2022 Volume 9 Pages 357-363
2022 Volume 9 Pages 357-363
Cerebral edema around the lead has been reported as a complication of deep brain stimulation; however, the causes remain unknown. Herein, we present a rare case of sudden cerebral edema around the lead occurring after deep brain stimulation. This was accompanied by cerebrospinal fluid (CSF) leakage into the subcutaneous thoracic pocket around the implantable pulse generator in a 53-year-old man with Parkinson's disease. No such case has been reported thus far. Lumbar drainage was performed to improve CSF leakage. The cerebral edema initially responded to steroids, but then it stopped responding to treatment. The edema appeared alternately on the left and right sides, and cyst formation was noted around the left lead. There are some reports of cyst formation around the lead; however, in our case, images were used to monitor the edema and cyst from their appearance to their disappearance. Our data suggest that cyst formation and cerebral edema are related.
Deep brain stimulation (DBS) is an established treatment for Parkinson's disease (PD).1) However, it has been reported to cause complications, such as bleeding, infection, and hardware-related trouble,2) and in recent years, there have been reports of non-infectious cerebral edema around the leads;3-20) cases of cyst formation around the lead have also been reported.4,9,11,15,21-23) Here, we report a rare case of sudden cerebral edema after DBS accompanied by cerebrospinal fluid (CSF) leakage to the skin of the chest. The edema was non-infectious, alternating left and right, with cysts around the lead, and took 3 months to resolve, despite steroid administration. In addition, we reviewed the literature regarding symptomatologic non-infectious edema and cysts around the lead.
A 53-year-old man developed a right upper limb tremor 6 years prior to visiting our clinic and was diagnosed with PD. As the symptoms progressed, the patient was admitted to our hospital for DBS. The condition before surgery was Hoehn and Yahr stage 3 and the Unified Parkinson's Disease Rating Scale (UPDRS) Part III on/off score was 8/35. Preoperatively, his daily medications included levodopa-carbidopa hydrate-entacapone 350 mg, selegiline 7.5 mg, ropinirole 4 mg, istradefylline 40 mg, gabapentin enacarbil 300 mg, and levodopa benserazide hydrochloride one tablet, as per-request medication. No cognitive decline was observed, and the mini-mental state examination score was 30/30. Head computed tomography (CT) /magnetic resonance imaging (MRI) showed dilation of the frontal subdural space due to marked brain atrophy (Fig. 1a).
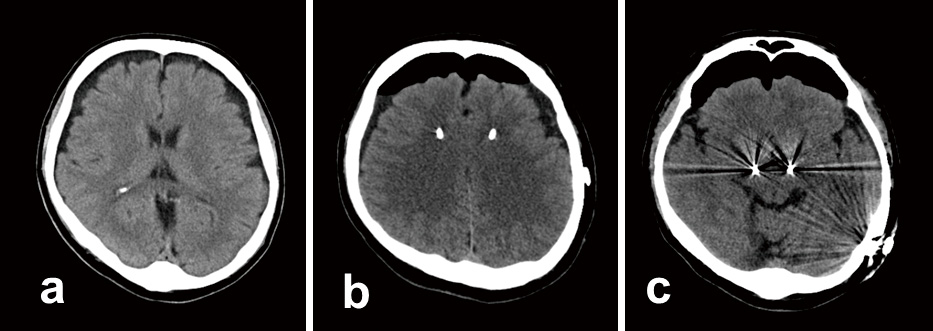
Pre- and postoperative computed tomography images.
(a) Preoperative image showing dilation of the subdural space due to cerebral atrophy. (b, c) Images immediately after operation. Air retention in the skull, but not intracranial hemorrhage, was observed. The lead was inserted at the target site.
Bilateral subthalamic DBS was performed. The subdural space was dilated, and when the arachnoid membrane was incised, CSF leaked. The intraoperative recording was performed using three microelectrodes to determine the lead placement site without keeping the patient awake. After inserting the microelectrode, fibrin glue was applied to the burr hole to prevent CSF outflow. Intraoperative test stimulation was not performed. The device used was a Vercise Gevia RC with a directional lead (Boston Scientific, MA, USA). After lead placement in the bilateral subthalamic nuclei, an implantable pulse generator was placed under the left greater pectoral muscle fascia. Postoperative CT showed that air was present in the skull due to the outflow of CSF, and no intracranial hemorrhage was observed (Fig. 1b, c). The leads were inserted into the target sites.
Postoperative clinical time course was summarized in Fig. 2. Postoperatively, the patient complained of headaches and was prescribed acetaminophen. The next day, bilateral monopolar stimulation was initiated (1 mA, 30 μs, 130 Hz). Seven days postoperatively, each contact was stimulated, the stimulation effect and side effects were confirmed, and the stimulation was adjusted with reference to the results. Head CT performed on the same day showed no brain edema (Fig. 3a). On the 13th day, the site of implantation in the left anterior chest suddenly became swollen, and CT on the 14th day showed marked cerebral edema around the right lead (Fig. 3b). Blood sampling showed a slight increase in the proportion of eosinophils, but without leukocytosis or C-reactive protein increase (white blood cell 7880/μL [neutrophils 78.9%, eosinophils 8.1%], C-reactive protein 0.22 mg/dL). Oral dexamethasone (9.9 mg/day) was administered, but on the 16th day, the edema around the right lead increased (Fig. 3c, d). Therefore, intravenous dexamethasone (6.6 mg) was administered for 3 days; then, the dose was gradually decreased for 7 days, and osmotic diuretics were administered. On the 28th day, the edema around the right lead decreased; however, edema appeared around the left lead (Fig. 3e).

Chronological time course of the present case.
The horizontal axis in each row indicates the number of days since the surgery.
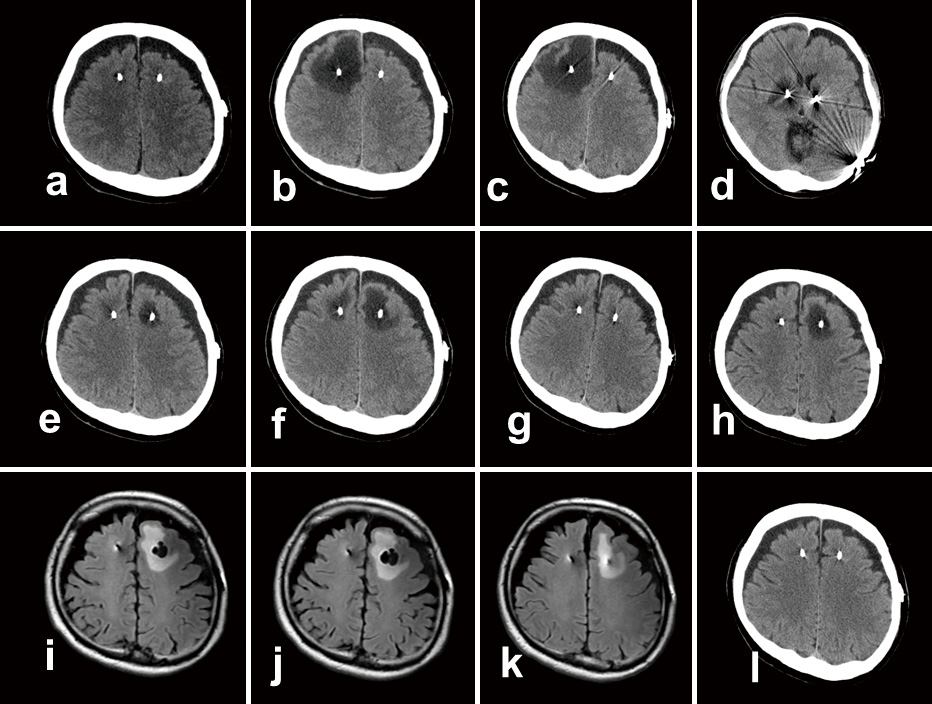
Radiographical findings shown in chronological order.
Images were obtained on days (a) 7, (b) 14, (c, d) 16, (e) 28, (f) 33, (g) 42, (h) 49, (i) 71, (j) 78, (k) 89, and (l) 97.
(a-h, l): Computed tomography.
(i-k) Fluid-attenuated inversion recovery magnetic resonance imaging.
(a) Edema was not seen in the images up to 7 days postoperatively, (b) but suddenly appeared 14 days after the operation. (c-d) Edema peaked on day 16 and extended to the tip of the lead. (e) After administration of steroids, the edema was reduced on the right side, but appeared on the left side. (f) The edema was enlarged predominantly on the left side. (g) After lumbar drainage, edema almost disappeared on both sides. (h) Edema reappeared on the left side on day 49. (i-k) Cysts formed around the left lead. (l) Eventually, both the cyst and edema disappeared.
A left anterior chest skin incision was made on the 33rd day (Figs. 3f and 4a, b), and serous fluid outflowed. The β-transferrin test was not performed because it is not covered by national health insurance in Japan; however, the fluid was visibly determined to be CSF based on the properties of the stored liquid. Bacteria were not detected in the culture test. As CSF retention was again observed in the chest on the 34th day, CSF lumbar drainage was performed the following day. CSF retention in the chest disappeared, and lumbar drainage was removed on day 41. The edema had nearly disappeared by the 42nd day (Fig. 3g). However, a CT scan on day 49 showed recurrence of edema around the left lead (Fig. 3h). After 71 days, MRI showed cyst formation around the left lead (Fig. 3i). The patient showed no response to steroid treatment as the edema persisted and the cysts increased in size (Fig. 3j). Contrast-enhanced MRI showed no lesions and CSF examination showed no signs of infection. On the 89th day, the edema had decreased and the cyst disappeared; the patient was discharged from the hospital (Fig. 3k). On CT, the edema had disappeared completely by day 97 (Fig. 3l) and no recurrence was seen on CT after 4 months. The UPDRS improved to a Part III on/off score of 9/9.
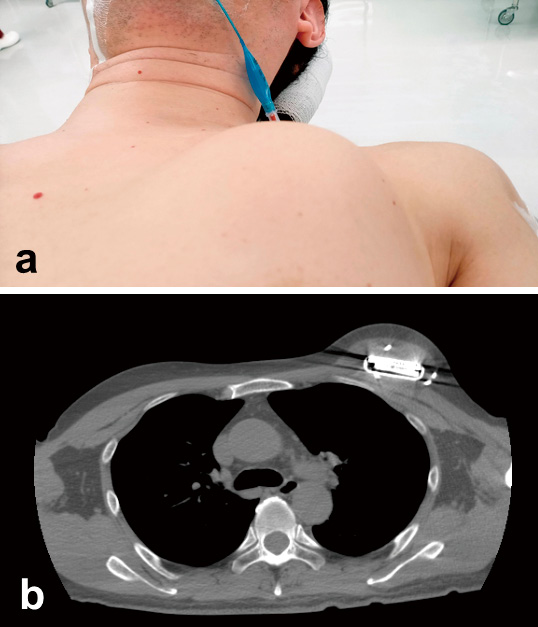
Cerebrospinal fluid leakage to the chest subcutaneous pocket.
(a) Photograph before left chest resection performed at 33 days post-surgery. Cerebrospinal fluid accumulated under the skin of the chest, which is swollen. (b) Fluid collection was observed around the implantable pulse generator on computed tomography.
In the present case, cerebral edema appeared around the lead after DBS, and CSF leaked into the subcutaneous pocket of the chest. The edema around the lead first appeared on the right side, disappeared once, then appeared on both sides, and finally disappeared; however, edema on the left side appeared and lasted for more than 1 month. Initially, the edema responded to the steroid treatment, but then it stopped responding; however, the cysts around the lead eventually disappeared. There are no other reports of edema alternately appearing on the right and left sides. The present case appears to be a valuable one, as the appearance and disappearance of edema and cysts could be chronologically observed from the images.
Symptomatic non-infectious cerebral edema after DBS was confirmed in 91 cases, including the present case (Supplementary Table 1).3-17,19,20,23,24) The incidence was reported to be 0.6%-31.6% (per number of operations)4,10,11,13,16,17) and 1.7%-4.1% (per lead).6,20) There have been reports of edema, with most studies reporting edema on one side and only a few reporting edema on both sides. Excluding studies where surgery was conducted on only one side, 49 unilateral and 18 bilateral cases have been reported; however, there are no reports on cases with alternating appearance of edema, as in the present case. Edema appeared no matter which site the lead was inserted. Symptoms of edema such as headache, seizure, worsening of preoperative symptoms, hemiplegia, and aphasia have been reported. There are no reports of CSF leakage, as in this case. In the literature, all cases showed improvement upon steroid administration (dexamethasone was used in most cases4,6,11,13,14,18-20,23)), or even with routine monitoring without any treatment.3,5,10,15) Our patient stopped responding to steroid treatment in the second half of the treatment period for an unknown reason.
Despite the large number of cases reported, the causes of peri-lead edema for DBS are still unknown. As for the possible causes of edema, the blood-brain barrier may collapse due to brain injury caused by microelectrodes and/or lead insertion, but the reason for edema appearing alternatingly on one side at a time, as in this case, cannot be explained. Initially, steroid treatment seemed effective; however, drug-resistant edema appeared on the contralateral side and resolved spontaneously after 3 months. Steroids were administered for peri-lead edema in most previous reports, which suggests that the development of edema may have been vasogenic; however, steroids were not effective in this case. The cause of the edema may rely on other mechanisms. Whiting et al. compared 15 patients with edema and 87 patients without and observed no significant differences in age, sex, angiopathy, hypertension, antithrombotic drug use, anesthesia method (awake/asleep), target, disease, number of leads, number of punctures, and presence or absence of microelectrode recordings between the two groups.16) Saitoh et al. classified peri-electrode edema after DBS into the following two types: (1) limited edema in deep white matter and (2) extensive edema in surface white matter. They speculated that the former type may be caused by microvessel occlusion; however, the cause of the latter has yet to be elucidated.25) Edema exhibited delayed onset rather than immediate occurrence after surgery in the previous studies. Half of the cases are reported to have appeared after the 5th day;6) however, there are also reports describing appearance after 200 days3) or even 5 years later.11) Regarding the time of onset, most cases developed within 1 week, although some cases develop after 2 or 4 weeks (Supplementary Table 1). Those that developed within 1 week may be affected by the invasion of the brain by microelectrode recording or lead insertion, but those that developed late may be related to other mechanisms.
The incidence of seroma as a complication of DBS was reported to be 0.26% in a systematic review of 96 articles, 20 of which were at the implantable pulse generator site.26) This appears to be a relatively rare complication. Three articles (five cases) were identified, in which a CSF leak caused fluid retention in the thoracic subcutaneous pocket.27-29) Two articles (four cases in total) showed improvement upon bandaging the patients' heads with pressure.28,29) In the remaining case, lumbar drainage was performed as in the present case, and improvement was noted.27) In two cases, the time of onset was 4 and 9 days postoperatively.27,28) None of those reports described imaging findings at the time when the CSF leak appeared and, therefore, we could not confirm whether there was cerebral edema.
One of the factors causing CSF leakage might be dilation of the subdural space, and the CSF likely leaked owing to the increased intracranial pressure caused by the cerebral edema. The burr hole should be sealed tightly with fibrin glue or other materials to prevent CSF from leaking out. We inserted three microelectrodes using the multitrack method. After insertion, the burr hole was packed with fibrin glue; however, two holes remained, as a single lead was inserted and three electrodes were removed. In the present case, CSF could have leaked from these holes. Particular attention is needed when the subdural space is enlarged owing to brain atrophy, as in the present case. In this case, the brain edema was ameliorated with lumbar drainage. If the edema around the leads was caused by the influx of fluid into the brain intercellular space owing to the disruption of the blood-brain barrier, decreasing the intracranial pressure by drainage may allow the fluid in the brain intercellular space to drain out, which may mitigate the cerebral edema. The absence of edema around the catheter during ventricular drainage or shunt surgery may be due to the reduction of intracranial pressure via drainage.
Regarding cases of cyst formation around the lead, 15 cases, including the present case, were confirmed (Supplementary Table 2).4,9,11,12,15,21-23) Three patients were asymptomatic.11,21) Cyst formation on both sides was observed in one case.9) Cases of cyst formation were divided into two types, one accompanied by air and edema within a few days of surgery,4,12) and the other characterized by delayed onset, wherein cysts are confirmed several months later.9,11,15,21-23) The lead was removed in seven cases, after which the cysts resolved.11,21-23) One patient developed hydrocephalus due to cyst formation.21) Eleven patients were confirmed to have edema. The present case is valuable as it demonstrated that there is a relationship between edema around the lead and the appearance of cysts over time. There were four cases without peri-lead edema, but the formation of cysts was confirmed at more than 8 months after DBS surgery; it is possible that these patients had edema before the formation of cysts.
Regarding treatment, Jagid et al. reported a protocol for the treatment of edema in these cases.9) The possibility of infection is first ruled out and then steroids are administered. Although the protocol for cases of steroid lack of effect, as in this case, is not described in the protocol, it is necessary to rule out the possibility of infection and carefully follow up the patient without removing the device. It is also necessary to fully explain to the patient, prior to surgery, that non-infectious cerebral edema and cysts may appear around the lead after DBS. Sharm et al. compared the preoperative and 1-year postoperative Montreal cognitive assessment findings in a group with edema and showed no significant reduction of cognitive function.20) Doctors should explain to the patients that the appearance of edema will not cause a decline in cognitive function, and it is thus not a complication to be concerned about.
Here, we report a case of CSF leakage in the subcutaneous pocket of the chest due to cerebral edema around the DBS lead. If the subcutaneous pocket of the chest is swollen, it is necessary to determine whether cerebral edema has appeared. It is also necessary to fully explain to the patients, prior to surgery, that non-infectious cerebral edema and cysts may appear around the lead after DBS. The cause of cerebral edema is still unknown; thus, future research should aim to elucidate the cause of cerebral edema and establish preventive methods.
This study was approved by the ethics committee of Kanazawa Neurosurgical Hospital (approval number ID30-11), Ishikawa, Japan. The patient provided written informed consent for the publication of the clinical data and accompanying images.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
The authors have no potential conflicts of interest related to this report.