2022 年 9 巻 p. 183-186
2022 年 9 巻 p. 183-186
Aneurysms of the A1 segment of the anterior cerebral artery tend to develop in combination with various vascular anomalies of the A1 segment. Arterial branches that originate from the A1 segment and perfuse cortical regions are known to be rare. In this report, we describe a 48-year-old woman who presented with a ruptured aneurysm at the origin of an anomalous cortical artery arising from the A1 segment, for which microsurgical neck clipping was performed. Intraoperatively, the anomalous artery was seen to originate from the A1 segment, running into the interhemispheric fissure. An aneurysm was located at the bifurcation of the anomalous artery and the A1 segment. Postoperative angiography showed that the anomalous artery has branched into the fronto-orbital artery and the frontopolar artery and terminated as the anterior internal frontal arteries. We report a rare case of an aneurysm arising from an anomalous callosomarginal artery that arose from the A1 segment and perfused the cortical region. It is of significance to recognize that an aneurysm can develop at the origin of an anomalous artery that arises from the A1 segment.
Aneurysms of the anterior cerebral artery (ACA) are usually detected in the anterior communicating artery or the distal portion of the ACA. Aneurysms of the A1 segment are deemed relatively rare, accounting for 0.88-2.1% of all cerebral aneurysms.1-5) The most common site of the A1 segment aneurysms is the origin of the perforating arteries, accounting for 55.6-88.9% of such aneurysms.2-4) A1 segment aneurysms also tend to be associated with other anomalies, such as fenestration, accessory middle cerebral artery, and azygous ACA.3,4,6,7) Arterial branches that originate from the A1 segment and perfuse cortical regions are rare.6,8-10) Further, origin of the callosomarginal artery (CMA) from the A1 segment has only been rarely reported.11,12)
Herein, we report a case of a patient who had a ruptured aneurysm at the origin of an anomalous CMA arising from the A1 segment of the ACA.
A 48-year-old woman presented with sudden headache. Computed tomography (CT) revealed subarachnoid hemorrhage (SAH) in the basal cistern (Fig. 1). Three-dimensional CT angiography has demonstrated an aneurysm with a major diameter of 2.8 mm, which was located at the bifurcation where the anomalous artery, running along with the left pericallosal artery, originated from the A1 segment of the left ACA (Fig. 2A). The diameter of the left pericallosal artery was noted to be smaller than that of the contralateral pericallosal artery (Fig. 2B). The patient underwent left frontotemporal craniotomy under general anesthesia. Intraoperatively, an aneurysm was confirmed at the bifurcation where the anomalous artery, running toward the interhemispheric fissure, arose from the A1 segment. The aneurysm projected downward and was attached to the left optic nerve (Fig. 3). During aneurysm clipping, absence of perforating arteries originating from the arterial wall around the aneurysm was confirmed.
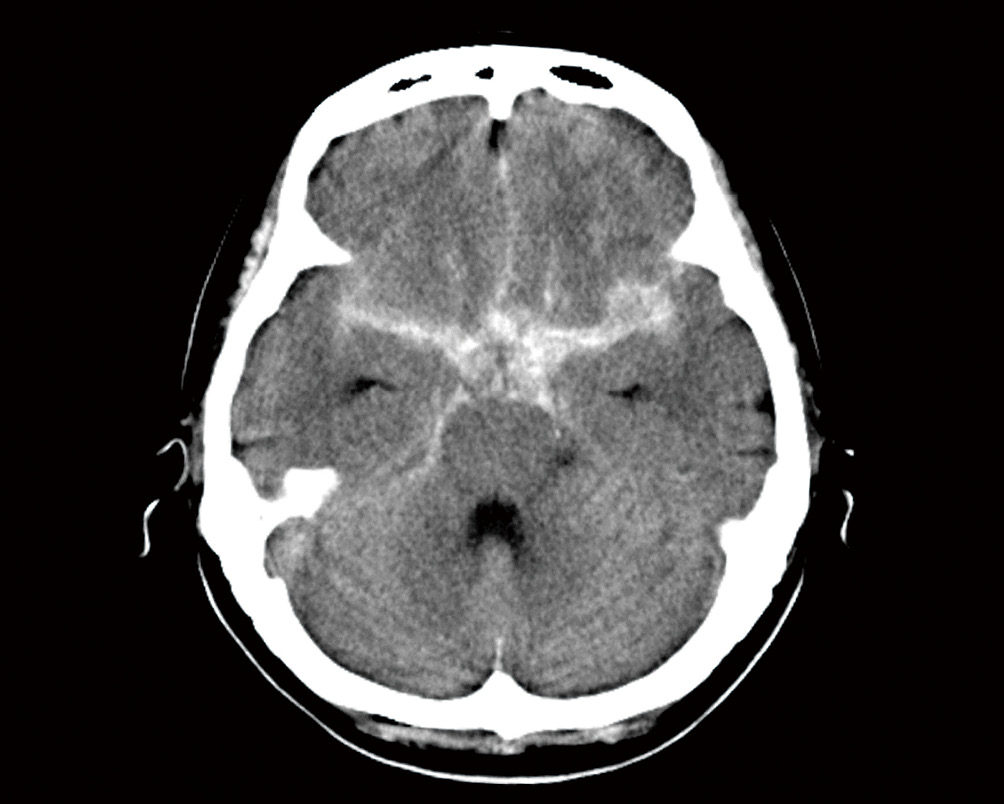
CT scan demonstrating subarachnoid hemorrhage in the basal cistern, predominantly on the left side.
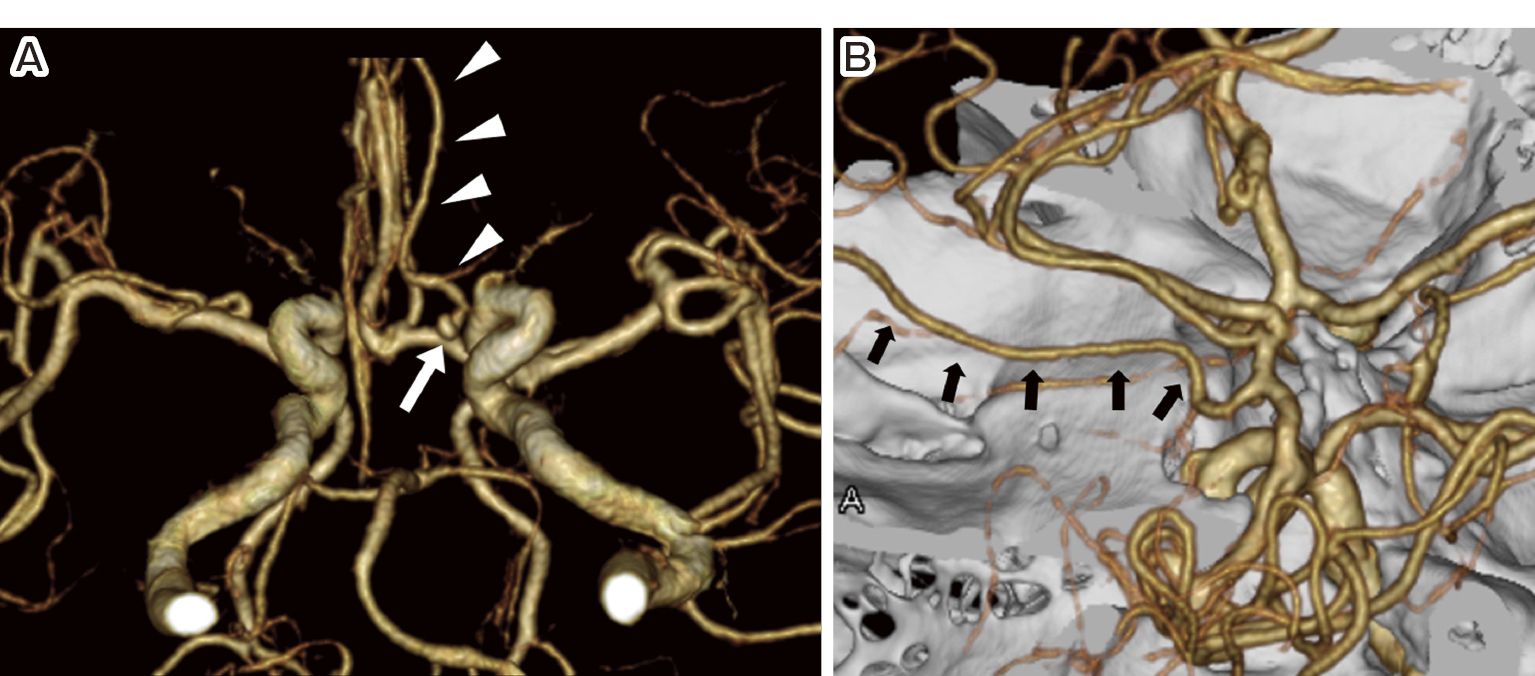
Three-dimensional CT angiograms showing an aneurysm (white arrow) located at the bifurcation of the A1 segment of the left anterior cerebral artery (ACA) and the anomalous artery originating from the A1 segment (white arrowhead) (A, inferior view). The anomalous artery has coursed toward the interhemispheric fissure (arrows) (B, lateral oblique view). The diameter of the anomalous artery was similar to that of the left pericallosal artery.
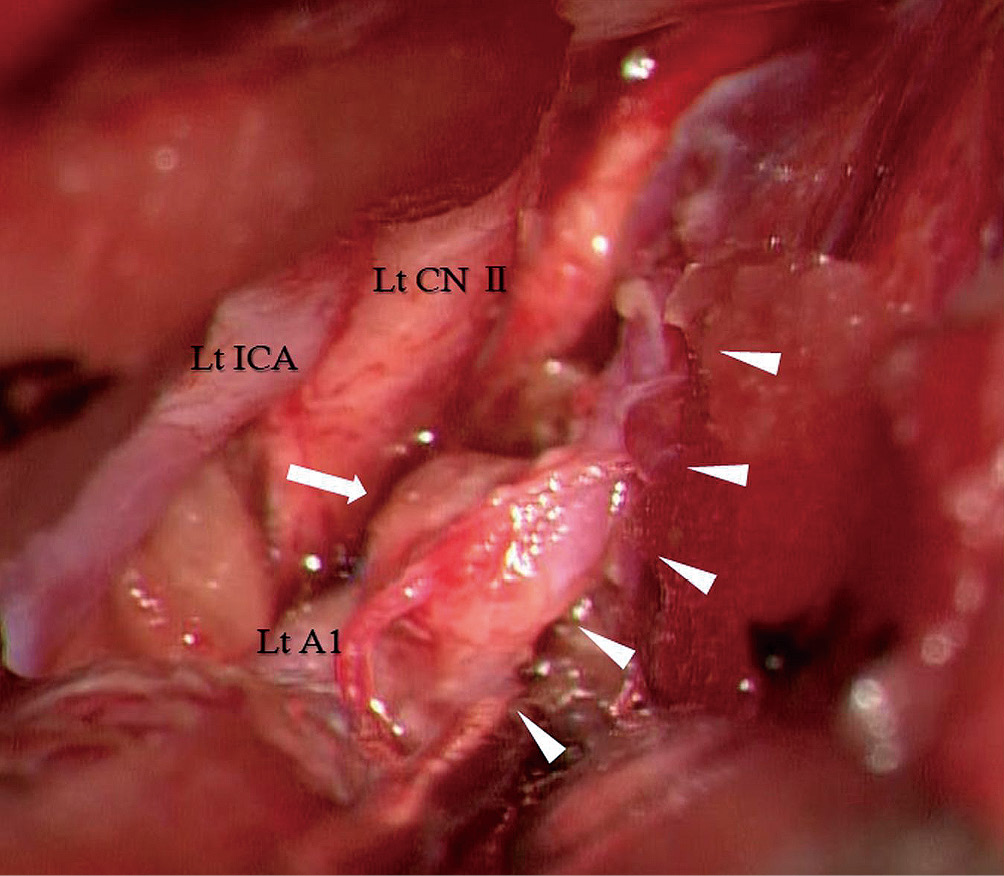
Intraoperative photograph showing an aneurysm located at the bifurcation of the left A1 segment of the anterior cerebral artery (white arrow) and the anomalous artery running toward the interhemispheric fissure (white arrowhead). The aneurysm projected downward and was attached to the left optic nerve.
Postoperative CT angiography confirmed resolution of the aneurysm. Angiography via arterial catheterization demonstrated that the anomalous artery branched into the frontopolar artery and the fronto-orbital artery and terminated as the anterior internal frontal arteries (Fig. 4). The patient's postoperative course was deemed uneventful.

Lateral view of the left common carotid artery angiogram showing that the anomalous artery originated from the A1 segment, ran parallel to the ipsilateral pericallosal artery, branched into the front-orbital artery (black dotted arrows) and the frontopolar artery (black arrow), and terminated as the anterior internal frontal arteries (white arrow).
The CMA courses in or near the cingulate sulcus, runs parallel to the pericallosal artery, and gives rise to two or more cortical branches.13,14) The artery in this present case was observed to be consistent with the above characteristics of the CMA, and the usual CMA originating from the A2, A3, or A4 segments of the ACA was absent. Thus, this present case was considered to have an anomalous CMA arising from the A1 segment of the ACA. This type of anomalous CMA has only rarely been reported.11,12) Development of the ACA generally begins at around 30 days of embryonic life.15) During the next 20 days, the ACA courses upward between the bilateral expanding cerebral hemispheres, followed by the development of cortical arteries.15) In this present case, the CMA might not have developed normally from the A3 segment for unknown reasons, resulting in the development of the anomalous CMA arising from the A1 segment.
A variant similar to that seen in the present case is the type 3 artery of the persistent primitive olfactory artery (PPOA). The type 3 artery of the PPOA arises from the A1 segment of the ACA and supplies the territory of the distal ACA, as it runs along the olfactory tract and makes a unique hairpin bend.16,17) This present case also had the former two features, although the latter two features differed from the anomaly in this present case.
A previous investigator reported a patient with intracranial hemorrhage due to a ruptured anteriorly directed aneurysm that formed at the origin of an anomalous CMA arising from the A1 segment.11) Our patient, however, suffered SAH due to a ruptured downward-facing aneurysm that formed at the origin of the anomalous CMA. Development of aneurysms in such locations has been reportedly associated with local hemodynamic stress2,3,10-12) and weakness of the arterial wall.12)
Saccular aneurysms of the A1 segment are divided into the following three types according to their site of occurrence: type 1, at the origin of a perforator arising from the A1 segment; type 2, proximal to the A1 fenestration; and type 3, at the end of the hairpin-curved A1 segment without branching arteries (with the A1 segment showing marked elongation and kinking).3) Aneurysms occurring at the bifurcation of a cortical artery arising from the A1 segment have not been classified, indicating that this type of aneurysm is rare.3)
Perforating arteries usually arise from the superior and/or posterior aspect of the A1 segment and run directly to the anterior perforating substance.18) Type 1 aneurysms typically project superiorly and/or posteriorly. Therefore, when type 1 aneurysms are clipped, separation of the perforating arteries from the neck or dome of the aneurysm is required.5,7) In contrast, when the aneurysm anatomically projects downward, as in this present case, it might be unrelated to the origin or course of the perforating arteries; hence, easy clipping of the aneurysm can be performed.
The author would like to thank the patient and her family for their cooperation.
The author declares no conflict of interest.