2022 年 9 巻 p. 25-30
2022 年 9 巻 p. 25-30
A 36-year-old woman presented with sudden onset of a right-sided headache that awoke her from sleep. She had no episodes of trauma or abuse. She was initially able to speak, but fell into a coma within an hour. The right pupil was dilated, with slow pupillary reflexes to light on both sides, and she showed left hemiparalysis. Computed tomography scan showed a right acute epidural hematoma, approximately 4 cm in thickness, and there were no findings of trauma such as skin wounds, subcutaneous hematomas, or skull fractures. In the emergency room, decompression of intracranial pressure by one burr hole was performed, and her dilated right pupil improved to normal size. She was then moved to the operating room, and hematoma removal was performed by craniotomy. Her blood pressure trended downward despite rapid blood transfusion and vasopressor therapy. There were no abnormal findings apparent intraoperatively, except for oozing from the whole surface of the dura mater and epidural space. Her consciousness improved postoperatively, and her left hemiparalysis improved within a few days. No causative diseases, risk factors, or vascular abnormalities were found on laboratory and radiological surveys. Two months postoperatively, the bone flap was removed because of infection. Eight months postoperatively, a cranioplasty using artificial skull was performed, and her postoperative course was uneventful. One year after the initial surgery, she has no neurological deficits, and there has been no recurrence of epidural hematoma.
Intracranial acute epidural hematoma (AEDH) is mostly caused by head trauma that causes skull fractures or middle meningeal artery lacerations. Cases of intracranial AEDH without a history of trauma, called "spontaneous AEDH," have been reported. It is known that most cases of spontaneous AEDH are induced by three major causes, sickle cell disease, adjacent paranasal sinusitis, and cancer spreading to the skull or dura mater.1-11) Other minor causes of spontaneous AEDH have been vascular abnormalities, coagulopathies, autoimmune diseases, anticoagulant treatment, after heart surgery, hemodialysis, or skull bone neoplasms.12-27) However, there are three reports of intracranial spontaneous AEDH without any causative disease or abnormality, which is called "idiopathic AEDH." 14,16,21) An extremely rare case of intracranial idiopathic AEDH with initial symptoms mimicking a stroke and rapid neurological deterioration is described.
A 36-year-old woman presented with sudden onset of right-sided headache that awoke her from her sleep in the morning. Initially, she was able to talk, but she had started vomiting, and her level of consciousness deteriorated rapidly. Within only an hour, she was unconscious and was transported to our hospital. She had no past or family histories and took no medicines. Additionally, there was no medical history of anticoagulant or oral contraceptive drugs. On arrival, her Glasgow Coma Scale score was 6 (E1V1M4). The right pupil was dilated, with slow pupillary reflexes to light on both sides. She showed left hemiparalysis. Screening blood examinations did not detect any congenital coagulation defects or positive antibodies (Table 1). Computed tomography (CT) scan showed a right AEDH approximately 4 cm in thickness (Fig. 1A-C). Physical and CT findings did not show any signs of trauma, such as skin wounds, subcutaneous hematomas, or skull fractures (Fig. 1D-F). There were also no episodes of trauma or abuse from interviewing her mother and husband. Since her consciousness and respiratory status deteriorated, intratracheal intubation was performed within 24 min after her arrival. Decompression of intracranial pressure by one burr hole was then performed in the emergency room within 30 min, and her dilated right pupil improved to normal size. She was moved to the operating room at 43 min for hematoma removal by craniotomy. Her blood pressure trended downward despite rapid blood transfusion and vasopressor therapy; systolic blood pressure dropped to 50 mmHg after craniotomy, so prompt hemostasis was required. After removal of a large amount of epidural hematoma, oozing from the whole surface of the dura mater and epidural space was observed. Bleeding was stopped with hemostatic agents such as gelatin-human thrombin matrix and oxidized regenerated cellulose, bipolar coagulation, and close tenting of the dura mater to the edge of the craniotomy. Surgical operating time was 2 h and 3 min, and total hemorrhage volume was 315 mL. The hemorrhage of 218 mL was encountered at the first 30 min of the surgery, which induced rapid blood pressure reductions. The total transfusion volume was 1400 mL of concentrated red blood cells and 480 mL of fresh frozen plasma. The operation was performed under unassisted vision without an operating microscope. There were no apparent bleeding points, skull fracture, or vascular abnormalities on the dura mater on intraoperative examination.
| Reference range | ||
|---|---|---|
| CLβ2GP1: cardiolipin β2-glycoprotein 1, ANA: antinuclear antibody, RNP: ribonucleoprotein, Sm: smooth muscle, ds-DNA: double-stranded deoxyribonucleic acid, vWF: von Willebrand factor, C: complement, *: preoperative data, **: postoperative 5 days data. | ||
| PT-INR | 0.96* | |
| Fibrinogen (mg/dL) | 293* | 200–400 |
| Lupus anticoagulant | 0.9** | 0–1.2 |
| Anti-CLβ2GP1 antibody (U/mL) | <1.2** | 0–3.49 |
| Cardiolipin IgG antibody (U/mL) | <8** | 0–9.9 |
| ANA (times) | <40** | 0–39 |
| Anti-RNP antibody | Negative** | |
| Anti-Sm antibody | Negative** | |
| Anti-ds-DNA IgG antibody (IU/mL) | <10** | 0–12 |
| Anti-ds-DNA IgM antibody (U/mL) | 5** | 0–5.9 |
| vWF antigen (%) | 242** | 60–170 |
| vWF activity (U/mL) | 208** | 60–170 |
| C3 (mg/dL) | 78.4** | 73–138 |
| C4 (mg/dL) | 13.4** | 11–31 |
| Serum complement value (CH50/mL) | 34.8** | 25–58 |
| Coagulation activity factor II (%) | 102** | 75–135 |
| Coagulation activity factor V (%) | 112** | 75–135 |
| Coagulation activity factor VII (%) | 46** | 75–140 |
| Coagulation activity factor VIII (%) | 162** | 60–150 |
| Coagulation activity factor IX (%) | 144** | 70–130 |
| Coagulation activity factor X (%) | 102** | 75–130 |
| Coagulation activity factor XI (%) | 143** | 75–145 |
| Coagulation activity factor XII (%) | 41** | 50–150 |
| Coagulation activity factor XIII (%) | 44** | 70–140 |
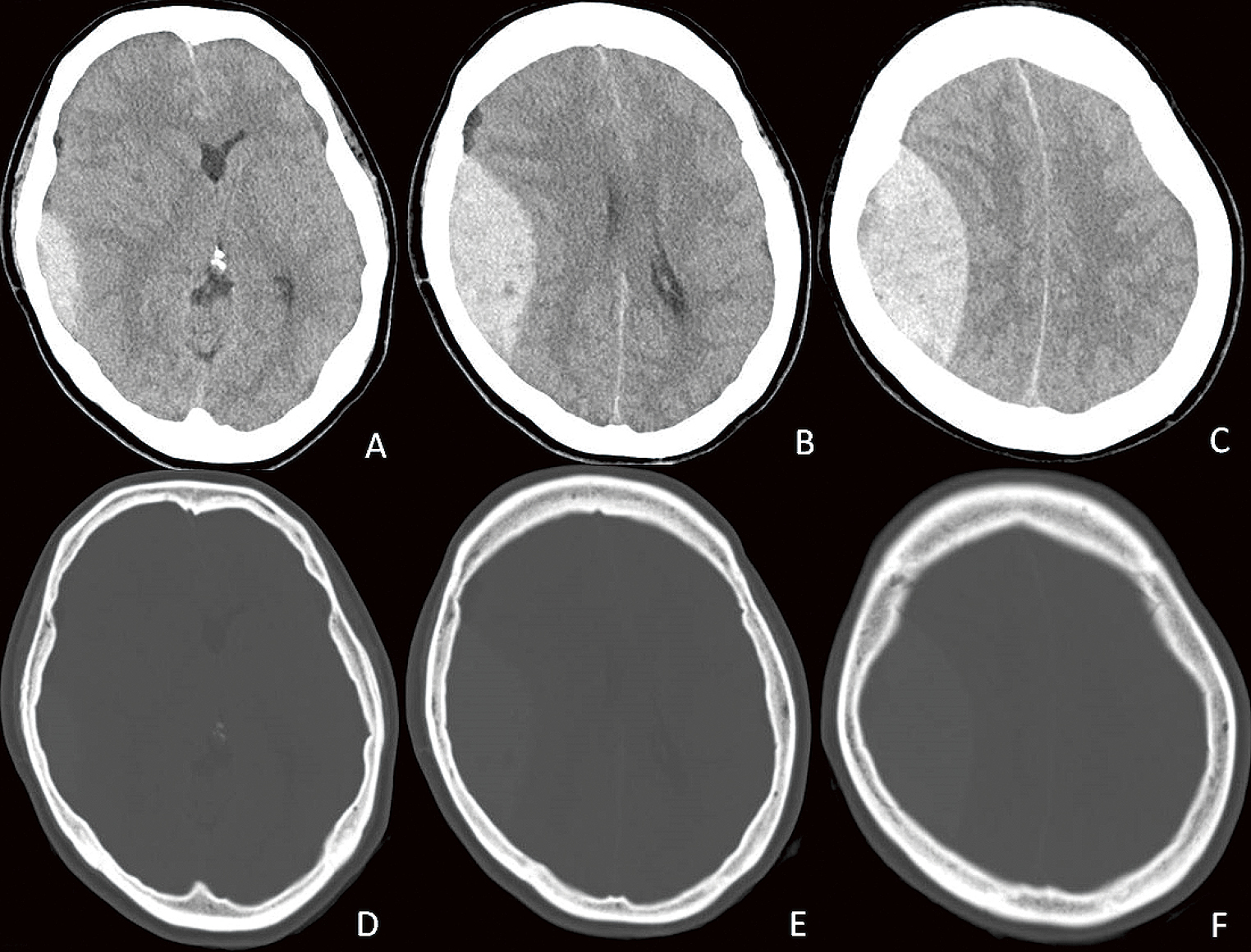
A–C) Computed tomography scan shows right acute epidural hematoma, approximately 4 cm in thickness. D–F) Computed tomography bone window setting does not show any subcutaneous hematoma or skull fracture.
Her consciousness improved postoperatively, and her left hemiparalysis also improved within a few days. CT angiography and cerebral angiography were performed postoperatively, but did not detect any abnormal vascular findings such as aneurysms, arteriovenous fistulas, arteriovenous malformations, or sinus thrombosis (Fig. 2). Magnetic resonance imaging also did not show any abnormal findings in the brain parenchyma, dura mater, or adjacent nasal sinuses (Fig. 3). Two months postoperatively, the bone flap was removed because of infection. Eight months postoperatively, a cranioplasty using artificial skull was performed, and her postoperative course was uneventful. One year after the initial surgery, she has no neurological deficits and no further recurrence of AEDH.

Right common carotid angiograms after surgery do not show any vascular abnormalities. Arterial phases (A: anteroposterior view, B: lateral view). Venous phases (C: anteroposterior view, D: lateral view).
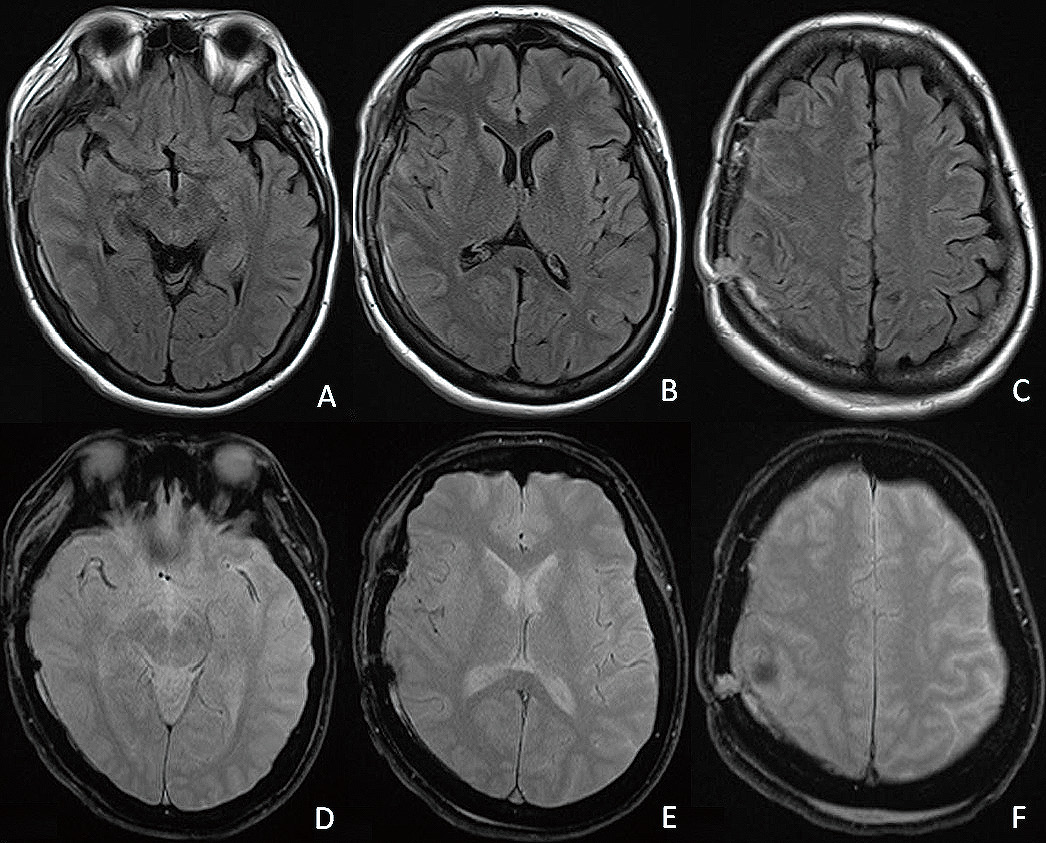
Magnetic resonance fluid-attenuated intension recovery images (A–C) and T2*-weighted images (D–F) do not show any abnormal findings in the brain parenchyma, dura mater, or adjacent nasal sinuses.
Intracranial spontaneous AEDH, a case of otological infections, was first reported in 1952 by Schneider.10) Seventy-seven cases of intracranial spontaneous AEDH have been reported so far.1-27) Intracranial spontaneous AEDHs are induced mainly by three major causes, such as sickle cell disease, adjacent sinusitis, and skull or dural metastases.1-11) The pathogenetic mechanisms of bleeding to the epidural space of the major causes are presumed to be as follows. Sickle cell disease was reported as the cause in 25 cases.3,6) It is known that sickle cell disease induces bony infarction in long bones. It also induces skull bone infarction, and recanalization of embolized vessels produces hemorrhage. A portion of infarcted skull bone is brittle, so bleeding can spread to the epidural space through the infarcted skull bone. Adjacent paranasal sinusitis was reported as the cause in 17 cases.4,8,10,11) Spreading inflammation in the paranasal sinus induces infiltration of air to the epidural space from the sinus, which causes the dura mater to detach from the skull bone. The sinusitis spreads to the meningeal artery wall through the blood vessels in the cranial diploe, and the weakened meningeal artery bleeds into the epidural space. Cancer metastases were reported as the cause in 15 cases.1,2,5,7,9) Most of them were metastases of hepatocellular carcinoma, which is a well-known risk factor of hemorrhage. When the cancer cells metastasize to not brain parenchyma, but the dura mater or skull bone, bleeding from the metastasis spreads into the epidural space.
There were other minor causes presenting with intracranial spontaneous AEDH, and they are listed in Table 2.1-27) The minor causes can be categorized into several types as follows: antithrombotic therapy type (after heart surgery,12) hemodialysis,22,23,25) rivaroxaban treatment20)), coagulation abnormality type (gastric cancer,11) hypofibrinogenemia,18) chronic liver or kidney disease21,27)), skull bone neoplasms type (solitary calvarial eosinophilic granuloma13), Langerhans cell histiocytosis,15,19) intradiploic epidermoid26)), autoimmune disease type (systemic lupus erythematosus17,24)), vascular abnormality type (berry aneurysm of the middle meningeal artery8)), and unknown type (idiopathic14,16,21)). Most cases of spontaneous AEDH induced by other minor causes needed craniotomy for hematoma removal because of their rapid and serious clinical course, and most of them achieved full recovery.
| Etiology | No. | Rates (%) |
|---|---|---|
| Major causes | ||
| Sickle cell disease | 25 | 32.5 |
| Adjacent paranasal sinusitis | 17 | 22.1 |
| Cancer metastases | 15 | 19.5 |
| Minor causes | ||
| Antithrombotic therapy type | 5 | 6.5 |
| Coagulation abnormality type | 4 | 5.2 |
| Skull bone neoplasms type | 4 | 5.2 |
| Autoimmune disease type | 2 | 2.6 |
| Vascular abnormality type | 1 | 1.3 |
| Unknown type | 4 | 5.2 |
| Total | 77 |
There have been three reported cases of intracranial "idiopathic AEDH." 14,16,21) All three cases had spontaneous AEDH, and emergency craniotomy was performed. There was no apparent risk factor on laboratory and radiological surveys. First, a 15-year-old man developed a headache that increased in severity with fever, and he fell into a coma after 4 days.16) Second, a 23-year-old woman presented with acute onset of severe headache and vomiting and a rapid decline in consciousness.21) Third, a 19-year-old woman suddenly presented with headache after hysterical crying with an AEDH.14) Two years later, she had a similar episode after crying with a new AEDH. It was postulated that hysterical crying reduced intracranial pressure and caused detachment of the dura from the skull, resulting in bleeding into the epidural space.
In the present case, AEDH was found in a patient presenting with sudden onset of a headache with a stroke-like attack. There was no evidence of any trauma, other triggers, or diseases causing easy bleeding. It was not possible to perform any examinations to detect vascular lesions before craniotomy because of the rapid clinical course. Various postoperative examinations did not detect any abnormalities of the vessels and brain parenchyma. This case had some features, such as the sudden onset of a stroke-like attack, large hematoma, and extremely rapid clinical course that indicated that the bleeding possessed high energy and the existence of some kind of vascular abnormalities supplied by arteries. Although no abnormalities around the AEDH could be detected intraoperatively, it was possible that causes of bleeding were overlooked because of the naked eye procedure. Postoperative imaging examinations did not show any lesions because of coagulation during the surgery. Some cases of intracranial idiopathic AEDH may be vascular abnormality type such as a berry aneurysm of the middle meningeal artery.8)
Intracranial idiopathic AEDH is extremely rare, and there have been only four cases reported, together with the present case.14,16,21) The clinical courses of intracranial idiopathic AEDH showed rapid deterioration. However, the deterioration was induced not by brain damage but by increasing intracranial pressure and brain compression caused by the hematoma. Therefore, prompt craniotomy and evacuation of the hematoma can achieve full recovery.
Not applicable.
The authors have no conflicts of interest directly relevant to the content of this article.