2021 Volume 8 Issue 1 Pages 281-286
2021 Volume 8 Issue 1 Pages 281-286
Dorsal arachnoid web (DAW) is a rare entity, which has been reported only in the thoracic spine. The authors report the first case of DAW developing in the cervical spine. A 78-year-old man with several-year progressive gait disturbance and bilateral lower-extremity numbness was referred to our hospital on the suspicion of a non-enhancing cystic cervical spinal tumor. Magnetic resonance imaging (MRI) showed a focal indentation along the dorsal surface of the spinal cord at C7 associated with widened cerebrospinal fluid (CSF) space and increased T2-weighted signals in the cord at C5–C7. DAW was suspected, but because of the atypical location for DAW, computed tomography (CT) myelogram was performed and demonstrated an incomplete blockage of the CSF flow at C7 with neither visible abnormal membranes nor a cyst formation. Intraoperative ultrasonography and operative findings revealed that two fluttering membranes disturbed the CSF flow. The pathology of the excised membranes was arachnoid tissues. DAW should be suspected based on the characteristic MRI findings even if the location is in the lower cervical spine. This case seems to support the theory that DAW may be an incomplete or disrupted formation of an arachnoid cyst.
Dorsal arachnoid web (DAW) is a rare entity, which was first reported by Mallcci et al.1) in 1997. DAW represents a subarachnoid extramedullary transverse band of arachnoid tissue connecting between the ventral surface of the arachnoid membrane and the dorsal surface of the spinal cord, which blocks the cerebrospinal fluid (CSF) flow in the longitudinal direction and widens the dorsal CSF space associated with increased pressure of CSF and a local mass effect, resulting in a dorsal indentation and anterior displacement of the cord to cause myelopathy.2,3) DAW has been reported only in the thoracic spine with a predilection for the upper thoracic spine, although there is no clear explanation for the localization of DAW.4) The authors here report the first case of a cervical DAW.
A 78-year-old man with a history of cervical spondylosis and lumbar degenerative spondylolisthesis presented with progressive gait disturbance and bilateral lower-extremity numbness for several years. As the patient underwent contrast-enhanced magnetic resonance imaging (MRI) and was suspected of a non-enhancing cystic tumor of the cervical spine in a local hospital, he was referred to our hospital.
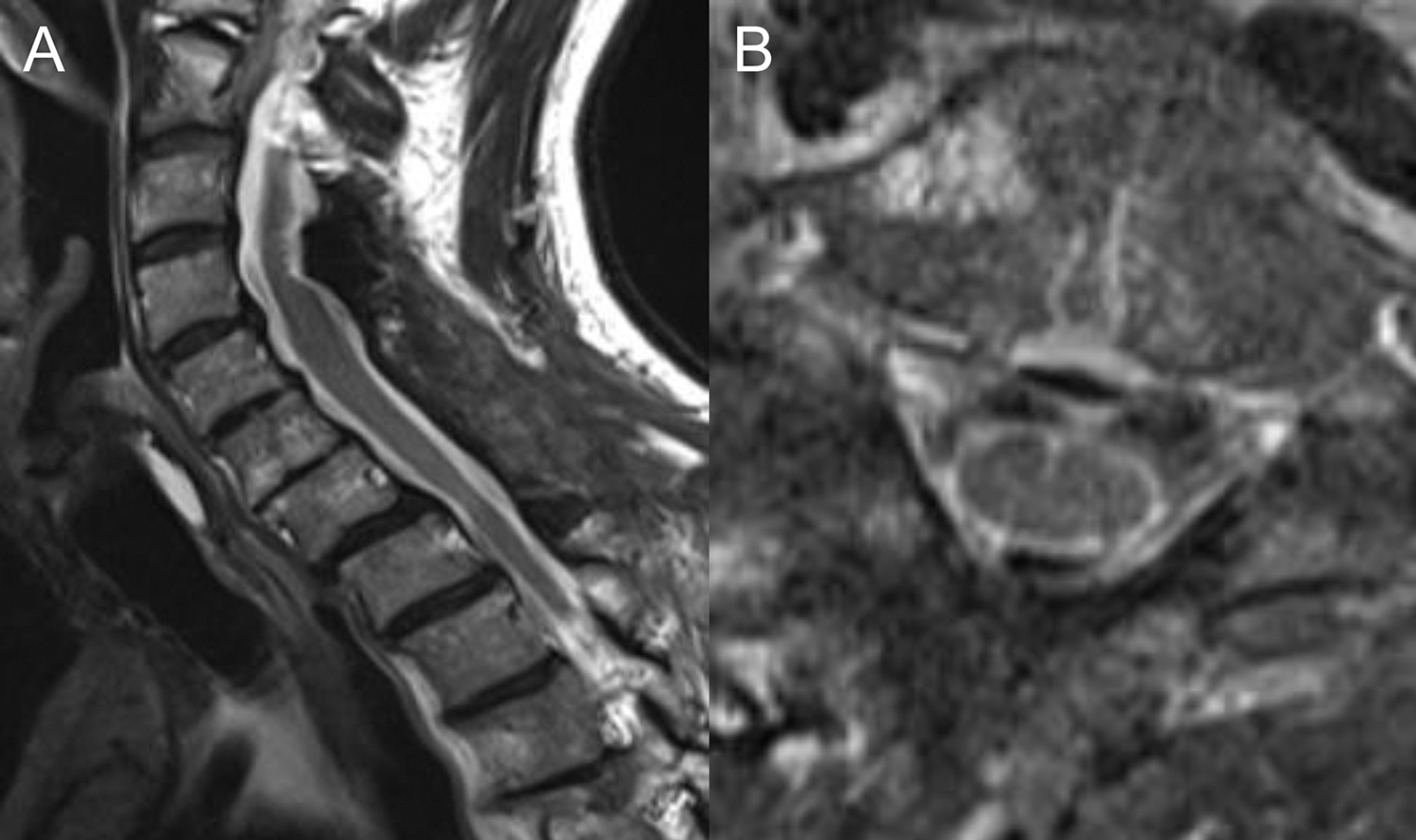
On admission, neurological examination, mild weakness, and reduced tactile sensation in the bilateral lower extremities were revealed in association with increased patellar deep tendon reflexes, normal Achilles reflexes, and negative Babinski reflex. T2-weighted MRI showed a dorsal indentation of the cervical spinal cord at C7 and intramedullary high intensity at C5–C7 with widened dorsal CSF space but neither a suspected arachnoid band nor a cystic lesion (Figs. 1A and 1B), in addition to the cervical spinal canal stenosis. As DAW was suspected but the location was atypical, computed tomography (CT) myelograms were performed via a lumbar tap. CT myelograms at 30 minutes after an injection of a contrast medium demonstrated an incomplete blockage of the CSF flow at C7 with no visible causes (Figs. 1C and 1D), leading to a definitive diagnosis of DAW taken together with MRI findings.

C6–T1 laminectomies for DAW as well as C3 laminectomy and C4–C5 laminoplasties for cervical spinal canal stenosis were performed. Intraoperative ultrasonography on the dura mater clearly showed that the spinal cord was compressed ventrally by the expanded CSF space, and that two membrane-like structures (cranial and caudal membranes) in the dorsal subarachnoid space were fluttering within the CSF flow at C7 (Figs. 2A–2D). After a midline durotomy was made, the thick and nebulous membranes were found to be fluttering in synchronization with the cardiac cycle at 60 beats per minute, seeming to block the CSF flow. When the arachnoid membrane was cut rostrally to the thick cranial membrane and CSF flowed out from there, the CSF space below the cranial membrane was not collapsed but was pulsating, and the caudal membrane was observed pulsating in the same way through the cranial membrane (Figs. 2E and 2F). The two membranes, which looked like a bag opening below and were continuous on the lateral, were excised together, and the pathology was arachnoid tissues.

The postoperative course was uneventful. One-week and 3-month MRIs showed that both spinal cord compression and the intramedullary lesion were improved (Figs. 3A and 3B). His gait disturbance was gradually improved, and he was able to walk without any help at 3 months after surgery.
DAW is a rare lesion, which impairs the CSF flow, compresses the spinal cord ventrally by the dorsally expanded CSF space, and causes slowly progressive myelopathy.3) DAW is sometimes complicated with syringomyelia.5) DAW occurs in 4th–7th decades with a male predominance.4) DAW has characteristic image findings called the scalpel sign, which is named because the mass effect on the dorsal spinal cord from the accumulated CSF is similar to a surgical scalpel with its blade pointing posteriorly on sagittal MRI and CT myelograms.2) The scalpel sign is a finding that can suspect the existence of DAW from the spinal cord deformity and obstructed CSF flow. The differential diagnosis of the scalpel sign includes dorsal arachnoid cyst and ventral spinal cord herniation, both of which can be distinguished from DAW: the former has a cyst, which can be more clearly diagnosed by CT myelogram, whereas the latter has a C-shaped indentation on the dorsal spinal cord, no CSF space on the ventral side of the spinal cord, and a rare coexistence of syringomyelia, unlike DAW.6) Thus, most of preoperative diagnoses of DAW were made based on the scalpel sign with or without syringomyelia on MRI and/or CT myelograms.2,7–13) In contrast, the identification of an extra-medullary transverse band of arachnoid tissue connecting between the ventral surface of the arachnoid membrane and the dorsal surface of the spinal cord is pathognomonic for DAW, but is impossible on preoperative MRI and CT myelograms in most of the cases, possibly because DAW is a continuously fluttering thin membrane.3) As far as we know, the arachnoid band indicating DAW was identified on preoperative images only in two cases.3,14) Fujiwara et al3) diagnosed double DAWs preoperatively using cardiac-gated phase-contrast cine-mode MRI. Grewal et al14) identified DAW preoperatively on a heavily T2-weighted constructive interference in steady state (CISS) sequence. Although these images have improved the sensitivity in diagnosing DAW, they cannot reliably diagnose DAW. Chang et al15) reported that quantitative CSF flow analysis by cardiac-gated phase-contrast cine-mode MRI in multiple axial planes could localize the obstruction of CSF flow on the dorsal side of the spinal cord and reveal a one-way valve-like function of the DAW, although cardiac-gated phase-contrast cine-mode MRI in the sagittal plane failed to show a distinct blockage of rostrocaudal CSF movement in the subarachnoid space: the technique may allow neurosurgeons to successfully excise the DAWs through limited surgical exposure. In the present case, the scalpel sign suggested DAW, but because of the atypical location and no visualization of the arachnoid band, a tumor was suspected and contrast-enhanced MRI was performed in a local hospital.
In the literature, the location of DAW was described in 37 cases.2–21) In all the cases, the location of the lesion was in a thoracic segment: T1 in two cases,16,17) T1/2 in one case,5) T2 in one case,14) T3 in six cases,2,4,6,7,10) T3/4 in two cases,6,17) T4 in six cases,2,3,6,12,15) T4/5 in one case,19) T5 in three cases,2,5,19) T5/6 in one case,20) T6 in four cases,2,16,18) T7 in five cases,2,6,13,21) T7/8 in two cases,9,11) T8 in one case,7) T8/9 in one case,9) and T11 in one case.8) The reason of the predilection for the thoracic spine is unknown.2) Although the etiology of DAW also remains unknown, one of the promising hypotheses is that DAW may be an incomplete or disrupted formation of an arachnoid cyst.2) That is, the dorsal location of DAW may be related to the theory of arachnoid cyst formation from diverticulations of the septum posticum, a thin membrane that longitudinally divides the posterior subarachnoid space.21,22) The septum posticum is an increasing number of overlying arachnoid membrane strands, which start at C5 to T1 and continue down to the lumber enlargement (T12) until becoming thinner and fenestrated.23) Nisson et al19) theorized that the septum posticum is altered in a specific environment to have a complex structure and to block the CSF flow. According to the theory, DAW can develop in the lower cervical spine (C5−C7) as well as the thoracic spine, because the septum posticum arises from C5−T1. In this case, two membranes were found on intraoperative ultrasonography like a case reported by Fujiwara et al,3) supporting the theory that DAW may be an incomplete or disrupted formation of an arachnoid cyst.
In the present case, after a midline durotomy was made, the thick and nebulous membranes were found to be fluttering at 60 beats per minute, suggesting the synchronization with the cardiac cycle. CSF flow is reported to be generated by the systolic pulse wave and rapid respiratory waves.24) Kudo et al. reported that the CSF pulse flow went from caudal to cranial directions during early diastole, and from cranial to caudal directions during early systole in the upper cervical canal.25) In our case, the authors consider that the caudal-to-cranial CSF flow during early diastole was obstructed by a one-way valve mechanism that trapped CSF by the two membranes, resulting in the configuration of the DAW looking like a bag opening below and causing progressive cord compression like previously reported cases.7,15)
It is notable that most of the patients with DAW had neurological improvement immediately after the operation and before discharge, even if preoperative symptoms lasted for 1 year or longer.19) The treatment for 37 cases described above was laminectomy with excision of DAW in 30 cases,2,4–12,14,15,17–21) laminectomy with shunt placement in 4 cases,3,16) and unknown in 3 cases:6,13) 35 cases showed improvement in a neurological status following surgery,2–15,16–21) while only 2 cases had no improvement.16,17) The information of follow-ups was provided in 24 of 37 cases, and the average duration was 12.8 months.2,5–9,11,14,16,17,19,20) Although there was no report of recurrent cases during the follow-up period, further longer follow-ups would be needed. Our case also had a good neurological recovery after surgical treatment irrespective of several-year progressive neurological deterioration including gait disturbance.
In conclusion, we reported the first case of a cervical DAW. DAW should be suspected based on the characteristic MRI findings even if the location is in the lower cervical spine.
All authors report no conflicts of interest regarding this article.