2021 Volume 8 Issue 1 Pages 89-93
2021 Volume 8 Issue 1 Pages 89-93
We describe a rare case of an anterolaterally projecting clinoid segment aneurysm of the internal carotid artery (ICA) causing oculomotor palsy. A 76-year-old woman was referred to our facility because of right oculomotor palsy that had been found just before surgery to remove bilateral cataracts. Neuroimaging revealed that the patient had an aneurysm at the clinoid segment that projected anterolaterally, eroding the anterior clinoid process. The aneurysm was thought to be compressing the oculomotor nerve, which runs at the upper part of the lateral wall of the cavernous sinus, thereby causing oculomotor palsy. Endovascular coiling of the aneurysm was successfully performed, and the oculomotor palsy was alleviated postoperatively. Anatomically, there exists the carotid collar between the arterial wall of the clinoid segment and the anterior clinoid process, containing the clinoid venous plexus in it. Hence, the anterolateral wall of the clinoid segment, although protected by a stiff bony structure, has an anatomical base that allows it to protrude centrifugally. Once protrusion occurs, the bone may be eroded by remodeling caused by the aneurysm’s pulsed beating.
It is widely known that oculomotor palsy can be caused by compression of an aneurysm at the junction of the internal carotid artery (ICA) and the posterior communicating artery, the junction of the basilar and superior cerebellar artery, or the cavernous segment of the ICA.1,2) The authors experienced a rare case of an anterolaterally projecting aneurysm at the clinoid segment of the ICA causing oculomotor palsy. As the lateral wall of the clinoid segment is protected by the bony architecture of the anterior clinoid process, it is of interest that an aneurysm could form there. The authors report this case with a review of the anatomy surrounding the clinoid segment of the ICA, discussing how this area generated an aneurysm.
A 76-year-old woman with a history of hypertension, dyslipidemia, and atrial fibrillation was hospitalized in our institution’s ophthalmology department to undergo surgery for bilateral cataracts. Physical examination at admission showed that she also had ptosis and slight external dislocation of the right eye. Pupils were 3 mm in size bilaterally, and the light reflexes were obscure probably because of cataract. She did not have diabetes mellitus. Magnetic resonance imaging revealed a right paraclinoid aneurysm, so she was referred to our department.
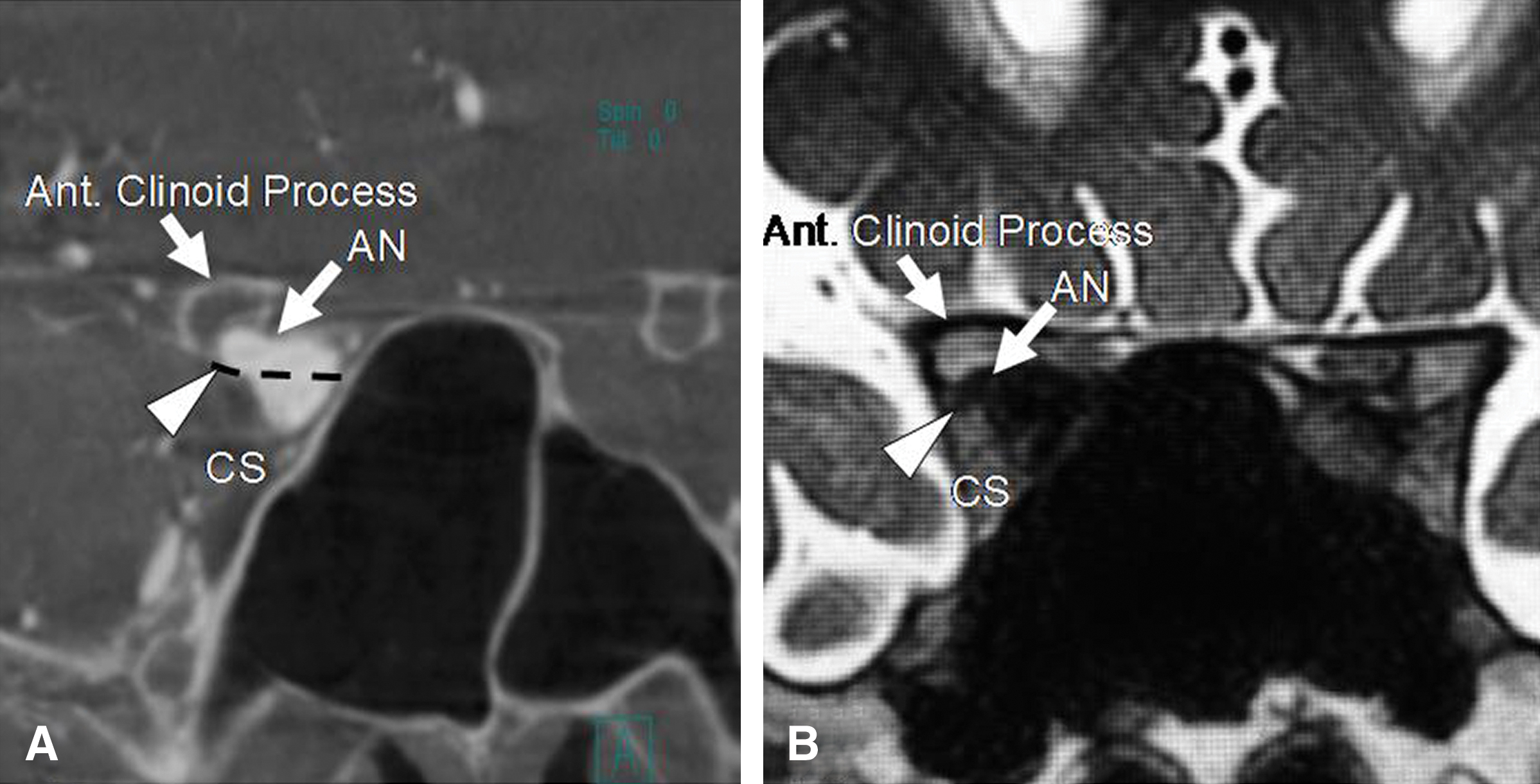
As she was not aware of having diplopia because of the severity of the cataracts, it could not be determined when the oculomotor palsy first occurred. Because an impending rupture could not be ruled out, the cataract operation was postponed and digital subtraction angiography was performed immediately. It showed that the aneurysm was located proximal to the origin of the ophthalmic artery, which seemed to have a lower-than-usual branching point. It appeared that the aneurysm had not been generated at the arterial branching point. The aneurysm projected anterolaterally and measured 5.6 mm at its neck, was 3.8 mm in height, and was 6.0 mm at its greatest dimension (Fig. 1). The dome of the aneurysm was embedded in the anterior clinoid process (Fig. 2). For more precise analysis, we then applied cone-beam computed tomography. The aneurysm was estimated to exist above the proximal dural ring, touching the oculomotor nerve that runs along the upper portion of the lateral wall of the cavernous sinus, thereby causing the oculomotor palsy. The anterior clinoid process, which did not contain extension of the paranasal sinus but was filled with bone marrow, was eroded by the aneurysm (Fig. 3A). With a coronal scan of heavily T2-weighted image, the topographical relationship between the aneurysm and the oculomotor nerve could be easily imagined (Fig. 3B).


Early intervention seemed necessary for this symptomatic aneurysm. As the aneurysm was wide-necked, stent-assisted coil embolization was performed using one Neuroform atlas stent (Stryker, Kalamazoo, MI, USA), one Axium platinum coil (Medtronic, Minneapolis, MN, USA), and three Target platinum coils (Stryker, Kalamazoo, MI, USA). The procedure was completed with a volume embolization ratio of 24.6%, leaving a tiny remnant of the aneurysmal neck.
Ptosis and slight exotropia of the right eye had improved by the day after the operation. The cataract surgery of both sides was carried out 6 months later. When the patient regained clear sight, she did not experience double vision. The status of the coil embolization was stable on MRI 6 months after the procedure.
The clinoid segment of the ICA is the portion exposed by removing the anterior clinoid process, defined as the segment between the proximal and distal dural rings.3–5) However, as the proximal ring (carotico-oculomotor membrane6)) becomes obscure at the medial side of the artery, and as the distal ring may decline at the posteromedial side of the artery to form the carotid cave,5) it is not always easy to find the exact margin of the segment, especially on the medial side of the artery.4) Clinically, for convenience, the clinoid segment may be considered the area between the lines projected medially from the upper and lower margins of the anterior clinoid process. Hence, aneurysms in the carotid cave, originally located above the distal ring, are sometimes treated as one of the clinoid segments.7,8) In addition to the type that protrudes medially, as in the present case, another type of aneurysm can arise in the clinoid segment, projecting anterolaterally, eroding the anterior clinoid process.4,7,9) This rare type is called a “subclinoid carotid aneurysm.”10) The ophthalmic artery originating from the clinoid segment is often found with this type.4) Although the ophthalmic artery of the present case seemed to have a lower origin than usual, it was difficult to determine that it arose at the clinoid segment for the abovementioned reasons. It was proved, at least, that the aneurysm was not located at the branching point of the artery.
The clinoid segment of the ICA is surrounded by a membranous architecture called the “carotid collar,” especially at its anterolateral aspect. There is also a clinoid venous plexus—which is an extension of the cavernous sinus—between the carotid collar and the wall of the clinoid segment of the ICA.3,5) (Fig. 4) Thus, the arterial wall of the clinoid segment adjoining the anterior clinoid process is not firmly fixed to the osseous clinoid process but is cushioned by a venous plexus. Hence, the anterolateral wall of the clinoid segment, although protected by a stiff bony structure, has an anatomical base that allows itself to protrude centrifugally. Once protrusion occurs, the bone may be eroded by remodeling caused by the pulsed beating of the aneurysm.11) This mechanism may also be applicable to the generation of the aneurysms in the carotid canal (surrounded by the internal carotid venous plexus) or the ones of the cavernous sinus protruding into the sphenoid sinus (interposed by the medial part of the cavernous sinus).

As the oculomotor nerve runs along the inferolateral margin of the anterior clinoid process, it is well known that care should be taken to avoid damaging this nerve when performing anterior clinoidectomy.12) Thus, it is not difficult to imagine that an aneurysm projecting in this direction along the carotico-oculomotor membrane may cause oculomotor palsy, as shown in the present case. Such cases are apparently rare, however, because we found no similar cases in the literature. Because our patient had become symptomatic, treatment was indicated. An aneurysm at this site is basically extradural. With enlargement, however, it can ascend through the anterior clinoid process to enter the subarachnoid space.4,10) Long-term follow-up is recommended even if the aneurysm is asymptomatic at the time of discovery.
All authors have no conflict of interest. They have registered online Self-reported COI Disclosure Statement Forms through the website for JNS members.