Abstract
Cavernous internal carotid artery (ICA) aneurysm complicated by simultaneous and spontaneous formation of thromboses in the aneurysm and the parent artery is a rare clinical condition. Although the majority of patients have good outcomes, some patients experience severe ischemic stroke. Here, we report a case of symptomatic large cavernous ICA aneurysm complicated by rapid growth of an intra-aneurysmal thrombosis with simultaneous parent artery thrombosis. A 68-year-old female presented with sudden-onset diplopia, right ptosis, right conjunctival hyperemia, and paresthesia of the right face. Magnetic resonance imaging (MRI) and digital subtract angiography (DSA) revealed the presence of a large partially thrombosed aneurysm in the cavernous portion of the right ICA. We planned endovascular embolization using a flow-diverting (FD) stent. Dual-antiplatelet therapy (DAPT) with aspirin and clopidogrel was started 2 weeks prior to treatment. Although the neurological state was stable, DSA conducted on the day of the endovascular treatment showed rapid growth of an intra-aneurysmal thrombosis and de novo thrombosis in the parent artery. Direct aspiration was performed via a distal support catheter with proximal blood flow arrest using a balloon-guide catheter, and the FD stent was successfully deployed. The patient’s symptoms improved postoperatively and DSA obtained 12 months after the procedure confirmed complete occlusion of the aneurysm. Although the exact mechanism of simultaneous thrombosis formation of the aneurysm and its parent artery remains unclear, it is important to recognize that rapid growth of the thrombosis increases the risk of ischemic stroke.
Introduction
With recent technological advancements in neuroimaging, cavernous internal carotid artery (ICA) aneurysms are frequently diagnosed incidentally.1) Most cavernous ICA aneurysms have benign natural histories, with low cumulative rates of rupture.2) However, large (>15 mm) or giant (>25 mm) cavernous aneurysms may cause ophthalmoplegia, chemosis, ptosis, proptosis, visual changes, facial pain or numbness, and Horner’s syndrome (collectively called “cavernous sinus syndrome”) because of their mass effect.3,4) Moreover, recent literature reported that aneurysm size was a significant predictor of aneurysmal growth, and even asymptomatic large or giant aneurysms potentially present risks of new-onset symptoms.1) Partial or complete thrombosis is not uncommon in such large/giant aneurysms,5) and thromboembolic events caused by intra-aneurysmal thromboses have been also reported.1) Although spontaneous intra-aneurysmal thrombosis involved parent artery thrombosis is rare and usually has good outcomes, some patients experience severe ischemic stroke.5)
Here, we present a rare case of symptomatic large cavernous ICA aneurysm complicated by rapid growth of an intra-aneurysmal thrombosis and simultaneous thrombosis formation in the parent artery.
Case Description
Preoperative course, neurological and radiological examinations
A 68-year-old female with a history of hypertension and dyslipidemia presented to our department with sudden-onset diplopia, right ptosis, right conjunctival hyperemia, and paresthesia of the right face. Neurological examination revealed right oculomotor nerve palsy and hypesthesia in the areas supplied by the ophthalmic (V1) and maxillary (V2) branches of the right trigeminal nerve. Magnetic resonance imaging (MRI) and MR angiogram revealed a well-defined mass adjacent to the cavernous portion of the right ICA (Fig. 1A). The mass was iso-intense on T1-weighted images and hypo-intense on T2-weighted images (T2WI) (Fig. 1B and 1C). The posterior part of the mass was partially hyper-intense on T2WI, and the lesion appeared to be a partially thrombosed cavernous ICA aneurysm. Digital subtraction angiography (DSA) demonstrated a large aneurysm (22 mm) in the cavernous portion of the right ICA (Fig. 2A and 2B). In compression study, collateral circulation from the contralateral ICA through the anterior communicating artery was not confirmed; however, collateral blood supply from the posterior circulation through the right posterior communicating artery was confirmed (Fig. 2C and 2D). The patient was diagnosed with a symptomatic large cavernous aneurysm and endovascular embolization using FD stent was scheduled.

Fig. 1
Preoperative time of flight MR angiography (A), axial T1-weighted MR image (B), and axial T2-weighted MR image (C) showing a well-defined mass in close relation to the cavernous portion of the right ICA. ICA: internal carotid artery, MR: magnetic resonance.

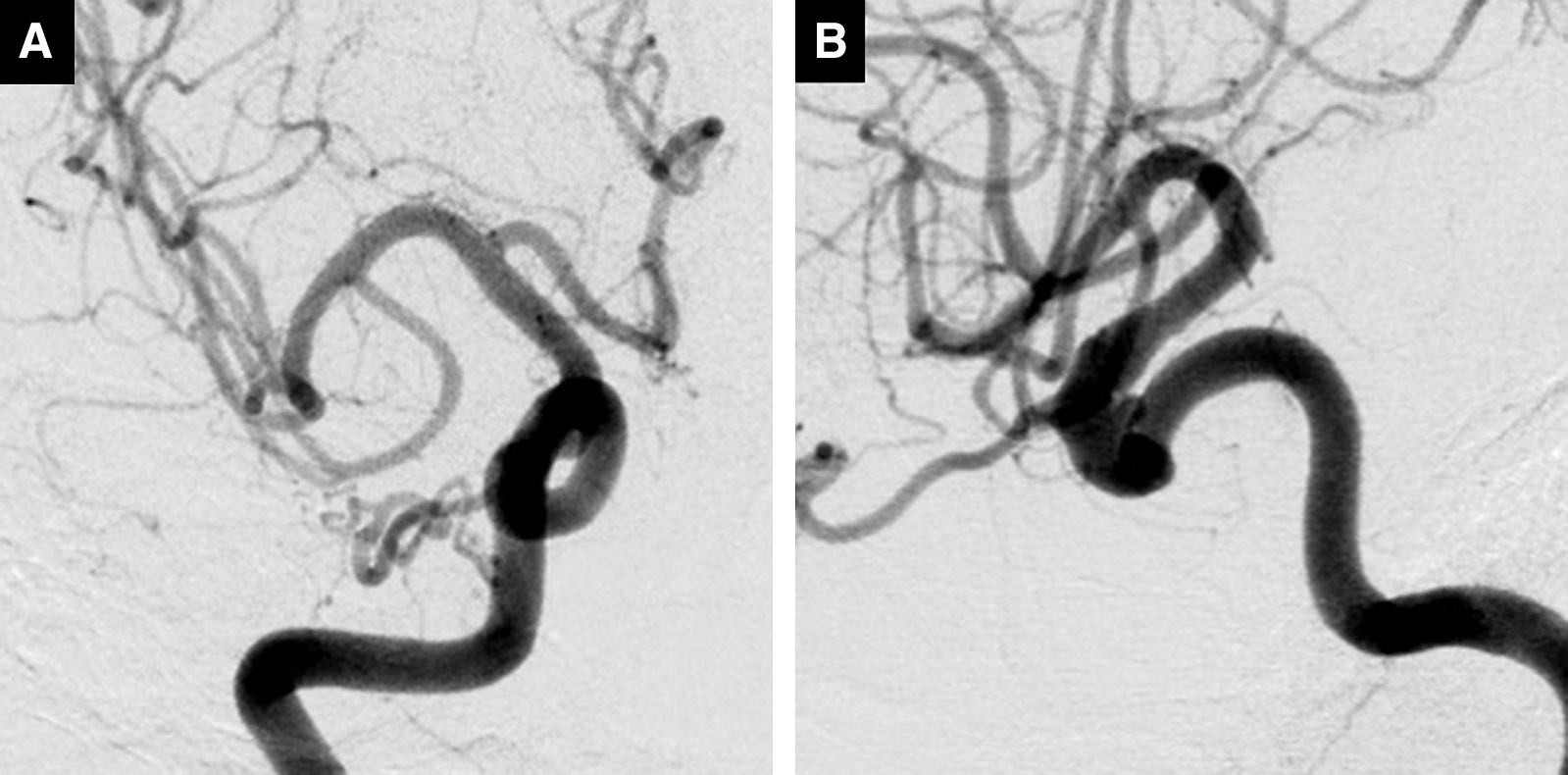
Fig. 2
(A and B) Antero-posterior view and lateral view of the right ICA angiography obtained 3 weeks before the endovascular procedures, demonstrating a large aneurysm (22 mm) in the cavernous portion of the right ICA. (C and D) Antero-posterior view of the left ICA angiography and lateral view of the right vertebral artery angiography with compression of the right carotid artery (compression study), demonstrating collateral blood supply from the posterior circulation to the right ICA through the right posterior communicating artery. ICA: internal carotid artery.
The patient was pretreated with dual-antiplatelet therapy (DAPT) consisting of aspirin 100 mg daily and clopidogrel 75 mg daily 2 weeks before the treatment. Assessment of P2Y12 reaction units (PRU), showing platelet inhibition reactivity of clopidogrel or other P2Y12 antagonists, was conducted using VerifyNow P2Y12 assay (Accumetrics, San Diego, CA, USA) 2 days before the treatment. The PRU, baseline value (BASE), and % inhibition (%INH), which was calculated as ([BASE-PRU]/BASE) were 197, 187, and 0%, respectively. The details of the VerifyNow P2Y12 assay are described elsewhere.6) Because the patient was suspected to be a poor responder for clopidogrel (%INH <40%),7,8) we changed the anti-platelet agent from clopidogrel to prasugrel, 3.75 mg daily (loading dose 20 mg). The PRU, BASE, and %INH on the day of the treatment were 96, 193, and 50%, respectively. The neurological status had been stable up to the day of the endovascular treatment.
Procedures
The endovascular procedure was conducted in an angiography suite under general anesthesia 3 weeks after admission. Systematic heparinization was achieved with a target activated clotting time of 250–300 seconds. We planned to deliver a 4.25 mm × 20 mm Pipeline Embolization Device (PED; Covidien/eV3 Neurovascular, Irvine, CA, USA) with transfemoral approach using a triple coaxial system consisting of an 8-F Launcher guiding catheter (Medtronic Neurovascular, Irvine, CA, USA), a 5-F 0.058-inch diameter Navien distal support catheter (Covidien/eV3 Neurovascular), and a Marksman microcatheter (Covidien/eV3 Neurovascular). Right ICA angiography conducted in advance of delivery of the PED demonstrated a filling defect of contrast material in most of the aneurysm and the siphon of the right ICA (Fig. 3A). As simultaneous thromboses in the aneurysm and its parent artery were suspected, direct aspiration of the thrombus in the parent artery was performed. To avoid distal migration of the thrombus, the 8-F Launcher guiding catheter (Medtronic Neurovascular) was exchanged for a 9-F Optimo balloon-guide catheter (Tokai Medical Products, Aichi, Japan). Direct aspiration of the thrombus via a 5-F Navien distal support catheter (Covidien/eV3 Neurovascular) was performed with proximal blood flow arrest using a balloon-guide catheter (Fig. 3B). The thrombus was a red thrombus and there were no apparent findings for organization. Most of the thrombus was removed by this procedure (Fig. 3C). The PED (Covidien/eV3 Neurovascular) was successfully deployed via a Marksman microcatheter (Covidien/eV3 Neurovascular) to cover the neck of the aneurysm in a state in which proximal blood flow arrest was continued (Fig. 3D–3F).

Fig. 3
(A) DSA obtained on the day of endovascular treatment showing a rapid growth of the intra-aneurysmal thrombosis (arrow heads) and the de novo thrombosis in the parent artery (arrow). (B) Direct aspiration of the thrombus in the parent artery via a distal support catheter (arrow) with proximal blood flow arrest using a balloon-guide catheter (double arrow). (C) Most of the thrombus in the parent artery was removed (arrow). (D) High-resolution computed tomography image showing sufficient apposition of the FD stent to the right ICA. (E and F) Antero-posterior view and lateral view of the postoperative DSA showing good antegrade blood flow to the distal territory. DSA: digital subtract angiography, FD: flow-diverting, ICA: internal carotid artery.
The patient developed no neurological deterioration after the procedure. Postoperative diffusion-weighted images (DWI) obtained the day following the procedure detected no ischemic lesion. Right oculomotor nerve and trigeminal nerve palsy gradually improved. DSA obtained at 12 months after the procedure demonstrated complete occlusion of the aneurysm (Fig. 4A and 4B).
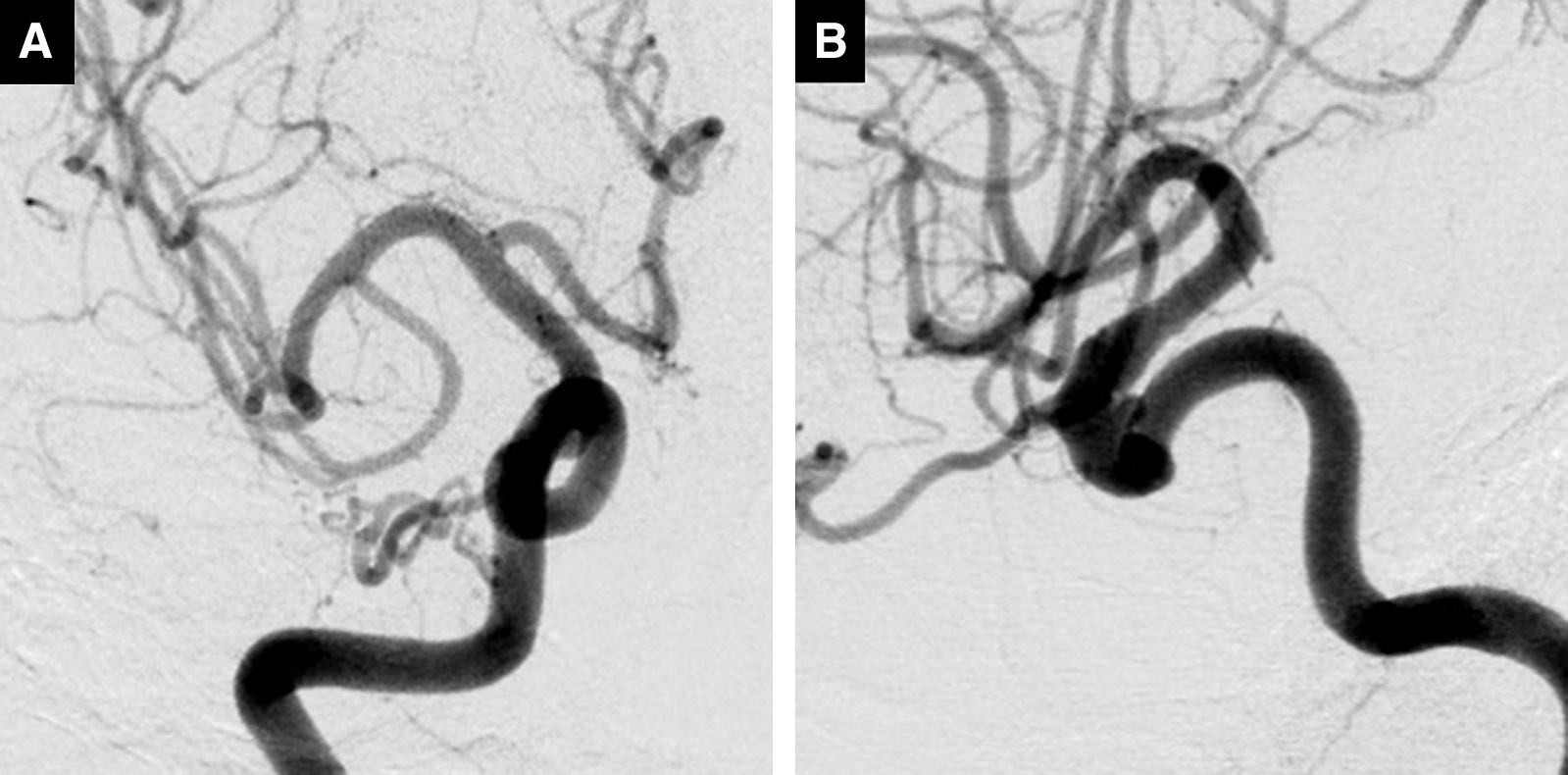
Fig. 4
(A and B) Antero-posterior view and lateral view of the DSA obtained 12 months after the treatment showing complete occlusion of the aneurysm. DSA: digital subtract angiography
Discussion
Thrombosis formation inside large or giant intracranial aneurysms is not uncommon. Most intra-aneurysmal thrombosis is partial, and the incidence of complete thrombosis is significantly lower (50–60% vs. 13–20%).5,9) Hemodynamic stress on the aneurysmal wall with subsequent endothelial damage has been described as the main cause of this phenomenon.5,10) The key predisposing factors are known to be an increased dome-neck ratio, long-standing aneurysm, and blood hypercoagulability.5) Simultaneous thromboses in the aneurysm and its parent artery is a rare clinical condition, and the exact mechanism behind this complication remains unclear.5,10,11) Whittle et al.12) described two possible mechanisms: first, the direct distortion and compression of the parent artery by the aneurysm, and second, the retrograde development of the thrombus originating from the aneurysm. Localized stretching, compression, and distortion of the ICA could explain the occurrence of this pathological condition in cavernous ICA aneurysms, which may be due to the presence of dural folds and bony structures at this location.10) The possibility of distal embolic occlusion secondary to migration of intra-aneurysmal thrombus (aneurysm-to-distal arteries emboli) has also been previously described.9) According to the literature, about 5–8% of thrombus-containing giant intracranial aneurysms were associated with distal thrombo-embolism.13,14) In this case, the acute thrombosis in the parent artery may have been caused by compression of the artery by a growing partially thrombosed aneurysm or an aneurysm-to-distal arteries emboli, causing a reduction in blood flow in the parent vessel, which led to the rapid growth of the intra-aneurysmal thrombosis. We did not conduct pathological examination of the thrombus in the present case and this is a limitation of this report. Although the thrombus was a red thrombus and there were no macroscopic findings for organization, pathological findings might have helped to identify the etiology of the thrombus.
Management of thrombosed intracranial aneurysms involved with thrombosis of the parent artery is a matter of controversy. The majority of the reported patients are successfully managed conservatively, whereas some of these patients experience ischemic stroke.5) Whether adequate cerebral vascular reserve or sufficient collateral circulation is present or not is thought to be important in considering the indication of surgical intervention.5) According to a previous report, acute parent vessel thromboses are high risk for occurrence of ischemic stroke.5) As the rapid growth of the thrombosis in the aneurysm and its parent artery was considered a high risk for ischemic stroke, we conducted mechanical thrombectomy prior to the deployment of an FD stent. Owing to the necessity of reducing the risk of thrombus migration, we conducted direct aspiration via a 5-F Navien distal support catheter (Covidien/eV3 Neurovascular) with proximal blood flow arrest using a balloon-guide catheter. This enabled us to conduct deployment of the FD stent subsequent to aspiration of the thrombus without exchanging the distal access catheter. The Navien catheter (Covidien/eV3 Neurovascular) is a distal intracranial catheter designed to accommodate the 0.027-inch microcatheters required for deployment of flow-diverting (FD) stents.15) The large inner lumen is one of the characteristics of this catheter.15) The 5-F Navien catheter (Covidien/eV3 Neurovascular) has a 0.058-inch inner diameter (ID) and this is comparable to those of Penumbra 5 MAX (Penumbra, Alameda, CA, USA) or Penumbra 5 MAX ACE (Penumbra, Alameda, CA, USA) which have 0.054-inch and 0.060-inch IDs, respectively.16) Although further testing and evaluation are needed, the large ID of the Navien catheter (Covidien/eV3 Neurovascular) is thought to present advantages in terms of direct aspiration of thrombus.
In conclusion, we present a case of a symptomatic large cavernous ICA aneurysm, complicated by rapid growth of the intra-aneurysmal thrombosis and simultaneous parent artery thrombosis, which was successfully treated via direct aspiration using a 5-F Navien distal support catheter with no neurological complications for the patient. While the exact mechanism behind the simultaneous formation of spontaneous thrombosis of the aneurysm and its parent artery remains unclear, it is important to recognize that rapid growth of the thrombosis increases the risk of ischemic stroke.
Acknowledgment
We would like to thank Editage (www.editage.com) for English language editing.
Conflicts of Interest Disclosure
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper. All authors have registered online self-reported COI disclosure statement forms through the website for Japan Neurosurgical Society (JNS) members.
References
- 1) Vercelli G, Sorenson TJ, Aljobeh AZ, Vine R, Lanzino G: Cavernous sinus aneurysms: risk of growth over time and risk factors. J Neurosurg 132: 22–26, 2019
- 2) Wiebers DO, Whisnant JP, Huston J, et al.: Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet 362: 103–110, 2003
- 3) Tang Y, Booth T, Steward M, Solbach T, Wilhelm T: The imaging of conditions affecting the cavernous sinus. Clin Radiol 65: 937–945, 2010
- 4) Dacus MR, Nickele C, Welch BG, et al.: Matricidal cavernous aneurysms: a multicenter case series. J Neurointerv Surg 11: 584–590, 2019
- 5) Das KK, Singh G, Pandey S, Bhaisora KS, Jaiswal A, Behari S: Completely thrombosed giant intracranial aneurysm with spontaneous thrombosis of the parent artery: is it nature's divine intervention and a self-cure? World Neurosurg 118: 132–138, 2018
- 6) Luo Y, Li J, Liu X, et al.: Combination of P2Y12 reaction unit and percentage of platelet inhibition assessed by VerifyNow P2Y12 assay is a useful predictor of long-term clinical outcomes in patients with acute coronary syndrome undergoing percutaneous coronary intervention. Thromb Res 139: 114–120, 2016
- 7) Ari H, Ozkan H, Karacinar A, Ari S, Koca V, Bozat T: The EFFect of hIgh-dose ClopIdogrel treatmENT in patients with clopidogrel resistance (the EFFICIENT trial). Int J Cardiol 157: 374–380, 2012
- 8) Valgimigli M, Campo G, de Cesare N, et al.: Intensifying platelet inhibition with tirofiban in poor responders to aspirin, clopidogrel, or both agents undergoing elective coronary intervention: results from the double-blind, prospective, randomized Tailoring Treatment with Tirofiban in Patients Showing Resistance to Aspirin and/or Resistance to Clopidogrel study. Circulation 119: 3215–3222, 2009
- 9) Cohen JE, Itshayek E, Yitshayek E, et al.: Spontaneous thrombosis of cerebral aneurysms presenting with ischemic stroke. J Neurol Sci 254: 95–98, 2007
- 10) Chihi M, Jabbarli R, Gembruch O, et al.: A rare case of a completely thrombosed bilobed giant intracranial aneurysm of the anterior cerebral artery with spontaneous parent vessel thrombosis: case report. BMC Neurol 19: 297, 2019
- 11) Perrini P, Bortolotti C, Wang H, Fraser K, Lanzino G: Thrombosed giant intracavernous aneurysm with subsequent spontaneous ipsilateral carotid artery occlusion. Acta Neurochir (Wien) 147: 215–216; discussion 216-217, 2005
- 12) Whittle IR, Williams DB, Halmagyi GM, Besser M: Spontaneous thrombosis of a giant intracranial aneurysm and ipsilateral internal carotid artery. Case report. J Neurosurg 56: 287–289, 1982
- 13) Whittle IR, Dorsch NW, Besser M: Spontaneous thrombosis in giant intracranial aneurysms. J Neurol Neurosurg Psychiatry 45: 1040–1047, 1982
- 14) Lonjon M, Pennes F, Sedat J, Bataille B: Epidemiology, genetic, natural history and clinical presentation of giant cerebral aneurysms. Neurochirurgie 61: 361–365, 2015
- 15) Lin LM, Colby GP, Huang J, Tamargo RJ, Coon AL: Ultra-distal large-bore intracranial access using the hyperflexible Navien distal intracranial catheter for the treatment of cerebrovascular pathologies: a technical note. J Neurointervent Surg 6: 301–307, 2014
- 16) Takahira K, Kataoka T, Ogino T, Endo H, Nakamura H: Efficacy of a coaxial system with a compliant balloon catheter for navigation of the Penumbra reperfusion catheter in tortuous arteries: technique and case experience. J Neurosurg 126: 1334–1338, 2017