2022 Volume 9 Pages 365-369
2022 Volume 9 Pages 365-369
Syringomyelia is often associated with Chiari malformation, trauma, infection, and spinal cord tumor. Although they are relatively rare diseases, arachnoid cysts and its related pathology, "arachnoid web" can sometimes lead to syrinx formation at the thoracic vertebral level. However, syrinx formation caused by degenerative spinal disorders, particularly at the thoracic vertebral levels, has rarely been reported. Herein, we present a case of syringomyelia with thoracic ossified yellow ligament (OYL) in a 79-year-old man, who underwent initial posterior decompression followed by arachnoid web removal. Posterior decompression via laminectomy of thoracic vertebra 2 and removal of the OYL improved the syrinx partially, but dorsal indentation of the spinal cord and a remnant syrinx were observed in post-operative magnetic resonance images, subsequent to the second surgery's successful removal of the arachnoid web, which had dorsally compressed the spinal cord. After the second operation, the syrinx shrunk further, and the patient could walk independently at 5 months after the operations. In our case, both the OYL and arachnoid web were responsible for syrinx formation. Therefore, the coincidence of degenerative vertebral diseases with a syrinx might indicate the coexistence of an underlying lesion. Furthermore, the arachnoid web in this case might have formed due to the denaturation of the arachnoid cyst triggered by the OYL.
Syringomyelia is usually caused by the obstruction of cerebrospinal fluid (CSF) in the subarachnoid space owing to conditions including Chiari malformation, arachnoiditis, or spinal tumor. However, syringomyelias are rarely associated with degenerative spinal diseases, particularly those at the thoracic vertebral levels.1) Nevertheless, arachnoid cysts occurring in the thoracic vertebrae have been reported to lead to syringomyelia.2) Recently, the "arachnoid web" has been linked to arachnoid cysts, which could also cause syringomyelia at the thoracic vertebral levels. The arachnoid web was first reported in the 1970s.3) It is a membranous tissue, also called the "dorsal thoracic arachnoid web" due to its presence in the dorsal spinal cord, and can be identified by its radiological characteristic known as the "scalpel sign." 4) The precise etiology and pathogenesis of arachnoid webs remain unknown. However, considering their histological and positional similarity to arachnoid cysts, it has been suggested that they are remnants of collapsed or degenerated arachnoid cysts.5)
Herein, we report a case of syringomyelia associated with both arachnoid web formation and ossification of the yellow ligament (OYL).
A 79-year-old man was presented to our hospital with a 4-year history of gait disturbance. While his symptoms gradually worsened and he visited the Neurosurgery department of the previous hospital, where magnetic resonance imaging (MRI) revealed a cystic lesion in the spinal cord at the cervicothoracic junction level, his earlier visits to the neurology departments of other hospitals or treatments at rehabilitation hospitals had not led to an accurate diagnosis.
On admission to our department, he manifested the gait disturbance, which was caused by the impairment of deep sensation in both lower limbs. Superficial sensation and muscular tonus were normal, and no paralysis or neuropathic pain was observed. MR (magnetic resonance) images (Fig. 1A) and Computed tomography (Fig. 1B) at the cervical (C) and thoracic (Th) vertebral levels showed that an ossification of the yellow ligament (OYL) had severely compressed the spinal cord in the dorsal direction (Fig. 1B-D). Furthermore, the images revealed that a syringomyelia had developed at the C7-Th1 level (Fig. 1A, E), on the cranial side of the OYL. Therefore, we considered that the OYL was the main symptomatic lesion and that the syringomyelia might have been caused by spinal canal stenosis. Posterior decompression was performed by laminectomy of Th2, and the OYL lesion was removed (Fig. 2A, B). Intraoperative ultrasonography demonstrated a pulsatile spinal cord; therefore, decompression of the spinal cord was considered fully achieved, and the dura matter was not opened to confirm the subdural lesion. Post-surgery, his gait improved slightly, but unstable gait and impairment of deep sensation in the lower limbs remained. Postoperative MR images showed that the syrinx had reduced in size, and the dural sac was not compressed by the OYL. However, although the cyst-like membranous lesion had cleared, it continued to compress the spinal cord dorsally, resulting in the indentation of the spinal cord that resembled a "scalpel sign" (Fig. 2C). We considered that this membranous lesion was associated with the remaining syrinx, and a second operation was performed to remove this membranous lesion 11 days after the first operation. A tough membranous structure, which had adhered to the arachnoid membrane, was observed in the dorsal spinal cord after the dural opening (Fig. 3A). After removal of the membranous lesion, the compression of the spinal cord was fully relieved (Fig. 3B). Pathological examination of the membranous lesion identified epithelial tissue without a tumor or infectious lesion, which was consistent with an arachnoid cyst (Fig. 3C, D). We concluded that the lesion was an arachnoid web based on the characteristic findings in the MR images and pathological examination. After the second surgery, the syrinx shrunk further (Fig. 4). Within 5 months after the first surgery, the patient could walk independently and stably, with his symptoms improved. MRI at 1 year after the operation confirmed no recurrence of the syrinx.
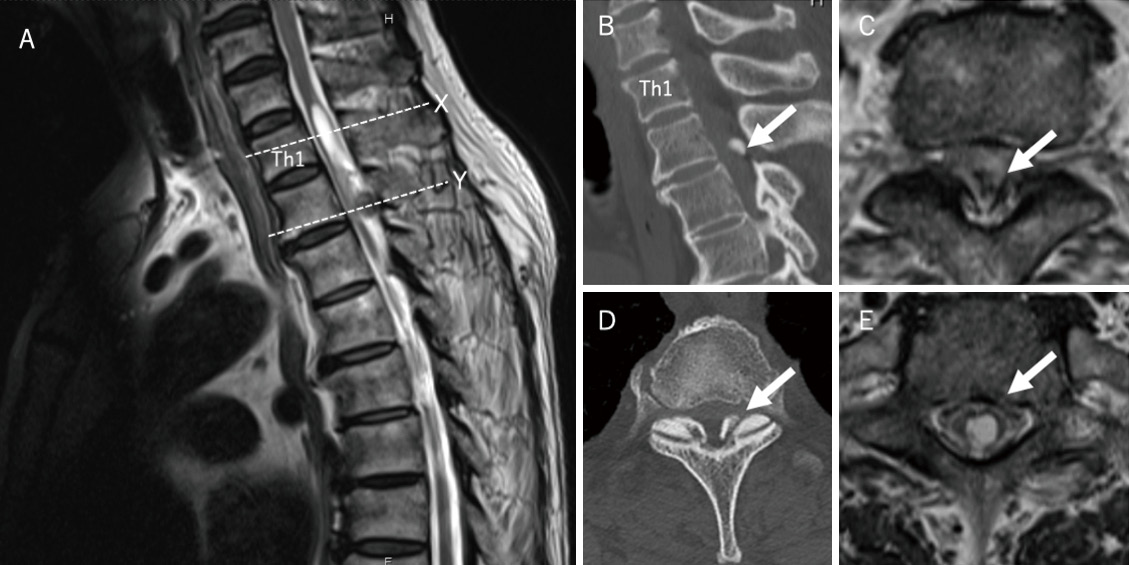
(A) Preoperative T2-weighted MRI sagittal image demonstrated posterior compression of the spinal cord by the OYL at Th2/3. Syringomyelia was observed at C7/Th1. The dotted lines X and Y indicate the location of the axial slices in (E) and (C), respectively.
(B) (C) The OYL (arrow) at Th2/3 compressed the spinal cord, causing severe spinal canal stenosis.
(D) CT image showed the OYL (arrow) at Th2/3.
(E) An intramedullary syrinx (arrow) was formed.
MRI: magnetic resonance imaging, OYL: ossification of the yellow ligament, Th: thoracic, C: cervical, CT: computed tomography
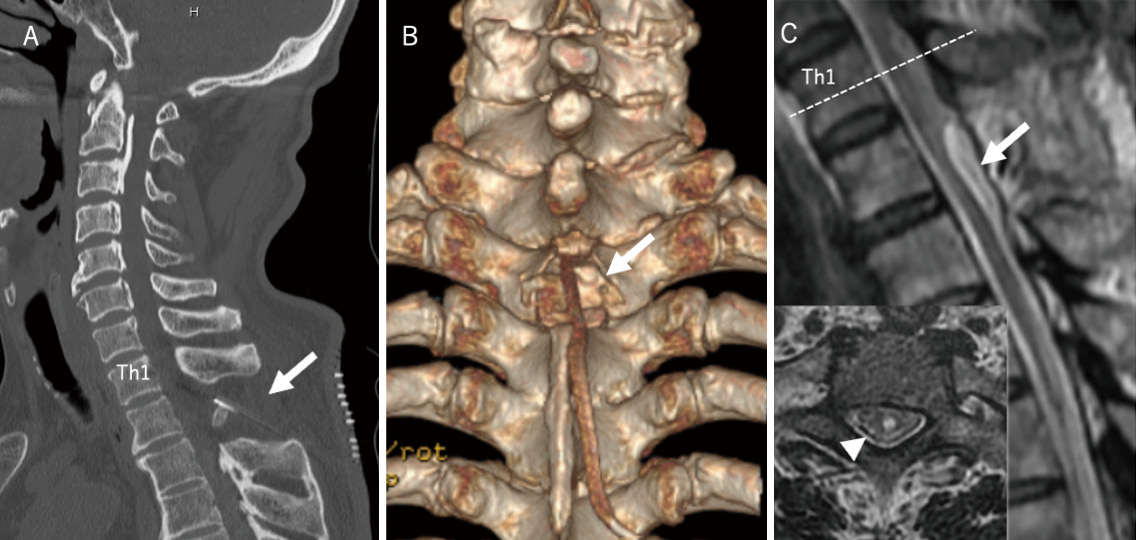
(A) (B) CT image and its three-dimensional reconstructed image after the first operation. The Th2 lamina was opened, and the OYL was resected. Laminectomy was performed at Th2 (arrow).
(C) T2-weighted MRI sagittal image showed a scalpel-like deformity in the spinal cord at the Th2/3 level. This “scalpel sign” is the radiological feature of arachnoid web. The dotted line shows the level of the axial image. A residual syringomyelia (arrowhead) was noted.
CT: computed tomography, Th: thoracic, OYL: ossification of the yellow ligament, MRI: magnetic resonance imaging

(A) Intraoperative microscopic image showed a tough, non-cystic, membranous tissue passing transversely and compressing the dorsal spinal cord. The membranous tissue was adhered to the intact arachnoid membrane in the upper and lower spinal cord regions. The asterisk indicates the cranial side.
(B) Intraoperative microscopic image after total resection of the arachnoid web.
(C) (D) Pathological examination of the resected arachnoid web revealed a tough membranous tissue with arachnoid-like epithelium.
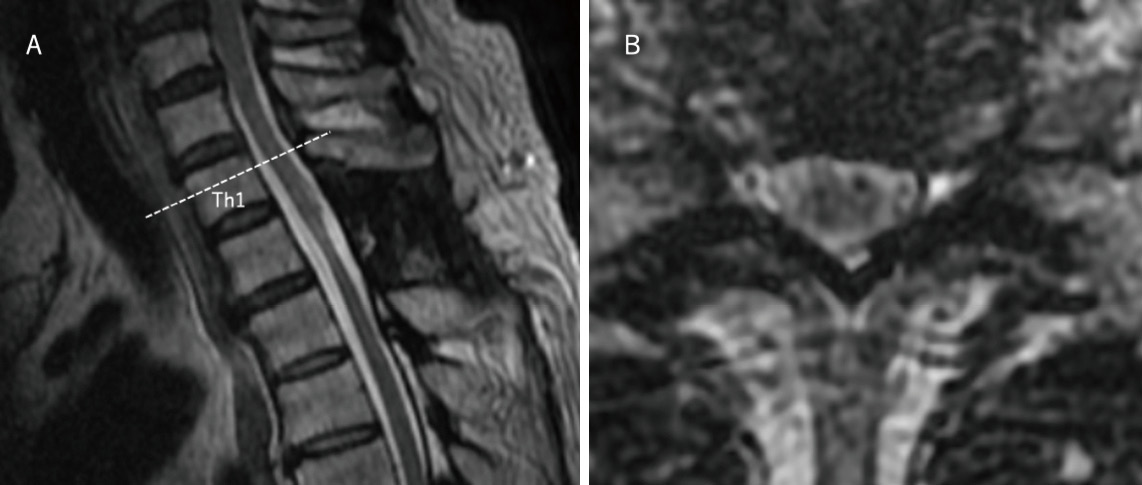
(A) T2-weighted MRI sagittal image acquired at 1 year after operation. Syrinx was remarkably shrunken. The dotted line indicates the location of the axial slice in (B).
(B) T2-weighted MRI axial image obtained at 1 year after operation.
MRI: magnetic resonance imaging
We report the successful treatment of a case of syringomyelia associated with thoracic OYL and arachnoid web formation. To the best of our knowledge, only two cases of syringomyelia complicated with thoracic OYL have been reported.6,7) OYL is a prevalent disease, with an incidence of 36% in Japanese populations8) and 63.9% in Chinese populations.9) Therefore, considering the high prevalence of OYL, the possibility of syringomyelia accompanied by OYL is very rare. Although the exact pathogenic mechanism of syringomyelia remains unknown, it is often associated with CSF dynamics around the spinal cord. According to the recently advocated "pulse pressure theory," the increase in the pulse pressure of the spinal cord relative to the surrounding subarachnoid space and repetitive mechanical distention cause the accumulation of extracellular fluid in the spinal cord, resulting in a syrinx.10) Consequently, supporting the notion that degenerative spinal diseases are rarely associated with syringomyelia, the relative increase in pulse pressure may be associated with CSF obstruction, which is principally not associated with vertebral degenerative disease involving the epidural compression of the spinal cord. Furthermore, in addition to epidural compression, the coexisting denaturation of the arachnoid membrane could lead to obstruction of the CSF, resulting in a syrinx.
Adhesive changes in the arachnoid membrane of the spinal cord have been described in a syringomyelia case associated with OYL.7) In this case, the simple mechanical compression by the OYL alone would not have caused the syringomyelia. Moreover, the membranous tissue formed at the same vertebral level as that of the OYL might have been the main cause of CSF obstruction. Additionally, although the removal of the OYL in the first operation only shrunk the syrinx, the OYL might have partially contributed to the disturbance of the CSF dynamics. Moreover, syrinx was occurred on the cranial side of the stenosis in this case. The side where syrinx occurred was, according to the pulse pressure theory, determined by the degree of the intramedullary pulse pressure transmission.10) Resulting in the syrinx development on the cranial side of it, OYL might constrict the spinal cord and prevent the pulse pressure transmission, as is seen in this case.
Pathological examination of the membranous tissue excised in the second operation revealed a tough membranous but noncystic appearance. While there is no pathological definition of the arachnoid web, the arachnoid membrane-like epithelial tissue observed in our specimen was consistent with that previously described.11)
In the arachnoid web diagnosis, the important finding of "scalpel sign" was found on the MR images, which indicated the dorsal indentation of the spinal cord. Thus, our case corresponded to the entity of the arachnoid web. Most of the reported cases of arachnoid web have occurred in the upper thoracic levels, where 100% of them were formed in the thoracic vertebral levels, among which 92% of them were located on the dorsal side.12) A total of 67% of them were complicated with syringomyelia. Furthermore, while most of cases were caused by an unknown pathology, some cases were due to trauma and previous surgery.
In this study, there was no previous history of trauma or pathology that may have caused the arachnoid web. Severe compression by the OYL was observed in the same location as that of the arachnoid web; thus, chronic mechanical stimulation by the OYL was considered to be involved in the development of the arachnoid web. Considering that arachnoid cysts of the spinal cord preferentially occur at the thoracic level.2) We speculate that the pre-existing arachnoid cyst was denatured and collapsed owing to chronic compression, which progressed gradually with aging to form the arachnoid web which in turn caused the syringomyelia through CSF obstruction.
Initially, although the arachnoid web in the dorsal spinal cord became apparent after the first operation, we considered that posterior decompression was sufficient to resolve the syringomyeli. Since syringomyelia is rarely associated with degenerative spinal disease, it is necessary to consider the coexistence of another factor that is causing the disturbance of the subarachnoid CSF dynamics, such as tumor, inflammation, arachnoid cyst, or arachnoid web.
More than 80% of the patients with arachnoid web underwent membranectomy with dural opening, where the neurological symptoms improved in 91% of the patients.12) These results suggest that surgical outcomes are usually good.
In our case, gait disturbance and impairment of deep sensation in the lower limbs improved, even though the diagnosis was confirmed 4 years from the symptom onset. We considered the surgical intervention to be very effective in our case. Although posterior decompression using laminectomy and removal of the OYL partially improved the syrinx status, surgical membranectomy was an indispensable procedure that ensured restoration of CSF dynamics around the spinal cord. This was beneficial since the main cause of the syrinx was the disturbance of the subarachnoid CSF dynamics.
In conclusion, we successfully treated a case of syringomyelia associated with both thoracic OYL and arachnoid web formation. Syringomyelias are rarely caused by degenerative vertebral diseases alone and in those cases when they coincide with a syrinx, clinicians should consider the coexistence of an underlying lesion affecting the arachnoid membrane and subarachnoid CSF dynamics. Although the pathogenesis of arachnoid webs is not well understood, they might be caused by degenerative diseases, such as OYL, which stimulate the adjacent arachnoid membrane or possibly pre-existing arachnoid cysts.
We thank all members of Iseikai Hospital for the assistance of this research.
This study has been performed in accordance with the Declaration of Helsinki and approved by the Ethical Committee of Iseikai Hospital. Witten, informed consent was obtained from the patient.
Authors have no conflicts of interest in this research.