2022 年 9 巻 p. 377-382
2022 年 9 巻 p. 377-382
Carotid endarterectomy (CEA) and carotid artery stenting (CAS) for internal carotid artery (ICA) stenosis have specific risks. Therefore, the accurate evaluation and management of each risk factor are important, especially for patients who are at high risk for both CEA and CAS.
We report the case of a 77-year-old man with right ICA stenosis that progressed despite optimal medical treatment. In addition, he had several risk factors for both CEA and CAS, including previous cervical radiation therapy, contralateral ICA occlusion, chronic kidney insufficiency, and severe aortic valve stenosis. CEA was performed with priority given to aortic valve stenosis without complications, and the patient was discharged 10 days postoperatively, without neurological sequelae. However, a pericarotid cervical abscess was detected by carotid echo, computed tomography (CT), and magnetic resonance imaging (MRI) 1 month after CEA that required surgical drainage. The infection was thought to be odontogenic because the pathogen was identified as normal oral bacterial flora, and a wound infection was not apparent. Teeth extraction and abscess drainage, in combination with antibiotic therapy, successfully cured the infection without additional complications.
Odontogenic cervical abscesses after CEA can occur, especially if the patient is at risk of infection. Therefore, both preoperative and postoperative dental evaluation and management are recommended. As in this case, a cervical abscess can occur without wound infection, and the abscess diagnosis is sometimes difficult from wound inspection alone. Cervical echocardiogram and CT were useful for detecting fluid collection, whereas MRI was useful for qualitatively evaluating the lesion.
Carotid endarterectomy (CEA) is the most well-established surgical treatment for internal carotid artery (ICA) stenosis. However, CEA is now being replaced by carotid artery stenting (CAS) in an increasing number of cases, since its non-inferiority relative to CEA has been proven.1) The indications for CEA or CAS are judged on the basis of their specific risks. However, we often encounter patients who are considered high risk for both CEA and CAS. In such cases, careful consideration is needed, for which the accurate evaluation and management of each risk factor are essential. CAS is mainly performed for patients who are at high risk for CEA treatment, and previous radiation therapy to the neck is among those risks, partly because of the increased risk of infection.2,3)
Notably, CEA and CAS have specific postoperative complications. Although we seldom experience operative site infection after CEA and abscesses are rare, infections are a lethal complication. In the literature, cases of patch infections after CEA, including abscess formation, have been reported.4-6) However, to our knowledge, there have been no reported cases of abscess after CEA without prosthesis.
Here, we report the case of a patient with an odontogenic cervical abscess that occurred following CEA for ICA stenosis after cervical radiation therapy. The patient was successfully treated with surgical drainage and antibiotic medications. Furthermore, we discuss the infection route and the recommended management for similar cases.
We present the case of a 77-year-old man with right ICA stenosis and left ICA occlusion. He continued to be asymptomatic for more than 10 years since his initial presentation to our department. The left cerebral hemisphere was perfused by sufficient collateral flow via the anterior communicating artery from the contralateral side and the ipsilateral posterior communicating artery. However, he became symptomatic thereafter. Another magnetic resonance imaging (MRI) revealed progressive stenosis in the right ICA despite optimal medical treatment with clopidogrel sulfate (75 mg/day) and pitavastatin calcium (2 mg/day) (Fig. 1A), which caused transient visual dysfunction in his left eye when his blood pressure was low. The patient had a history of cervical radiation therapy for laryngeal cancer that occurred 12 years prior, coronary artery bypass grafting, severe aortic stenosis, and chronic kidney disease (serum creatinine, approximately 1.9 mg/dL). As a surgical intervention, CEA was selected instead of CAS since the patient had severe aortic valve stenosis, which is considered a contraindication for CAS. However, CEA was also considered high risk because the patient had a history of cervical radiation and a contralateral ICA occlusion. CEA was successfully performed under general anesthesia using a vascular shunt, and the stenotic lesion was successfully removed (Fig. 1B). Intraoperatively, the influence of previous radiation therapy, such as scar formation, tissue adhesion, and vulnerability of the arterial wall, was not apparent objectively (Fig. 1C). The carotid artery was sutured using a Gore-Tex suture without a prosthetic patch. The postoperative course was uneventful. Minocycline was administered to prevent both wound infection and cerebral hyperperfusion syndrome for 7 days after surgery. A computed tomography (CT) scan 7 days after surgery revealed a small amount of fluid in the carotid space that was not apparent 1 day after surgery (Fig. 2A, B), which was thought to be exudate, and the patient was discharged. Approximately 1 month after surgery, the patient visited our outpatient clinic with transient swelling around his right jaw. Physical examination revealed no remarkable findings, including signs of wound infection or fever; however, CT and carotid duplex ultrasound revealed increased fluid collection in the right pericarotid space (Figs. 2C and 3A). The ICA was patent, and there were no findings suggestive of a pseudoaneurysm or intravascular thrombus. Since an infection could not be ruled out, antibiotic treatment with levofloxacin was started immediately. Additionally, MRI was performed for qualitative evaluation of the fluid on the following day, and the findings were suggestive of pericarotid cervical abscess because of the high intensity on diffusion-weighted imaging (DWI) (Fig. 3B). The patient underwent surgical drainage under local anesthesia (Fig. 3C, D), and the antibiotics were changed to sulbactam/ampicillin + teicoplanin. Intraoperatively, the carotid artery appeared normal without signs of infection, so the Gore-Tex suture was left behind. Streptococcus intermedius was isolated from the abscess as the pathogen, and teicoplanin was discontinued based on the antibiotic sensitivity test. The fluid with high intensity on DWI disappeared on the MRI scan that was performed 8 days postoperatively. Because the infecting pathogen generally constitutes normal oral bacterial flora, we performed dental examination to determine the source of the infection. Notably, tooth decay of the mandibular teeth on both sides was identified. Tooth extraction was performed by a dentist. The antibiotics were changed to oral amoxicillin/clavulanate, and the patient was discharged. The antibiotics were continued for 5 weeks after surgery. No signs of reactivation of the infection or other vascular complications were found on follow-up examinations over a year after antibiotic treatment completion.
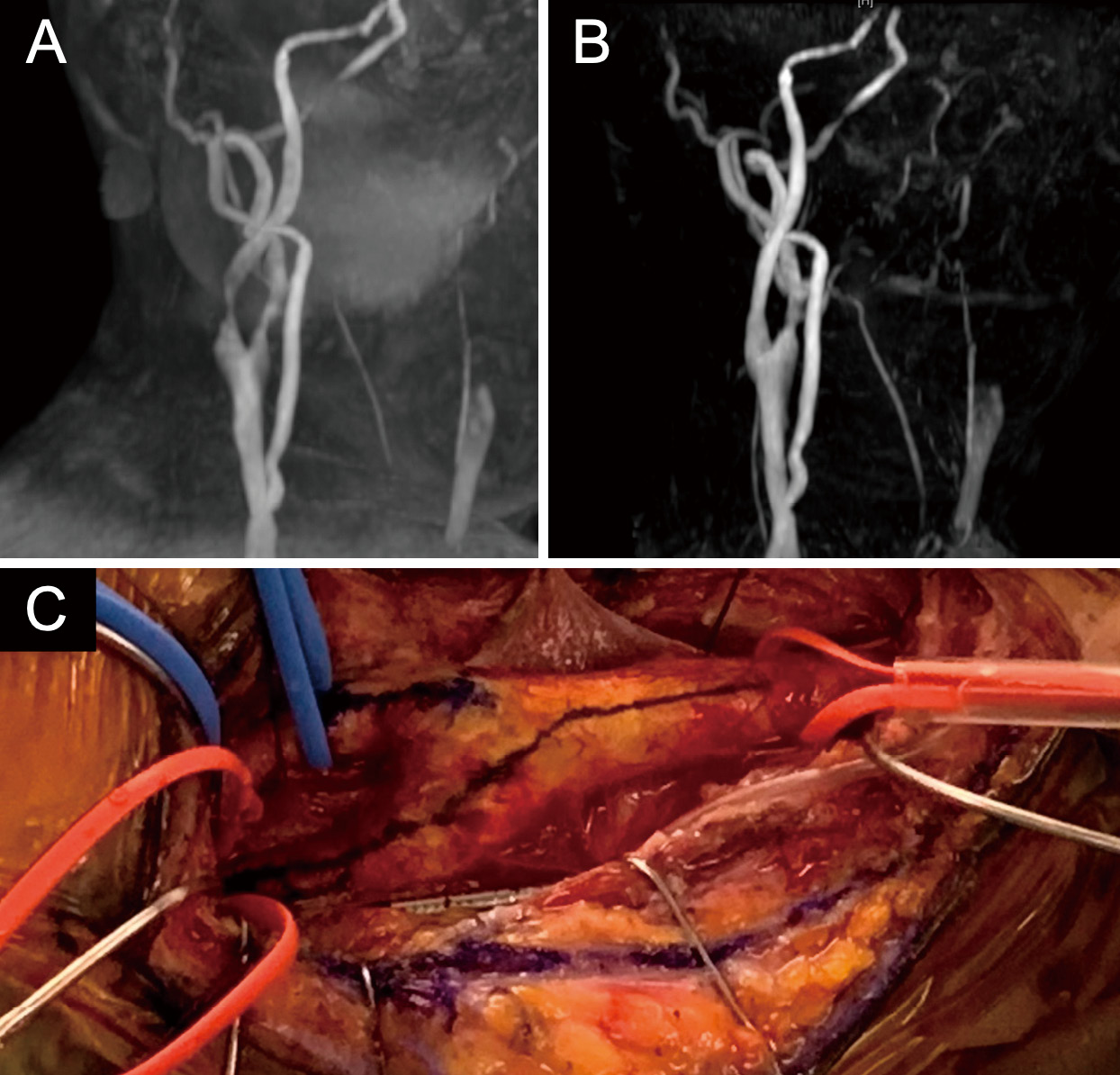
Maximum intensity projection image of pre-(A) and postoperative (B) magnetic resonance angiography. Intraoperative view of the exposed carotid artery (C).

Axial image of the surgical site by computed tomography 1 (A) and 7 days (B) after carotid endarterectomy, when the abscess was detected (C).
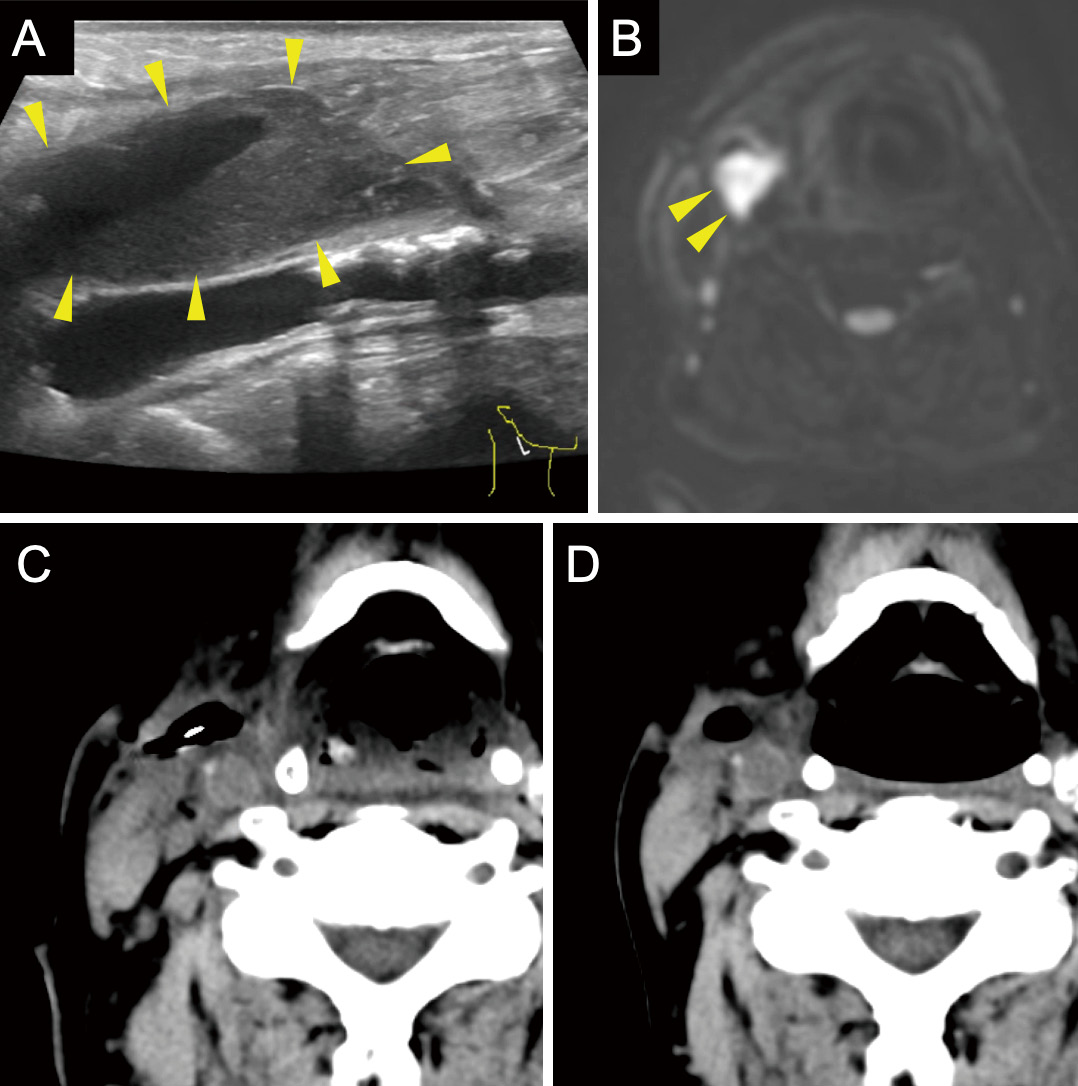
The pericarotid abscess was depicted as a heterogeneous echoic area in the carotid duplex ultrasound (A) with high intensity on diffusion-weighted image (B). Axial image of the surgical site by computed tomography after surgical drainage of the abscess (C) and at the time of discharge (D).
In this case, an odontogenic pericarotid cervical abscess occurred after CEA. We speculate that the risk factors for tooth decay and previous cervical radiation therapy were related to cervical abscesses in this case. Carotid duplex ultrasound and MRI are useful for detecting and diagnosing cervical abscesses, especially when the patient has faint subjective symptoms and no apparent signs of infection at the surgical wound.
Although CEA for ICA stenosis after cervical radiation therapy is reported to have a higher risk of postoperative infections,2,3) such infections are rare because wound infections following CEA rarely occur. It has been reported that 0.4%-1.8% of patients who undergo CEA with prosthetic patch closure will develop patch infection.4) It has been also reported that the most frequent clinical presentation of patch infection is pericarotid cervical abscess (46%).5) These findings suggest that abscesses can occur following CEA when patients have certain risk factors. The most common pathogens that cause cervical infections are reported to be staphylococci.4,6) In the current case, previous cervical radiation therapy was a risk factor.2,3)
Deep cervical infections can occur without surgery. They are most commonly caused by the extension of an infection in the mandibular teeth, tonsils, parotid gland, cervical lymph nodes, middle ear, and sinuses. Such infections have become relatively uncommon in the post-antibiotic era; however, we must be aware of such infections because they often have a rapid onset and can progress to life-threatening complications.7) It is essential to understand the pathogenesis of infections in compartments where the deep neck space is divided into several compartments by the cervical fascia.8) Carotid sheath involvement is a dreaded state because it has the potential for carotid artery erosion and suppurative jugular thrombophlebitis.9) The carotid space also has the potential to provide a direct path for descending necrotizing mediastinitis, which is often referred to as the "Lincoln highway." 10) Carotid artery mycotic aneurysms are reported to have a mortality rate of approximately 20%.11) In general, the most common infectious organisms are viridans streptococci, which reflect their abundance in the mouth.12-15) Generally, the initial clinical presentation is often a sore throat, trismus, or other symptoms, which are determined by the primary source of infection. In our patient, although the infection site was the surgical site, the carotid abscess was thought to have an odontogenic source because the wound itself was clear (not reddish) and showed no signs of infection. The pathogen isolated from the abscess was S. intermedius, which is not a common infective agent after CEA and is not present in the normal skin bacterial flora. Instead, it is present in normal oral bacterial flora, and the patient had tooth decay. S. intermedius is included in the viridans group of streptococci and is known to cause abscesses in the brain and liver. In the current case, we speculate that the cervical abscess was caused by overlapping risks. Preoperatively, the lymphatic barrier around the carotid space, which had deteriorated by radiation therapy, had managed to constantly eliminate the infective organisms attributable to the tooth decay. Surgical manipulation further injured the lymphatic system and resulted in infection. Yasuda et al. reported a case in which surgical injury to the parotid gland was thought to affect infection after CEA,16) but in the current case parotid gland injury was not apparent. Preoperative dental screening was not routinely performed in our department. In this patient, the tooth decay was not treated preoperatively. However, preoperative dental screening and treatment of dental lesions, if needed, might have been favorable if the patient had a risk of infection, such as previous radiation therapy. Oral infections are reported to be related to carotid artery stenosis and its progression;17,18) therefore, earlier and periodic dental screening may be favorable for ICA stenosis. The small amount of fluid found on the CT scan that was taken 7 days after surgery could be a sign of infection; however, it is a relatively common finding after CEA. Notably, we should have observed the fluid more closely, which would have allowed an earlier detection of the abscess. In this patient, after CEA, we administered minocycline as an antibiotic because it can prevent hyperperfusion syndrome. Minocycline, which is administered to prevent both wound infection and cerebral hyperperfusion syndrome as described previously,19) has a broad antibacterial spectrum and covers normal oral and skin bacterial flora. Therefore, this antibiotic may also have a prophylactic effect on odontogenic infections in addition to a bacteriostatic effect, rather than a sterilization effect. Antibiotics that have sterilization effects are recommended for patients who are at risk of postoperative infection.
Interestingly, in a systematic review of prosthetic infection after CEA,4) the timing of infection appeared to follow a bimodal distribution, with one-third presenting within 2 months of the original procedure, usually with a preceding wound infection. Furthermore, two-thirds presented in >6 months, seldom with wound infection. Although no discussion was made about the source of infection in that review, the latter group appeared to have a different etiology from the former group. The former type is thought to be an extension from wound infection, whereas the latter type is thought to be caused by slow bacterial growth on prothesis after intraoperative contamination. In the current case, early infection without sign of wound infection or prothesis occurred, suggesting an uncommon etiology caused by overlapping risks. The early detection of an abscess was possible because it occurred relatively early, and the patient was still under close postoperative follow-up. However, the preoperative treatment of tooth decay might have improved the patient's condition.
For the current patient, carotid duplex ultrasound and MRI were useful for detecting and diagnosing the carotid abscess. The early diagnosis of a carotid abscess enables early surgical drainage and antibiotic treatment, which help in avoiding the most severe complications of pseudoaneurysms and suppurative thrombophlebitis. It was difficult to suspect a carotid abscess from the patient's physical examination, which included a wound inspection because the patient had no signs of wound infection or inflammation in his mouth and throat. With duplex ultrasound, fluid accumulation, the vascular flow state, and intravascular thrombus can be easily observed. Although the presence of fluid in ultrasound findings is nonspecific, adding DWI to MRI was helpful in providing a qualitative evaluation of the fluid, which led to treatment decisions.
As mentioned above, many cases of carotid infection after CEA have a late onset without any signs of wound infection, and thus, close observation is needed. This idea might also be applicable to other cervical surgeries. However, to the best of our knowledge, no such study had discussed postoperative infections.
Attention should be paid to odontogenic cervical abscesses after CEA, especially if the patient has specific risks, such as previous cervical radiation therapy and intraoperative prosthetic patch closure. Both preoperative and postoperative dental screening are favorable for such patients. Treatment prior to CEA is recommended if dental lesions are found. Postoperative carotid infection can occur even in the late period and sometimes presents with only faint symptoms. Carotid duplex ultrasonography and MRI are useful for such diagnoses.
Consent was obtained from all the participants.
The authors declare that they have no conflict of interest. All authors are members of the JNS and have registered online self-reported COI Disclosure Statement Forms through the website for JNS members.