2021 Volume 8 Issue 1 Pages 33-37
2021 Volume 8 Issue 1 Pages 33-37
The authors report a rare autopsy case. A 59-year-old woman underwent flow diverter (FD) therapy using a pipeline embolization device (PED) for a large paraclinoid internal carotid artery aneurysm. Follow-up magnetic resonance (MR) examinations were performed 6 months after the treatment. Although the T2-weighted images showed progressive thrombosis of the aneurysm, the silent MR angiography (MRA) clearly showed the residual blood flow within the aneurysm. The patient committed suicide 2 months after the follow-up MR examinations. An autopsy specimen showed a small section of the defective membranes with the PED that matched the entry point of residual blood flow seen clearly in the silent MRA. Macroscopic photograph and hematoxylin and eosin stained sections showed defective endothelialization. In contrast, complete endothelialization was observed in membranes covering the PED. The autopsy findings after FD therapy showed defective endothelialization that perfectly matched and corroborated the silent MRA findings.
Flow diverter (FD) therapy for intracranial aneurysms has been an important alternative for open surgery. The pipeline embolization device (PED; Covidien, Irvine, CA, USA) is the most popular among FD devices worldwide. Herein, we report a rare autopsy case that showed defective endothelialization with a PED.
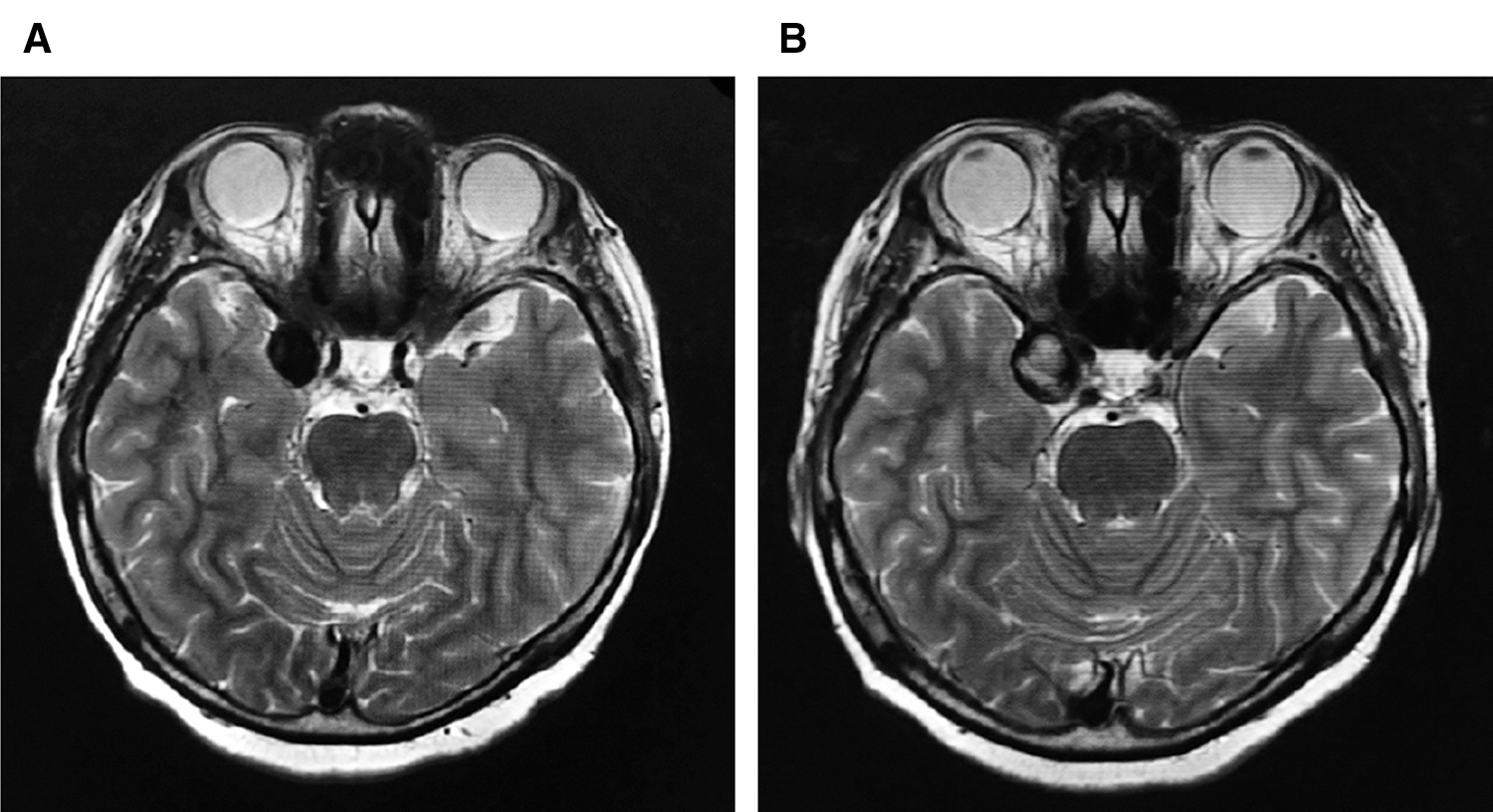
A 59-year-old woman was referred to our department with a 6-month history of right oculomotor nerve palsy. Pre-treatment T2-weighted magnetic resonance (MR) image (T2WI) showed a round flow void sign in the right paraclinoid region (Fig. 1A). Digital subtraction angiography (DSA) of the right internal carotid artery showed a large paraclinoid aneurysm (Fig. 2: longest diameter 24.2, shortest diameter 20.9, and neck width 7.5 mm). The patient underwent FD therapy using a PED (Fig. 3A). DSA images obtained immediately after the treatment showed a significant contrast medium stagnation in the aneurysm (Figs. 3B and 3C). The patient was discharged without any complications, and her symptoms gradually improved. Follow-up MR examinations were performed 6 months after the treatment. The T2WI axial MRI showed progressive thrombosis of the aneurysm (Fig. 1B). The silent MRA clearly showed the residual blood flow within the aneurysm (Fig. 4). The patient committed suicide likely due to depression 2 months after the 6-month follow-up MR examinations. An autopsy was performed with the patient's family's written consent. The autopsy specimen showed a small section of the defective membranes with the PED that matched the entry point of residual blood flow seen clearly in the silent MRA (Fig. 4). Macroscopic photographs and HE stained sections showed organized thrombus filling the aneurysm sac and defective endothelialization (Fig. 5, arrows). In contrast, complete endothelialization was observed in membranes covering the PED (Fig. 5, high magnification image).




Aneurysm occlusion after FD therapy occurs due to aneurysm sac thrombosis followed by endothelialization with the devices. But the mechanisms of endothelialization are still unclear.1) To our knowledge, there are no radiological modalities that can accurately and correctly evaluate endothelialization.1,2) In an animal model, complete aneurysm occlusion by DSA strongly suggested complete endothelialization.3,4) In humans, Griessenauer et al.5) used the term “collar sign” in the follow-up DSA images of incompletely occluded aneurysms after PED embolization. In their report, the optical coherence tomographic (OCT) images showed a great variability of endothelialization.5) Therefore, incomplete aneurysm occlusion suggests defective endothelialization with the device. Antiplatelet therapy after FD therapy is mandatory, but the optimal timing for stopping the therapy remains controversial. Complete endothelialization is an important indication to safely stop antiplatelet therapy. When the DSA shows incomplete aneurysm occlusion, stopping the antiplatelet therapy might cause severe thromboembolic complications due to thrombus formation at the contrast medium entry point which is not endothelialized.6) Because repeated DSA examinations are invasive for patients, a less invasive imaging modality has been needed. Oishi et al.7) reported the usefulness of silent MRA for intracranial aneurysms treated with the PED. In the present case, the 6-month follow-up silent MRA showed residual blood flow within the aneurysm. The macroscopic autopsy findings showed a portion of defective endothelialization that matched the entry point of residual blood flow depicted with the silent MRA. Therefore, silent MRA findings after PED embolization are helpful to determine the optimal timing for stopping antiplatelet therapy.
Macroscopic autopsy findings after FD therapy showed defective endothelialization that perfectly matched and corroborated the silent MRA findings.
We thank the Laboratory of Molecular and Biochemical Research, Research Support Center, Juntendo University Graduate School of Medicine for technical assistance, and Akihide Kondo, MD, PhD.
No grant support regarding submitted manuscript.
No presentation in part or whole at any meeting regarding submitted manuscript.