as shown in our case, if skilled cardiologists are immediately accessible.
Technical tips to keep in mind during CAS for CICAD are the use of embolic protection systems, securing the true lumen and type of stent for deployment. Meticulous handling is prerequisite during navigation of the microguidewire through the stenotic area, and the utility of proximal protection for preventing thromboembolism has been reported.10) Dissection has also been reported to occasionally start 20–30 mm distal to the carotid bifurcation.11,12) We need to keep this distance in mind when manipulating the microguidewire.
We encountered a case involving bilateral CICAD and successfully performed simultaneous bilateral CAS. Bilateral CICAD causes severe insufficiency of cerebral blood flow, and symptoms often persist even after hydration and administration of antithrombotic agents. In such refractory cases, early intervention should be considered. During simultaneous bilateral CAS, a transvenous temporary pacemaker maintains hemodynamic stability and might represent a favorable option.
The authors report no conflicts of interest (COI) concerning the materials or methods used in this study or the findings specified in this paper. All authors who are members of The Japan Neurosurgical Society (JNS) have registered online Self-reported COI Disclosure Statement Forms through the website for JNS members.