2022 年 9 巻 p. 31-35
2022 年 9 巻 p. 31-35
Because of nonspecific clinical and radiological findings, it is difficult to diagnose isolated neurosarcoidosis without histological examination. Distinguishing neurosarcoidosis from neoplasm, infectious disease, or granulomatous disease can be challenging.In this study, we present a case of a 61-year-old female who presented with unilateral blindness. Magnetic resonance imaging (MRI) revealed a large invasive mass lesion located in the neurohypophysis with homogeneous enhancement after the injection of gadolinium. The lesion involved the bilateral cavernous sinus, which extended along the dura of the skull base with leptomeningeal lesions. Contrast-enhanced computed tomography (CT) and fluorodeoxyglucose positron emission tomography/CT of the entire body showed no other lesions. Biochemical examinations showed no useful data, including angiotensin-converting enzyme, β-glucan, soluble interleukin-2 receptor, and T-SPOT. Cerebrospinal fluid examination revealed only the elevation of total protein. Under the preoperative diagnosis of a malignant tumor or metastatic tumor, followed by tuberculosis, fungal infection, or granulomatous disease, a biopsy was performed to immediately determine the appropriate therapy, which revealed the histological diagnosis of sarcoidosis. After steroid therapy, the lesions had markedly shrunk as observed on MRI, and the eyesight of the patient's right eye was completely restored. In this case, without a biopsy, discriminating between sarcoidosis and a malignant tumor was difficult. We believe that a prompt histological diagnosis of an invasive isolated neurohypophysial mass lesion involving the bilateral cavernous sinus, which is similar to a malignant tumor, is essential for selecting the appropriate therapy.
Sarcoidosis is an idiopathic multisystem inflammatory disorder characterized by the formation of noncaseating granulomas. The lung and intrathoracic lymph nodes are commonly involved, followed by the skin, eye, liver, and spleen, among other organs.1) Sarcoidosis is certain in patients with Löfgren syndrome or in those who underwent a biopsy of easily accessed organs, such as the skin and peripheral lymph nodes. Moreover, a transbronchial biopsy can diagnose pulmonary sarcoidosis.1) By contrast, the diagnosis of neurosarcoidosis (NS) without the involvement of any other organs may be challenging because of nonspecific clinical and radiological findings. In this study, we present the case of a patient with isolated neurohypophysial sarcoidosis involving the bilateral cavernous sinus with leptomeningeal and pachymeningeal lesions, which mimicked a malignant tumor.
A 61-year-old female was referred to our department with a neurohypophysial lesion on magnetic resonance imaging (MRI) associated with acute blindness in her right eye for 2 weeks. The patient did not have any medical history. Ophthalmological examination showed blindness in the right eye; however, the patient's visual acuity (vision with correction: oculus sinister 20/20) and left eye visual field were normal. No eye movement restriction and abnormal fundus or uvea findings were observed. The patient did not experience headache, ophthalmalgia, nausea, fever, neck stiffness, and consciousness disturbance. Neurological examination showed no abnormal findings, except for her right eye.
Endocrinological tests revealed panhypopituitarism and diabetes insipidus (DI). The administration of hydrocortisone (15 mg/day) and levothyroxine (25 μg/day) was initiated before biopsy, and on the day of the biopsy, desmopressin acetate hydrate (60 μg/day) was started. The serum level of the angiotensin-converting enzyme (ACE) was 13.4 U/L (normal range: 8.3-21.4 U/L). Other biochemical examination results were as follows: β-glucan, <6.0 ng/L (normal range: 0-11 ng/L); β-human chorionic gonadotropin, <0.2 IU/L (normal range: 0-3 IU/L); alfa-fetoprotein, 4.9 μg/L (normal range: 0-10 μg/L); soluble interleukin-2 receptor (sIL-2R), 505 U/mL (normal range: 121-613 U/mL); and T-SPOT (Oxford Immunotec, Oxford, UK), negative. The serum levels of tumor markers were normal. The results of cerebrospinal fluid (CSF) examination were as follows: initial pressure, 70 mmH2O; cell count, 5/μL including no atypical cells (normal range: 0-5/μL); total protein, 99 g/L (normal range: 15-45 g/L); glucose, 48 g/L (normal range: 50-80 g/L); Immunoglobulin G4 (IgG4), <60.0 mg/L; ACE, 0.8 U/L; and cultivation test, negative. Epstein-Barr virus (EBV) was not detected via polymerase chain reaction test.
Radiological findingsMRI demonstrated an invasive lesion located in the neurohypophysis, appearing as an isointense region on a coronal T1-weighted image (WI) (Fig. 1a), hypointense region on a coronal T2WI (Fig. 1b), and isointense region on a diffusion-WI (b-1000 and b-4000 s/mm2) in comparison with normal white matter. The coronal (Fig. 1c) and sagittal (Fig. 1d) gadolinium-enhanced T1WIs showed homogeneous enhancement of the lesion extending into the bilateral cavernous sinus and along the dura of the skull base. Intracranial leptomeningeal lesions were also found but not in the spinal cord cavity. Arterial spin labeling-based perfusion-WI showed no elevation of relative tumor blood flow. The ratio of choline to creatine and choline to N-acetylaspartate was elevated on single-voxel proton magnetic resonance spectroscopy (PRESS, TR 2000 msec, TE 144 msec). Computed tomography (CT) revealed an isodense lesion without abnormal calcifications and destruction of the skull base bone. Contrast-enhanced CT and fluorodeoxyglucose positron emission tomography/CT of the entire body showed no other lesions.

Initial coronal (a–c) and sagittal (d) magnetic resonance imaging results show an invasive neurohypophysial lesion as an isointense area on T1-weighted image (WI) (a) and a hypointense area on T2WI (b), with homogeneous enhancement on the T1WIs following gadolinium injection (c, d). The lesion extended into the bilateral cavernous sinus with multiple leptomeningeal and pachymeningeal lesions. The right side of the chiasma was swollen and showed high intensity on T2WI (b).
Under the preoperative diagnosis of a malignant tumor or metastatic tumor, followed by tuberculosis, fungal infection, IgG4-related disease, and granulomatous disease, a biopsy was performed through the right nostril under endoscopic observation to immediately determine the appropriate therapy. The bone of the sellar floor was drilled out, and the dura mater was cut. The anterior pituitary gland was observed behind the dura mater. After incising the thin anterior pituitary gland, a yellowish-white lesion was found. Biopsy specimens were obtained from the lesion, which was hard but not hemorrhagic.
Histopathological findingsHistological examination revealed multiple small granulomas with focal hyalinized fibrous tissue and infiltration of lymphocytes. Noncaseating granulomas showed the presence of epithelioid cells, and several multinucleated giant cells were observed (Fig. 2a). Immunohistochemically, the epithelioid and multinucleated giant cells were positive for cluster of differentiation 68 (CD68) (Fig. 2b), CD163, and s-100p; however, they were not immunoreactive to CD1a (Fig. 2c) and EBV-encoded small RNA in situ hybridization. The rate of IgG4-positive plasmacytes was below 6%. Fungus or acid-fast bacterium was not found. These immunohistochemical findings were consistent with those of sarcoidosis.
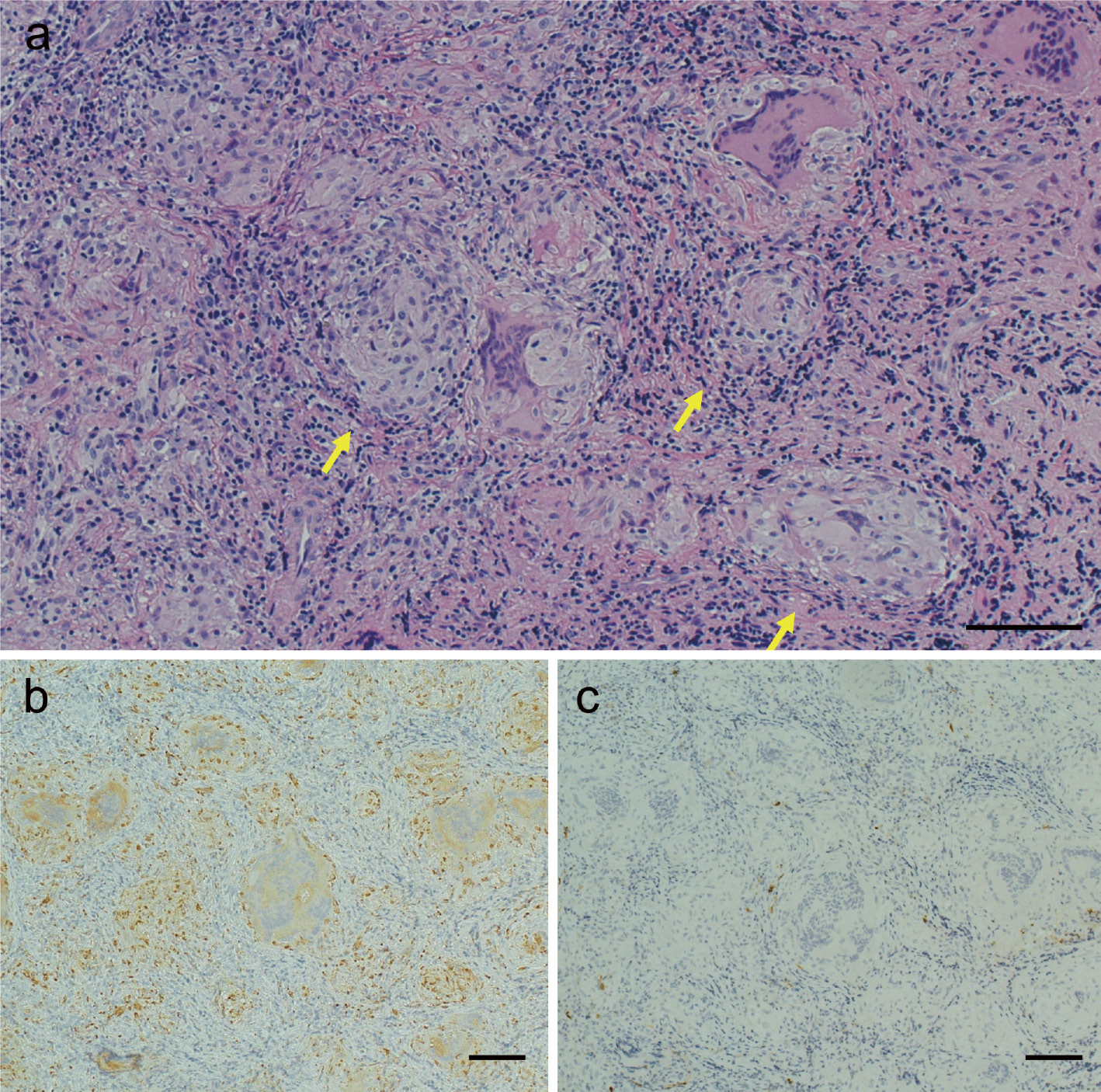
Photomicrographs of the tumor. Hematoxylin and eosin staining (a) revealed multiple small granulomas with focal hyalinized fibrous tissue and infiltration of lymphocytes. Noncaseating granulomas (arrow) showed epithelioid cells, and many multinucleated giant cells were observed. Immunohistochemically, the epithelioid and multinucleated giant cells were positive and negative for CD68 (b) and CD1a (c), respectively. Original magnification, ×100; bar, 100 μm.
Hydrocortisone (100 mg) was injected after obtaining the lesion, and hydrocortisone (30 mg) was administered on postoperative day 1 as a steroid cover therapy. Hydrocortisone replacement was tapered to 15 mg/day on postoperative day 5. DI became obvious on the day of biopsy, which was considered masked DI. The patient's visual function had gradually improved from postoperative day 1, although the lesion was not debulked enough to decompress the chiasm. The patient received steroid pulse therapy from postoperative day 16 (methylprednisolone 1 g daily for 3 days), followed by the administration of prednisolone 30 mg/day. The eyesight of the patient's right eye was completely restored after the steroid pulse therapy (vision with correction: oculus uterque 20/20), and the lesion had markedly shrunk as observed on MRI performed on postoperative day 49 under the administration of prednisolone 30 mg/day (Fig. 3).
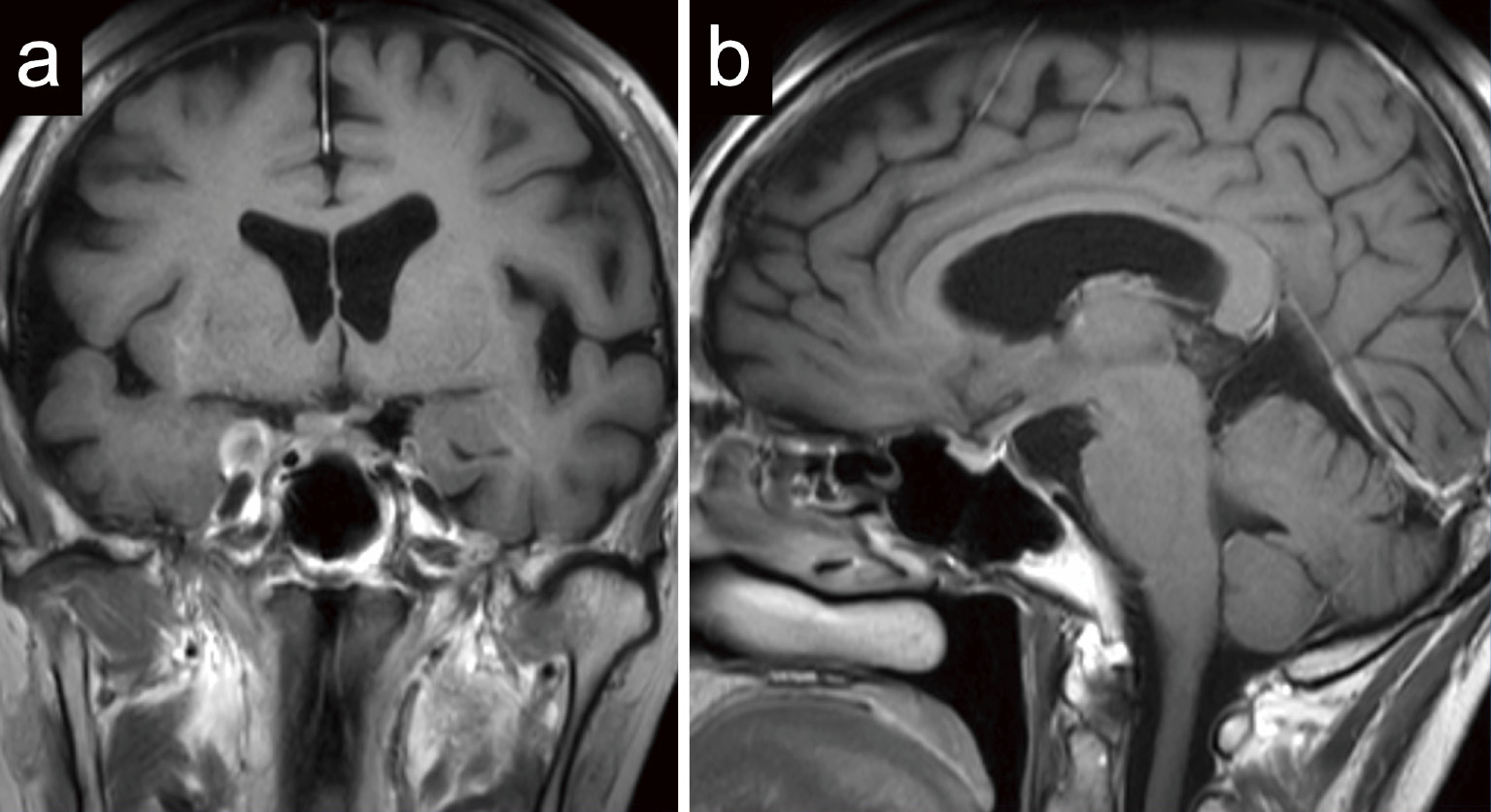
Coronal (a) and sagittal (b) gadolinium-enhanced T1-weighted images, which were obtained 49 days after the biopsy, revealed that the neurohypophysial lesion had markedly shrunk and the leptomeningeal and pachymeningeal lesions had disappeared.
In this study, we present a case of an isolated neurohypophysial sarcoidosis, involving the bilateral cavernous sinus with leptomeningeal and pachymeningeal lesions. The central nervous system is involved in up to 25% of the patients with systemic sarcoidosis during autopsy.1) Nonetheless, isolated NS is rare and reported to occur in 3.6% of the patients with NS.2)
In patients with NS, the hypothalamic-pituitary axis is often involved, which is considered secondary to proximity to basal meninges.3) Furthermore, imaging reveals the extending meningeal lesions surrounding the hypothalamic-pituitary axis. By contrast, sarcoidosis involving the cavernous sinus is rare,3) with only four patients reported thus far.4-7) Nevertheless, the definition of the involvement of the cavernous sinus was obscure. NS can often appear in the cerebral meninges;2,8) wherein the lateral wall of the cavernous sinus can be involved in NS. NS involving the cavernous sinus appears to have the thickness of the lateral wall of the cavernous sinus in literature. In other words, NS extending into the cavernous sinus may be extremely rare. To the best of our knowledge, this is the first report that describes NS forming a large intracavernous sinus mass lesion.
The diagnosis of NS is challenging in some cases because of nonspecific clinical and radiological findings. Saltijeral et al. have described a case of NS with leptomeningeal enhancement mimicking malignancy, similar to the patient in this case report.9) Furthermore, Deguchi et al. have reported a case of NS requiring differentiation from tuberculous meningitis.10) Based on the finding by Kidd et al., who have reported that 14% and 40% of the patients with NS had pachymeningeal and leptomeningeal lesions, respectively,2) NS can have pachymeningeal and leptomeningeal lesions mimicking malignant tumors or other diseases. Furthermore, the patient in this case report had a large invasive mass lesion at the neurohypophysis involving the bilateral cavernous sinus besides the pachymeningeal and leptomeningeal lesions, making it difficult to distinguish NS from a malignant tumor.
The elevation of ACE levels is indicated as a diagnostic biomarker of sarcoidosis.11) However, the test is insufficiently specific and sensitive in both serum and CSF to be useful.1,12-14) There are still no conclusive markers for diagnosing sarcoidosis. Hence, the clinical diagnosis of isolated NS remains unresolved. Biopsy still plays an important role in developing a correct and prompt diagnosis of NS.12,14)
Steroid replacement should be carefully conducted for patients with adrenocortical insufficiency because the steroid administration could cause spontaneous regression of some types of intracranial lesions: malignant lymphoma, germinoma, and IgG4-related disease, in addition to sarcoidosis. To obtain an accurate histological diagnosis of the neurohypophysial lesion, a biopsy should be promptly performed under minimum steroid replacement.
In this study, we reported a case of an isolated NS that formed a large neurohypophysial mass lesion involving the bilateral cavernous sinus. Discriminating between sarcoidosis and a malignant tumor was difficult without performing a biopsy on the patient in this study. We believe that having a prompt histological diagnosis of an invasive isolated neurohypophysial lesion, similar to a malignant tumor, is essential for selecting the appropriate therapy.
This study was partially supported by JSPS KAKENHI Grant Number JP19K17987. The authors would like to thank Enago (www.enago.jp) for the English language review.
The authors declare that they have no conflict of interest. Yasuyuki Kinoshita, Akira Taguchi, Fumiyuki Yamasaki, and Koji Iida have registered online Self-reported COI Disclosure Statement Forms through the website for JNS members.