2021 年 8 巻 1 号 p. 665-671
2021 年 8 巻 1 号 p. 665-671
A 50-year-old man and a 69-year-old woman with consciousness disturbance were diagnosed to have suffered from subarachnoid hemorrhage (SAH) involving the posterior fossa. In both cases, the initial 3D CT angiogram failed to reveal the SAH source in the vertebrobasilar system. Delayed 3D rotational angiography revealed aneurysms on unfamiliar aberrant arteries. One was a dissecting aneurysm located between the proximal part of the posterior inferior cerebellar artery and the distal part of the intracranial vertebral artery. It was trapped and resected; the patient subsequently presented with lateral medullary symptoms. The other aneurysm was between the distal posterior and the distal anterior inferior cerebellar artery. It was successfully embolized; there were no complications. We think that the aberrant aneurysm-harboring vessels encountered in these two patients were primitive arteries on or adjacent to the vertebrobasilar paramedian longitudinal axis and that they persisted past the embryologic stage. Such aneurysms arising from unfamiliar persistent arteries beside the brainstem are extremely rare but must be considered when the SAH source is not detected in the trunk of the vertebrobasilar system.
Advances in diagnostic imaging have led to the increased awareness of cerebral aneurysms in areas other than the arterial trunks. We encountered two patients with subarachnoid hemorrhage (SAH) from aneurysms in unfamiliar aberrant arteries on or adjacent to the rostral part of the paramedian longitudinal axis (PLA) present during vertebrobasilar development.1,2) One was a dissecting aneurysm located between the proximal part of the posterior inferior cerebellar artery (PICA) and the distal part of the intracranial vertebral artery (VA). The other aneurysm was between the distal PICA and the distal anterior inferior cerebellar artery (AICA). To the best of our knowledge, only one aneurysm involving the rostral part of the PLA, similar to ours, has been reported.3)
A 50-year-old man with a history of untreated hypertension was admitted after fainting in the rest room. At the time of admission, he was hypertensive; the Glasgow Coma Scale was 8, but no neurological focal signs were detected. Our preliminary diagnosis was SAH, World Federation of Neurosurgical Societies (WFNS) grade IV. A CT scan revealed diffuse SAH predominantly in the right cerebellomedullary cistern (Fisher grade 4). A bleeding source in the vertebrobasilar system was suspected, however, 3D CTA failed to show a bleeding source (Fig. 1A). Because of his severe aspiration pneumonia and pulmonary edema, we postponed selective angiography. He required intensive care under sedation. On day 18, selective angiography of the right VA was performed. On anteroposterior and lateral digital subtraction images, there was no evidence of vascular lesions (Fig. 1B and 1C). However, a 3D rotational image revealed a 2-mm diameter sphere on an aberrant tortuous artery that arose from the proximal part of the PICA (anterior medullary segment)4); it ran just medial and parallel to the VA and merged into the distal part of the VA (Fig. 1D and 1E). We judged this lesion to be the bleeding source and chose direct surgery because we expected super-selective catheterization for embolization to be difficult. On day 26, he underwent direct surgery; there had been no rerupture. We extended a lateral suboccipital craniotomy to the foramen magnum and traced the aberrant artery from its origin at the proximal part of the PICA to its distal tortuous and atherosclerotic part that was partly embedded in a clot (Fig. 2A). The tortuous part was trapped and removed (Fig. 2B); detachment from the clot was easy; however, several perforating arteries supplying the medulla oblongata had to be sacrificed. The histological diagnosis was dissecting aneurysm on the affected artery (Fig. 2C) associated with a false aneurysm in the clot (Fig. 2D). Postoperatively, the patient was hoarse, and manifested ataxia and a reduction in pain and temperature sensation on the ipsilateral face, the contralateral trunk, and the extremities, signs indicative of lateral medullary symptoms. An MRI study of the medulla oblongata was not possible due to clip artifact. We placed a lumboperitoneal shunt for hydrocephalus, and he underwent rehabilitation. The patient was discharged 10 months after SAH onset with persistent lateral medullary symptoms.
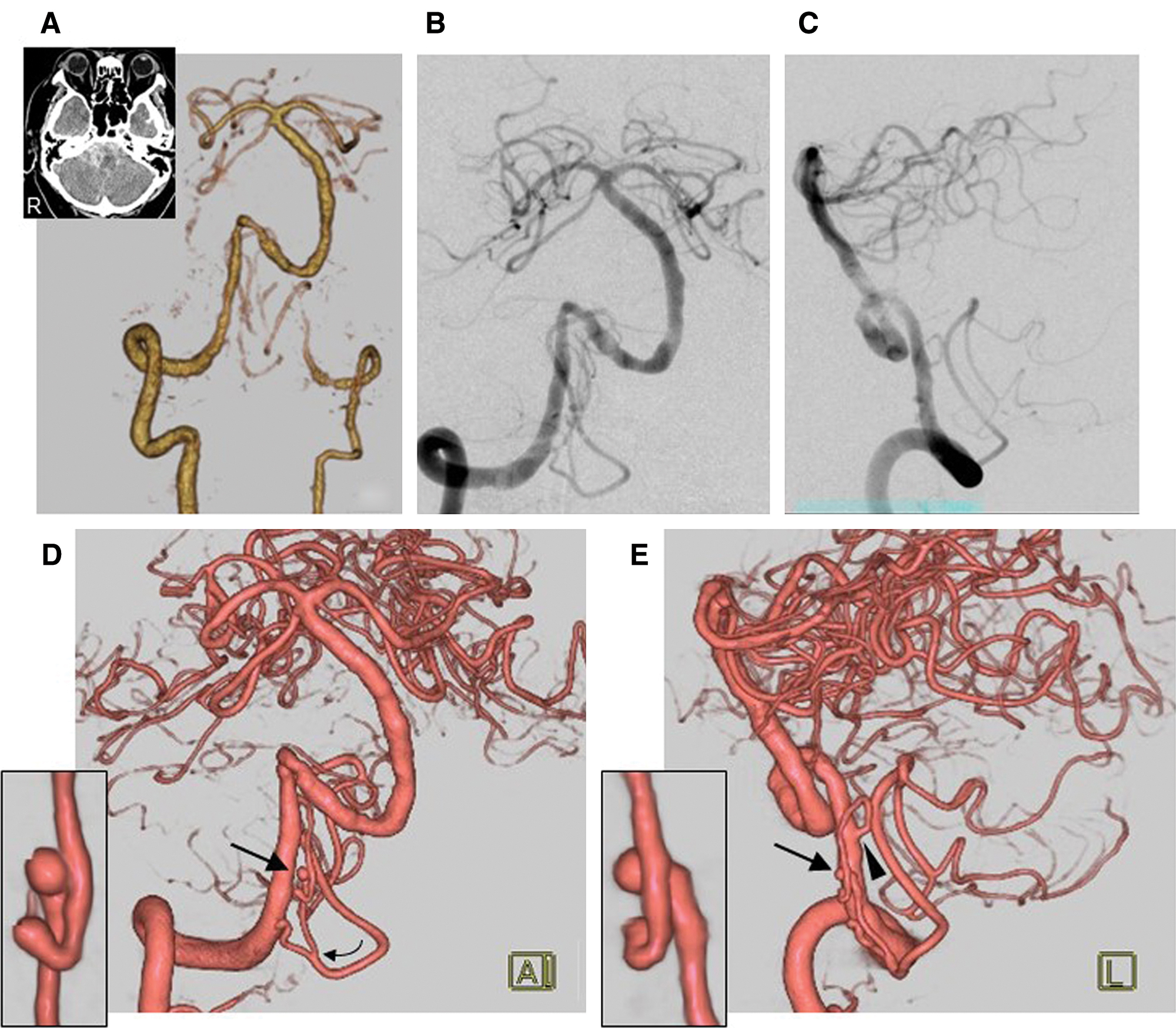
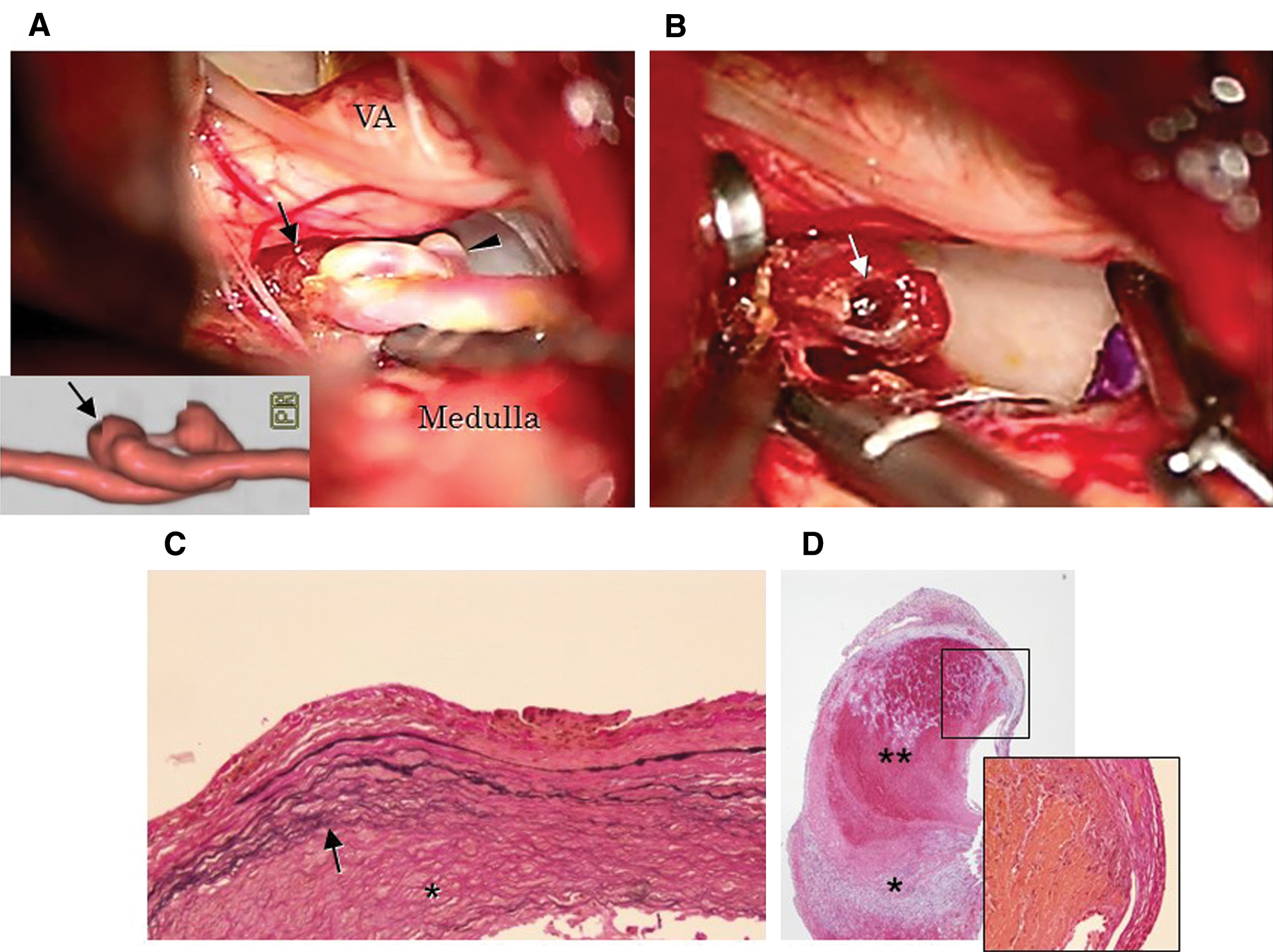
A 69-year-old woman with no relevant medical history was admitted for severe sudden-onset headaches. She was hypertensive; the Glasgow Coma Scale was 14, but there were no neurological focal signs. Based on CT findings, the preliminary diagnosis was SAH, WFNS grade II. The SAH was limited to the left ambient and quadrigeminal cisterns (Fisher grade 3). 3D CTA showed communicating segment carotid aneurysms on both sides. There were no apparent lesions in the vertebrobasilar system (Fig. 3A). The carotid aneurysm on the left was judged to be the bleeding source. It was clipped uneventfully; intraoperative inspection revealed no apparent evidence of rupture. On the 3rd postoperative day, she suddenly became stuporous. A CT scan revealed SAH predominantly in the posterior fossa and a thick clot in the left cerebellomedullary cistern. Selective angiography showed occlusion of the clipped aneurysm. Left vertebral anteroposterior and lateral angiograms showed an engorged vasculature adjacent to the VA in the arterial phase (Fig. 3B and 3C). On 3D rotational images, the lesion (maximum diameter 4.5 mm) arose from an aberrant artery between the distal part of the PICA (telovelotonsilar segment)4) and the distal part of the AICA (flocculopeduncular segment)4) (Fig. 3D). Judging this lesion to be the true source of the first and second bleeding, we performed endovascular surgery. A Marathon microcatheter (Medtronic Neurovascular, Irvine, CA, USA) with a Chikai micro-guidewire (Asahi Intec, Aichi, Japan) was introduced into the aberrant artery and two ED coils (Kaneka Medix, Osaka, Japan) were placed just proximal to the aneurysm. Then a small amount of a 17% n-butyl cyanoacrylate/lipiodol mixture was slowly injected (Fig. 3E and 3F). We confirmed complete occlusion of the lesion and patency of the trunk of the PICA and the AICA (Fig. 3G). Her postoperative course was uneventful, and she was discharged without deficits.

During the first 32–40 days of gestation, the approximate fetal length is 7–18 mm; seven primitive cervical segmental arteries (primitive form of the VA) connect with each other and to the longitudinal neural arteries (a pair of the primitive form of the basilar artery on the median longitudinal axis).1,2) During this developmental process, transient primitive vertebrobasilar anastomoses are present between the longitudinal neural arteries and the first cervical segmental arteries; they form the primitive vertebrobasilar system (Fig. 4A). On the PLA, a primitive lateral vertebrobasilar anastomosis connects the primitive VA, the stem of the PICA and the AICA, and the more cephalad stem of the cerebellar arteries. The disappearance of the anastomoses between the median longitudinal axis and the PLA leads to normal development (Fig. 4B) or to a variation in the vertebrobasilar arteries.5) There are three types of duplication of the intracranial VA (Fig. 4C), i.e., duplication within the VA, premedullary duplication of the VA harboring a duplication between the distal VA and the proximal basilar artery, and a duplication of the remnant of the primitive long tract anastomosis between the VA and the middle basilar artery.6–8)

In our patients, the aberrant arteries harboring the aneurysms may have been attributable to dysgenesis on or adjacent to the PLA (Fig. 4D). The configuration observed in Case 1 resembled a duplication in the VA. However, this should be distinguished from the typical duplication because the aberrant artery arose from the proximal part of the PICA trunk and its diameter was much thinner than that of the VA. Therefore, we suspect that this aberrant artery was a persistent form in the proximal part of the PICA stem that was situated between the two trunks with dominant flow, i.e., the VA and the PICA originating at the most proximal part of the intracranial VA along the PLA. The aberrant artery in Case 2 may have been a persistent primitive lateral vertebrobasilar anastomosis on the PLA. The aberrant arteries on or adjacent to the PLA, the lateral spinal artery,8) and the so-called vasa corona9) arteries, potential sites of aneurysm development, were ambiguous at a site aside the brainstem (Fig. 4E). The lateral spinal artery arises from either the VA or the PICA to supply the upper cervical cord.8) The vasa corona is a horizontal leptomeningeal collateral pathway between the lateral spinal artery and the anterior spinal artery.9) The caudal locations differ from those of the aberrant arteries we observed.
With respect to the PLA, aneurysms on the lateral spinal artery have been reported.10–14) However, only one other aneurysm rostral to the origin of the PICA has been documented.3) In their patient, the aberrant artery, called the bulbar artery, arose from the distal part of the intracranial VA to supply the PICA as one of the collateral pathways. Its course was similar to the course of the aberrant artery in our Case 1 although the reticular channels appeared to be more complex than those in our patient. They used endovascular glue embolization and encountered an infarct in the lateral part of the medulla oblongata. No other aneurysms in the rostral part of the PLA, true, false, or dissecting, have been reported. In Case 1, we observed a chronically grown dissecting aneurysm; it may have contributed to degeneration of the internal elastic lamina.15) The false aneurysm may have been due to the rupture of the dissecting aneurysm. Kurita et al.13) suggested that in their case, fragility of the lateral spinal artery on the PLA resulted in aneurysm development. The artery did not develop to compensate for occlusion or stenosis of the PICA or VA trunk, and it was not under hemodynamic stress. In our patients, the aberrant vessels did not represent collateral pathways because the distal connecting vessels were patent. We think that, as in their case, fragility of the aberrant artery may have led to aneurysm development.
We offer some suggestions for the management of such lesions. Diagnostically, 3D CTA and selective angiography with only anteroposterior and lateral images may be insufficient because the aneurysms may be small and overlap with the adjacent VA. The high resolution of 3D rotational angiograms helps to detect such lesions at optional angles and by subtracting adjacent obstacles. Complex lesions may also require evaluation on super-selective angiograms. The occlusion of such lesions is challenging because the aberrant parent artery that may supply the lateral part of the brain stem must be sacrificed. Direct surgery as in our Case 1 and endovascular surgery performed by Gabrieli et al.3) resulted in infarction. However, endovascular surgery performed in our Case 2 was curative without infarction.
In conclusion, we presented two patients with ruptured aneurysms on unfamiliar persistent arteries beside the brainstem. The vessels involved the embryologic development of the PLA. Such aneurysms must be carefully evaluated when the SAH source is not detected in the trunk of the vertebrobasilar system.
The authors have no personal financial or institutional interest in any of the drugs, materials, or devices in the article. All authors who are members of the Japan Neurosurgical Society (JNS) have registered online self-reported COI disclosure statement forms through the website for JNS members.