2021 Volume 8 Issue 1 Pages 651-656
2021 Volume 8 Issue 1 Pages 651-656
A 57-year-old woman who presented with a sudden severe headache and subsequently diagnosed with a subarachnoid hemorrhage was referred to our hospital. CTA revealed a large irregularly shaped dissecting aneurysm of the right vertebral artery (VA) and a small round distal aneurysm of the right posterior inferior cerebellar artery (PICA), which originated just proximal to the VA aneurysm. We diagnosed the VA aneurysm as a ruptured aneurysm and performed endovascular treatment the day the patient was hospitalized. Because the left VA was aplastic, stent-assisted coiling was performed to preserve the blood flow of the right VA, following the administration of antiplatelets and heparin. The proximal part of the laser-cut closed-cell stent jailed the orifice of the right PICA. The postoperative course was uneventful, and she was discharged from the hospital 3 weeks later without any neurological deficits. The follow-up VA angiogram revealed complete disappearance of the distal PICA aneurysm 17 months after stent jailing. Flow reduction by stent jailing of the arterial orifice is considered to be the main mechanism of aneurysmal shrinkage. Jailing of the orifice of the cerebral artery using even a low-metal-coverage stent may cause arterial flow reduction, which may shrink a distal aneurysm.
Shrinkage of large and giant cerebral aneurysms due to intra-aneurysmal thrombosis has been reported in 13–20% of these cases, while 1–2% of small ruptured cerebral aneurysms disappear due to intra-aneurysmal thrombosis following subarachnoid hemorrhage (SAH) and subsequent vasospasm.1–3) Unlike large or ruptured aneurysms, a spontaneous shrinkage of unruptured small cerebral aneurysms has been reported as extremely rare.4) In contrast, flow-related unruptured small aneurysms harboring the feeding arteries of cerebral arteriovenous malformations (AVMs) are frequently reported to shrink or disappear following the treatment of AVMs.5,6)
Herein, we report a rare case of a small unruptured aneurysm of the distal posterior inferior cerebellar artery (PICA) that gradually shrank and disappeared following stent jailing of the orifice of the PICA. The mechanisms of aneurysmal shrinkage, differential diagnoses of the rupture site, and treatment strategies for multiple aneurysms accompanied by SAH are discussed.
A 57-year-old woman experienced an occipital headache 20 days prior to her referral to our hospital, and a Computed Tomography (CT) scan performed at a private clinic revealed no intracranial abnormalities. She complained of severe headache again 1 day prior to referral, and a CT scan performed at the same clinic revealed SAH (Fig. 1A–1C). On admission, she had no history of hypertension or other diseases, and her routine preoperative evaluation results were within normal ranges. CTA and vertebral artery (VA) angiography revealed two cerebral aneurysms, a large irregular and pearl-and-string-shaped dissecting aneurysm (maximum diameter, 16.6 mm) of the right VA and a small fusiform aneurysm (maximum diameter, 6.2 mm) on the lateral medullary segment of the right PICA (1.4 mm diameter), which originated just proximal to the right VA aneurysm (Fig. 1D and 1E).
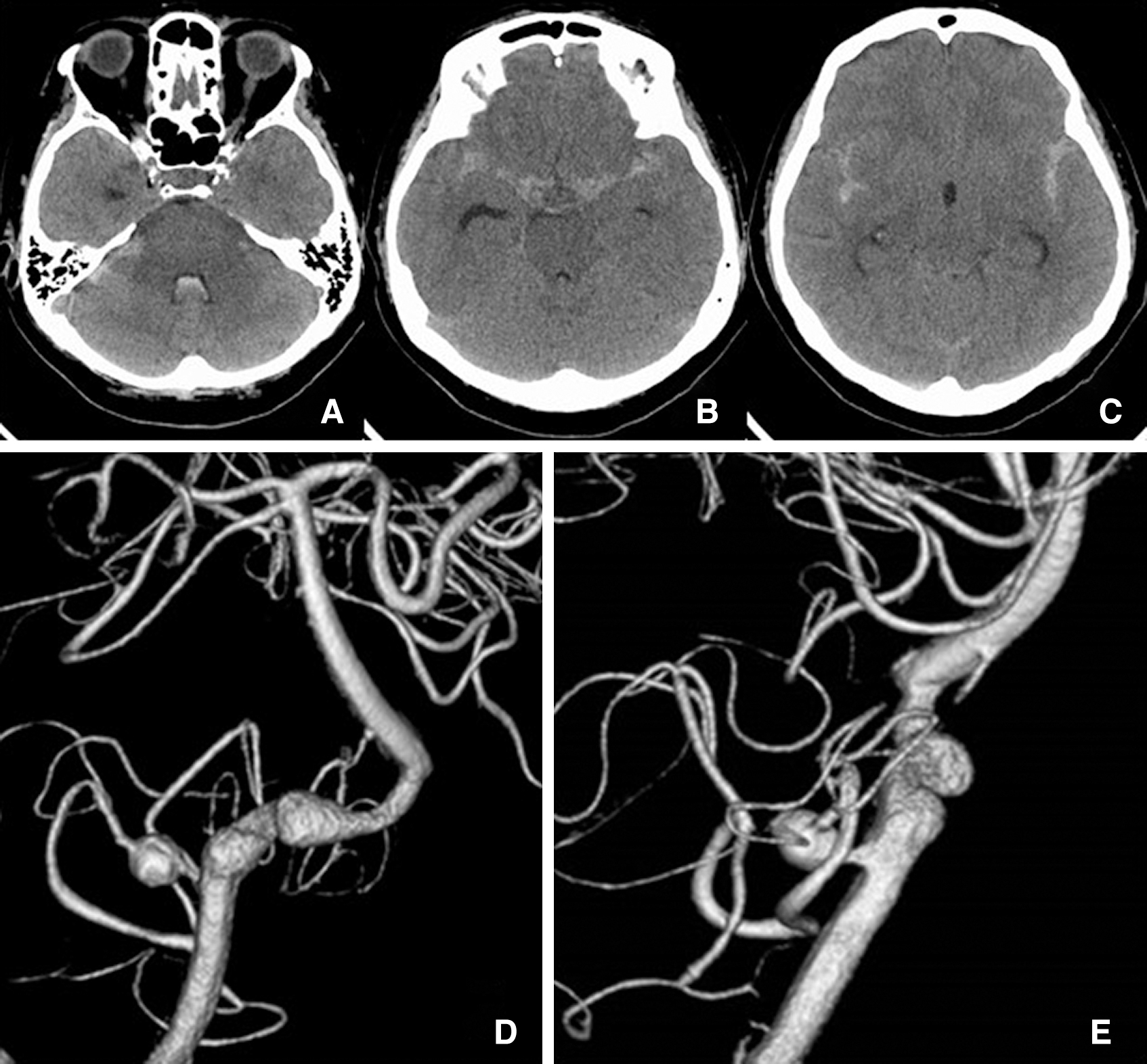
The CT scan from the clinic revealed a diffuse distribution of SAH around cisternal spaces, except for predominant clotting in the right cerebellopontine cistern (Fig. 1A). Because the right VA aneurysm had an irregular shape and a larger maximum size than the PICA aneurysm, we diagnosed the VA aneurysm as a ruptured aneurysm and the PICA aneurysm as an unruptured aneurysm. Subsequently, we decided to perform endovascular treatment of the right VA aneurysm on the day the patient was hospitalized and observe the PICA aneurysm conservatively. Because the left VA was hypoplastic, we performed stent-assisted coiling for the VA aneurysm, preserving the blood flow of the right VA.
Following femoral sheath insertion under general anesthesia, systemic heparinization was initiated until an activated clotting time of approximately 250 s (twice the pre-heparinization) was achieved. As an antiplatelet treatment, powdered aspirin (100 mg) was administered via a gastric tube, and continuous intravenous infusion of ozagrel sodium (80 mg) was initiated. Using the jailing technique, a closed-cell laser-cut stent, Enterprise 2 vascular reconstruction device (VRD 4.0 × 30 mm; Cerenovus, Irvine, CA, USA), was deployed from the VA union to the proximal side of the orifice of the right PICA following the insertion of a microcatheter into the aneurysm. The proximal portion of the stent subsequently jailed the orifice of the right PICA. Three target detachable coils (Stryker, Fremont, CA, USA) were inserted into the aneurysm, preserving the origin of the anterior spinal artery (Fig. 2A–2D).

Postoperatively, intravenous heparin (15000 U), intravenous ozagrel sodium (80 mg twice daily), and oral clopidogrel (75 mg) and aspirin (100 mg) were administered for 1 day, 2 days, and per day for 3 months, respectively, followed by single antiplatelet therapy with clopidogrel (75 mg/day) for an additional 9 months.
The patient’s postoperative course was uneventful, and she recovered without any neurological deficit and was discharged 3 weeks after the operation. The postoperative angiographies were repeated at 7 days, 6 weeks, and 3 months after the operation. Although no remarkable change of the aneurysmal size of right PICA was seen until 3 months after the operation, the stagnation of contrast medium in the PICA aneurysm persisted to the venous phase 6 weeks (Fig. 2E and 2F) and 3 months after the operation. Angiograms performed 11 and 17 months later revealed moderate shrinkage (Fig. 2G) and complete disappearance of the PICA aneurysm (Fig. 2H), respectively. The angulation of right VA was gradually straightened, and the angle of the right PICA against the right VA slightly sharpened following the stent placement (Fig. 2C–2H).
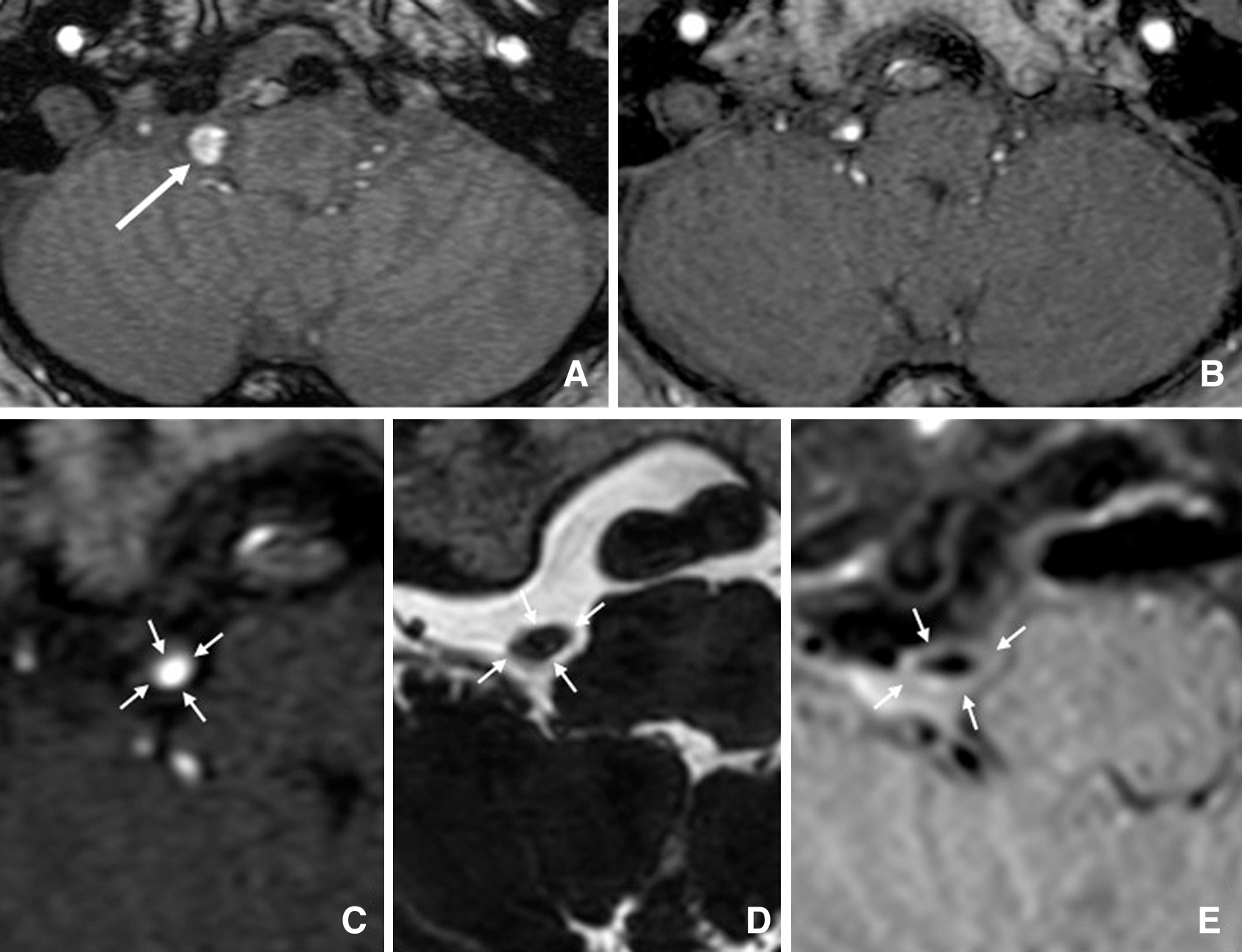
Time-of-flight MRA (TOF-MRA) images obtained at 3 weeks (Fig. 3A) and 39 months (Fig. 3B) following stent jailing revealed aneurysmal shrinkage. Figure 3C–3E shows MRIs at 39 months after stent jailing, comparing TOF-MRA (Fig. 3C), heavily T2-weighted imaging (Fig. 3D), and contrast-enhanced magnetic resonance vessel wall imaging (MR-VWI) (Fig. 3E) of the same lateral medullary segment of the right PICA. The TOF-MRA represents the inside of the artery, the heavily T2-weighted imaging indicates the outside of the artery, and MR-VWI shows the wall of the artery, which indicated no thickness or thrombosis of the wall of this segment.
To the best of our knowledge, this report presents the first case of a small and round unruptured fusiform aneurysm that disappeared following stent jailing of the orifice of the parent artery.
Upon observing multiple aneurysms in this patient experiencing SAH, we tried to distinguish the ruptured aneurysm from the other unruptured aneurysm because simultaneous treatment of all the aneurysms in the acute phase was considered difficult due to the invasive nature of aneurysm surgery. The distribution of the clot from a SAH or the existence of an intracerebral hematoma often indicates a ruptured aneurysm. When the clot distribution is homogenous, the morphology of aneurysms is compared, and aneurysms with a larger diameter and/or an irregularly shaped dome are diagnosed as ruptured.7–9) Recently, Matouk et al.10) reported that ruptured aneurysms demonstrated thick vessel wall enhancement on MR-VWI, while associated unruptured aneurysms did not exhibit this finding. MR-VWI has also been reported to support morphological evidence to differentiate between ruptured and unruptured aneurysms.10) Although contrast enhancement of the aneurysmal wall is often associated with atherosclerotic, degenerated, and thickened wall structures, MR-VWI, if performed on this patient, could play an important role in the differential diagnoses of the aneurysms in the acute phase.11,12)
Because the left VA was hypoplastic, we selected stent-assisted coiling for the right VA aneurysm, which was diagnosed as ruptured. To prevent thromboembolic complications, loading of antiplatelets and systemic heparinization are considered useful,13,14) and peri- and postoperative hemorrhagic complications are of concern. However, a meta-analysis of internal trapping and stent-assisted coiling15) for ruptured VA dissecting aneurysms indicated that there was no significant difference in long-term occlusion, good clinical outcome rates, recurrence rates, and perioperative mortality.
The right VA aneurysm was irregularly shaped, and it was difficult to determine the bleeding point of the aneurysm. Therefore, we selected the most enlarged dome as a rupture point and packed it tightly with platinum coils following the deployment of a laser-cut closed-cell stent. The length of the stent used was 30 mm, and the orifice of the right PICA was jailed because the length of the proximal part of the stent had to be more than 5 mm from the proximal edge of the right VA aneurysm.
Enterprise2 VRD, used in this patient, has been reported to have a lower metal coverage and flow reduction effect than other closed-cell braided stents and flow diverters.16,17) However, the angulation of the right VA was gradually straightened, and the angle of the right PICA against the right VA slightly sharpened following the stent placement. These effects may have contributed to the cure of the VA aneurysm and the shrinkage of the PICA aneurysm.18)
Flow diverter stents have been reported to commonly produce the caliber reduction and occlusion of covered cortical branches, following stent deployment on small cerebral artery aneurysms.19) Although stent-assisted coiling for cerebral aneurysms is a widely accepted treatment, the jailing of cerebral arteries by a stent, even when using a low-metal-coverage stent, may produce some degree of flow reduction.
The treatment alternatives for right distal PICA aneurysm in the acute phase are stent-assisted coiling, which preserves the flow of the right PICA, or trapping and bypass surgery. Because the diameter of the right PICA was small, and the PICA was angled at the aneurysmal portion, we found stent-assisted coiling of the PICA aneurysm in the acute phase to be contraindicated. Conversely, staged treatment of PICA aneurysms using bypass surgery in the chronic phase has been reported and could be an alternative.20)
Because the PICA aneurysm may have ruptured, we repeated the angiography after the operation. Although the size and morphology of the PICA aneurysm did not change until 3 months after the operation, the stagnation of contrast medium persisted to the venous phase at 6 weeks and 3 months after the operation. The straightened angulation of the right VA and the sharpened angle between the right PICA and the right VA following the stent placement were also apparent. We assume that these findings may indicate that the mechanisms contributed to the shrinkage of the PICA aneurysm and the mechanisms of flow reduction mimicked the shrinkage of flow-related aneurysm following the treatment of AVMs. Although the MRI findings performed 39 months after the operation indicated no thrombosis of the PICA aneurysm, the occurrence of partial thrombosis inside the aneurysm between 3 and 39 months after the operation cannot be excluded.
The authors thank Dr. Yoji Tanaka for his valuable contribution concerning the MRI findings.
None of the authors have conflicts of interest to declare.