2022 年 9 巻 p. 37-41
2022 年 9 巻 p. 37-41
Stent-assisted coil embolization (SACE) is useful for treating wide-necked aneurysms. Most superior cerebellar artery (SCA) aneurysms have a wide neck, but there are few reports of SCA aneurysms treated with SACE.
One reason is that the anatomical characteristic of SCA aneurysm is not suitable for standard SACE. It is often challenging to deliver a stent to SCA via the basilar artery in an anterograde manner. In contrast, it is not difficult to deliver a stent to SCA from the anterior circulation via the posterior communicating artery. This method, in which a catheter is navigated from the anterior to the posterior circulation, is called a transcirculation technique.
We report two cases of SCA aneurysm successfully treated with SACE using transcirculation technique. This approach is helpful for wide-necked SCA aneurysms.
Aneurysms of the superior cerebellar artery (SCA) are rare, accounting for only 1% to 2% of all intracranial aneurysms,1,2) and almost all have been reported to have wide necks.3)
Although both microsurgery and endovascular treatment have shown promising outcomes for treating SCA aneurysms,4) endovascular approach has taken place of microsurgery. SCA aneurysms are difficult to treat via microsurgery because of the narrow operative field and adjacent important neurovascular structures. Conversely, developed devices and techniques have given advantages to endovascular treatment in this area.
Stent-assisted coil embolization (SACE) has been a major part of treatment for wide-necked aneurysms, but few cases of SCA aneurysm treated with SACE have been reported. One reason is that the anatomical characteristics of SCA aneurysms are not suitable for SACE. In most cases of wide-necked SCA aneurysms (dome-to-neck ratio <1.5), the angle of the SCA from the basilar artery (BA) is acute, making it difficult to deliver stents to the SCA from BA.1) We present two cases of wide-necked SCA aneurysm treated with SACE using transcirculation technique. The advantages of and notes on this technique for SCA aneurysms are discussed.
A 58-year-old woman presented to our facility after expansion of an SCA aneurysm was identified over an 8-year period. Digital subtraction angiography showed a saccular aneurysm with a diameter of 6.33 mm, a depth of 2.65 mm and a neck 4.97 mm in length (Fig. 1A). Ipsilateral to the aneurysm, the SCA-BA and SCA-posterior cerebral artery (PCA) angles, as measured from working projections of rotational angiography with three-dimensional (3D) image reconstruction, were 5° and 145°, respectively (Fig. 1B and Table 1). Alcock's test showed the diameters of the posterior communicating artery (PCoA) and P1 were 1.18 and 2.98 mm, respectively.
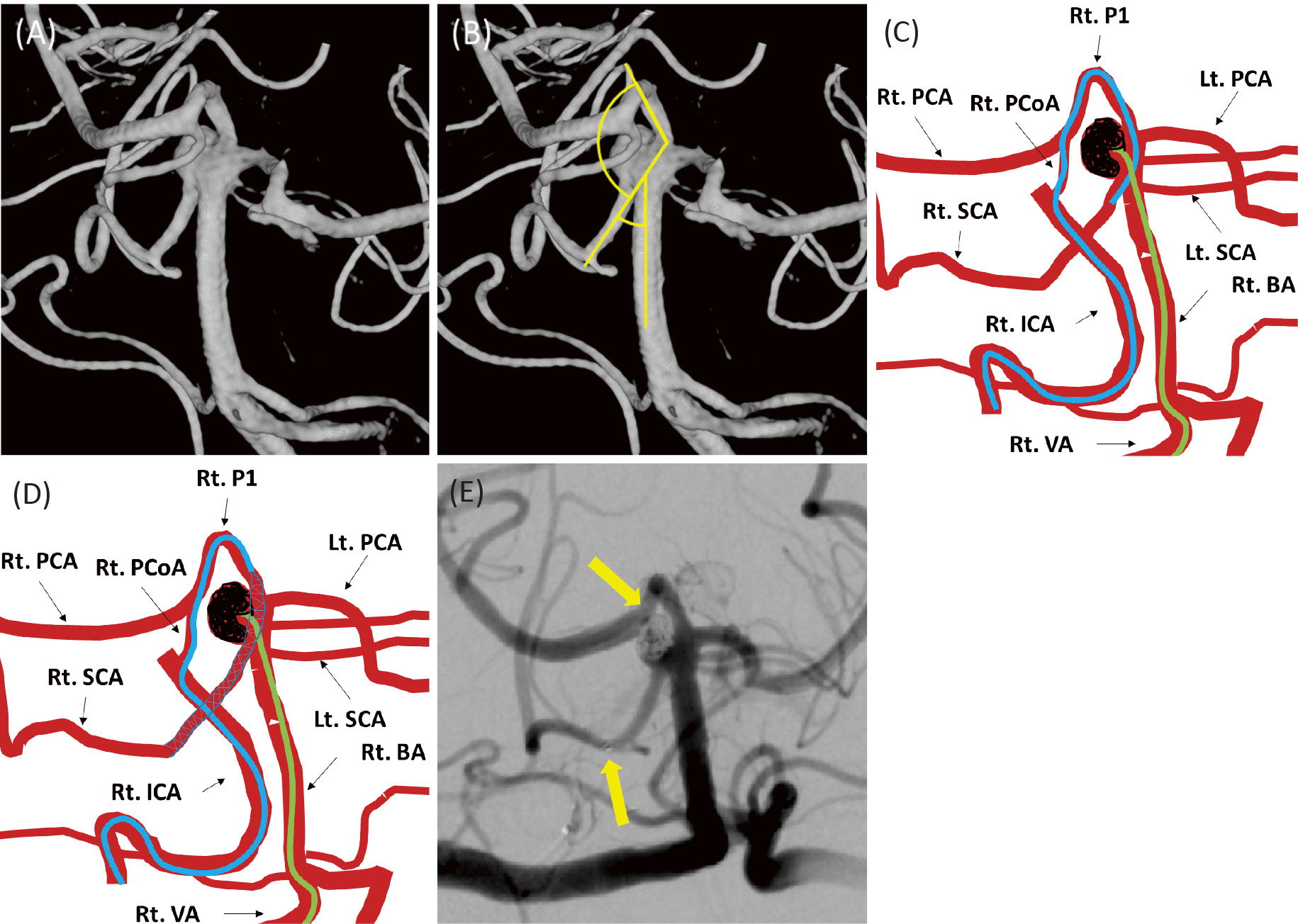
(A) The three-dimensional rotational angiography shows a wide neck aneurysm of the right SCA. (B) The angle of the right SCA/PCA was wide, and the angle of the right SCA/BA was acute. (C) An Excelsior SL-10 microcatheter (Stryker, Kalamazoo, MI, USA) was derived to the right SCA via the right PCoA and the right P1. Coils were embolized using another microcatheter delivered from the right VA. (D) After the aneurysm was embolized, a Neuroform Atlas stent 3*21 (Stryker) was derived by the Excelsior SL-10 covering the neck of the aneurysm. (E) The angiography just after the intervention shows that the Raymond–Roy occlusion classification is class IIIa. The stent was positioned from the right SCA to the right P1 just proximal to the right PCoA (arrows).
BA, basilar artery; Lt. PCA, left posterior cerebral artery; Lt. SCA, left superior cerebellar artery; Rt. ICA, right intracervical artery; Rt. PCA, right cerebral artery; Rt. P1, right P1 segment of PCA; Rt. PCoA, right posterior communicating artery; Rt. SCA, right superior cerebellar artery.
| Case | Vessel diameter (mm) | SCA–BA angle (°) | SCA–PCA angle (°) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| SCA | P1 | PCoA | Contralateral | Ipsilateral | Contralateral | Ipsilateral | ||||
| BA, basilar artery; PCoA, posterior communicating artery; P1, P1 segment of the posterior cerebral artery; SCA, superior cerebellar artery. | ||||||||||
| 1 | 1.65 | 2.98 | 1.18 | 80 | 5 | 0 | 145 | |||
| 2 | 1.48 | 1.82 | 1.04 | 55 | 30 | 30 | 150 | |||
Prior to intervention, the patient was neurologically intact. She was administered clopidogrel at 75 mg/day and aspirin at 100 mg/day for 1 month preceding the intervention. Platelet aggregation testing confirmed a slightly insufficient response to clopidogrel. Cilostazol at 100 mg/day was thus administered for 1 day before the intervention.
Technical procedureGeneral anesthesia was induced. Guiding catheters were positioned at the cervical portion of the right internal carotid artery (ICA) and at the right vertebral artery (VA). An Excelsior SL-10 microcatheter (Stryker, Kalamazoo, MI, USA) was navigated to the right SCA covering the neck of the aneurysm via the right ICA, right PCoA, and right P1 segment of PCA along a microguidewire (Fig. 1C). Another microcatheter was introduced to the right SCA aneurysm from the right VA, with six coils filled into the aneurysm. After embolization, we placed a Neuroform Atlas stent 3*21 (Stryker) from the right SCA to the right P1 via the Excelsior SL-10 microcatheter (Fig. 1D). The final angiographic run demonstrated almost complete embolization of the aneurysm. The Raymond-Roy occlusion classification was class IIIa (Fig. 1E). After the intervention, the patient was free from neurological abnormality.
She was subsequently discharged home on postintervention day 5 with a modified Rankin Scale (mRS) score of 0. Clopidogrel and aspirin were continued for 6 months. No thrombotic complications were detected during the clinical course. Six months after the intervention, digital subtraction angiography demonstrated moderate coil compaction but no stenosis of the stent. The Raymond-Roy occlusion classification at this point was class IIIa.
A 75-year-old woman presented to our facility with subarachnoid hemorrhage (Hunt and Kosnik grade 3) due to rupture of a BA-SCA aneurysm. The aneurysm had a wide neck and a bleb with a neck length of 5.09 mm, diameter of 3.71 mm, and depth of 2.98 mm (Fig. 2A). Diameters of the PCoA and P1 were 1.04 and 1.82 mm, respectively (Table 1). SCA-BA and SCA-P1 angles, as measured from working projections of rotational angiography with 3D image reconstruction, were 30° and 150°, respectively (Fig. 2B and Table 1). In the acute phase, we embolized only the bleb of the aneurysm, holding off on complete embolization of the dome. After the first intervention, she was administered clopidogrel at 75 mg/day and aspirin at 100 mg/day for 1 month. One month later, in the subacute phase, complete embolization of the aneurysm was performed.
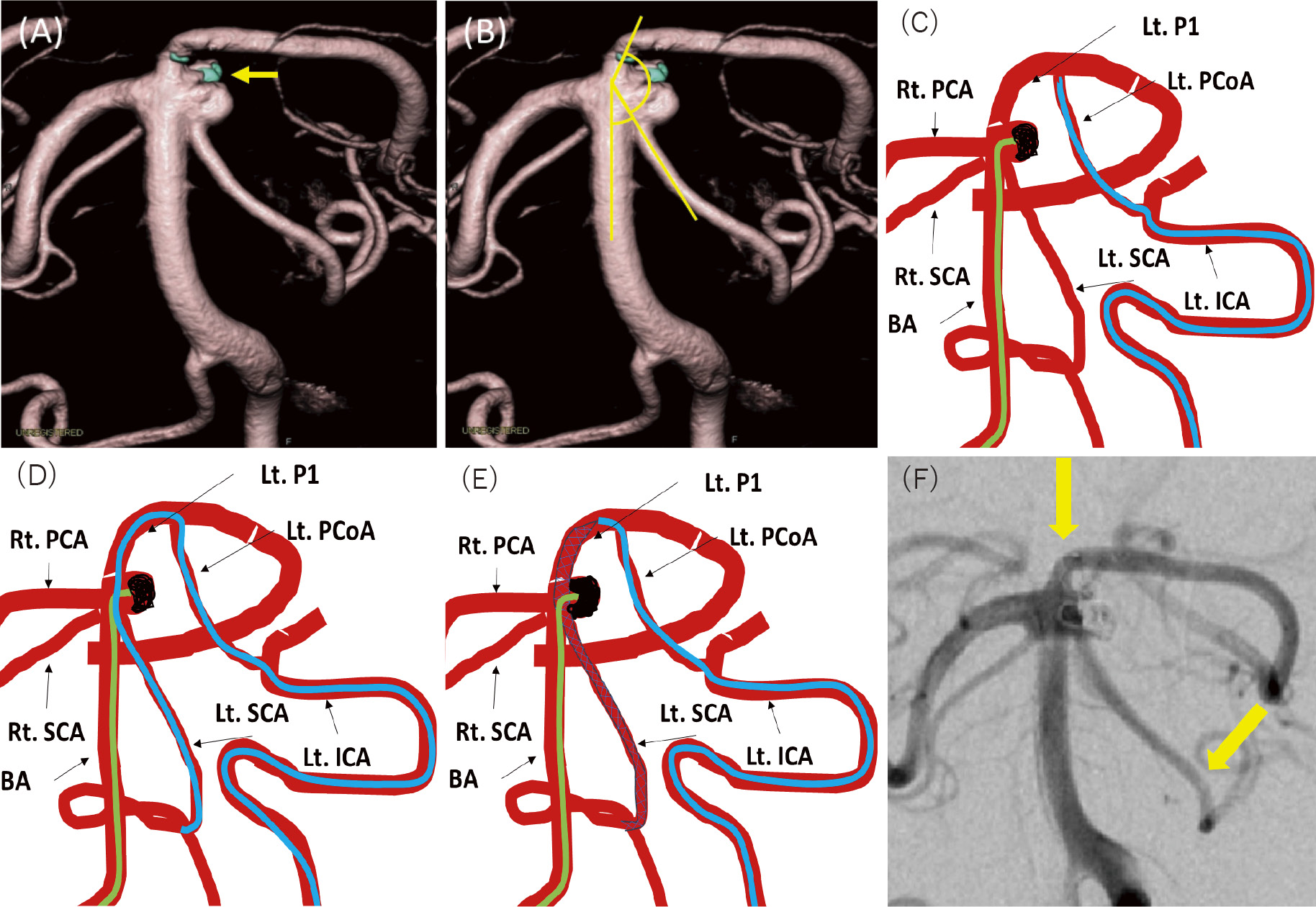
(A) The three-dimensional rotational angiography shows a wide neck aneurysm of the left SCA. The bleb was embolized in the first treatment after subarachnoid hemorrhage (arrow). (B) The angle of the left SCA/PCA was wide, and the angle of the left SCA/BA was acute. (C) An Excelsior SL-10 microcatheter was placed at the left PCoA adjacent the PCoA. Two framing coils were embolized using another microcatheter delivered from the right VA. (D) The Excelsior SL-10 microcatheter derived to the SCA. (E) A Neuroform Atlas stent 3*21 (Stryker) was placed covering the neck of the aneurysms; then finishing coils were embolized. (F) The angiography just after the intervention shows that Raymond–Roy occlusion classification is class IIIa. The stent was placed from the left SCA to the left P1 just proximal to the junction with the PCoA (arrows).
BA, basilar artery; Lt. ICA, left intracervical artery; Lt. PCoA, left posterior communicating artery; Lt. P1, left P1 segment of PCA; Lt. SCA, left superior cerebellar artery; Rt. PCA, right posterior cerebral artery; Rt. SCA, right superior cerebellar artery.
After general anesthesia was induced, we inserted and positioned guiding catheters in the cervical portion of the left ICA and right VA. An Excelsior SL-10 microcatheter was navigated to the left PCoA adjacent to the left P1 segment of PCA. Another microcatheter was delivered to the aneurysm from the right VA along a microguidewire, and two framing coils were embolized (Fig. 2C). An Excelsior SL-10 was delivered to the left SCA (Fig. 2D), and a Neuroform Atlas stent 3*21 (Stryker) was placed from the left SCA to the left PCoA. Then, two finishing coils were embolized (Fig. 2E). The Raymond-Roy occlusion classification was class IIIa (Fig. 2F). After the intervention, neurological examination demonstrated no deficits. The patient was discharged home on postintervention day 4 with an mRS score of 0. Platelet aggregation testing demonstrated excess response to clopidogrel, so the dose was reduced to 25 mg/day. A regimen of clopidogrel at 25 mg/day and aspirin at 100 mg/day was continued for 6 months.
SACE is known to be effective for wide-necked aneurysms. Howard et al. reported that 12.2% of intracranial aneurysms were treated with SACE.5) They also reported that the recurrence rate was significantly better in the SACE group (9.5%) than in the non-SACE group (11.3%; p = 0.003).
Many SCA aneurysms are wide necked. Chan et al. reported that as many as 88.6% of all SCA aneurysms are wide-necked type in a single-center retrospective case series.3) However, not many SCA aneurysms are treated with SACE. The reason may be due to the anatomical characteristics of an SCA aneurysm. Chan et al. stated that SCA aneurysms are unsuitable for SACE because the angle between the BA and SCA ipsilateral to the aneurysm tends to be acute.3) An acute SCA-BA angle makes it difficult to direct a wire and catheter to the SCA from the BA in an anterograde manner. Conversely, directing devices to the SCA via the PCoA is not difficult because the SCA-P1 angle tends to be obtuse. Further, stents delivered via the PCA could effectively cover the necks of the target aneurysms. In our case, the anatomical characteristics corresponded to Chan's report (Table 1), and the stent was delivered to SCA via PCA and effectively covered the necks of the aneurysms.
This method, in which a catheter is navigated from the anterior to the posterior circulation, is called a transcirculation technique.6) Thanks to developments of devices and techniques in the endovascular field, the number of the reports of SACE using transcirculation technique has increased since end of 2000 decades. According to recent literatures, basilar tip and SCA aneurysms were treated SACE via PCoA.7-9) Basilar tip aneurysms, which are most frequently reported, were treated with SACE using transcirculation technique with the stents navigated P1 to P1 via PCoA.
We can find two reports of SCA aneurysm treated with SACE using transcirculation technique.7,8) Felipe et al. achieved successful outcomes in a case of SCA aneurysm by placing a stent from the PCoA opposite the aneurysm to the SCA.7) Ahmed et al. treated an SCA aneurysm delivering a stent to the SCA from the PCoA on the aneurysm side.8) In our cases, we introduced stents to the SCA from the PCoA ipsilateral to the aneurysm.
In the procedure of transcirculation technique, the PCoA on either side can be chosen for the passage of stents depending on which is better for the stent intended to cover the neck of the aneurysm or which is larger. In treating an SCA aneurysm with SACE using the transcirculation technique, the diameters of the PCoA and P1 need to be considered when determining the approach route of the stents. When the diameters of the PCoA and P1 are larger than 1 mm, a 1.7-Fr microcatheter such as the Excelsior SL-10 can be navigated safely for delivering a Neuroform Atlas.
We successfully performed SACE using the transcirculation technique for two cases of wide-necked SCA aneurysm with acute SCA-BA angles. Good angiographic outcomes were achieved, and no thrombotic complications were encountered. We think SACE using the Neuroform Atlas with the transcirculation technique is useful for treating wide-necked aneurysms of the SCA.
The authors received no financial support.