論文ID: cr.2016-0308
論文ID: cr.2016-0308
We present a case of double-crushed L5 nerve root symptoms caused by inside and outside of the spinal canal with spur formation of the lumbosacral transitional vertebra (LSTV). A 78-year-old man presented with 7-year history of moderate paresis of his toe and left leg pain when walking. Magnetic resonance imaging (MRI) revealed spinal stenosis at the L3/4 and 4/5 spinal levels and he underwent wide fenestration of both levels. Leg pain disappeared and 6-min walk distance (6MWD) improved after surgery, however, the numbness in his toes increased and 6MWD decreased 9 months after surgery. Repeated MR and 3D multiplanar reconstructed computed tomography (CT) images showed extraforaminal impingement of the L5 root by bony spur of the left LSTV. He underwent second decompression surgery of the L5/S via the left sided Wiltse approach, resulting in the improvement of his symptoms. The impingement of L5 spinal nerve root between the transverse process of the fifth lumbar vertebra and the sacral ala is a rare entity of the pathology called “far-out syndrome (FOS)”. Especially, the bony spur formation secondary to the anomalous articulation of the LSTV (LSPA) has not been reported. These articulations could be due to severe disc degeneration, following closer distance and contact between the transverse process and the sacral ala. To our knowledge, this is the first report describing a case with this pathology and may be considered in cases of failed back surgery syndromes (FBSS) of the L5 root symptoms.
Lumbosacral transitional vertebra (LSTV) is known as both the congenital numerical anomaly of vertebrae, such as sacralization or lumbarization (L6), and the developmental degeneration that make contact with the L5 transverse process onto the sacral ala to establish the pseudoarticulation (LSPA). The previous reports of LSTV mainly noted the correlation between the existence of LSTV and low back pain (LBP). The LSPA should be included in the criteria for severe lumbar degenerative pathology secondary to the reduction of disc height and/or coronal inclined bony structure. Recent highly advanced imaging technology coupled with an aging population has led to the detection of multiple factors that can cause L5 radiculopathy, i.e., originating from not just L4/5 disc level stenosis but L5/S1 lateral recess stenosis, L4/5 foraminal stenosis and far-lateral entrapment of the nerve root by various cause such as disc herniation and bony spur formation. Thus, we must keep in mind that multiple crush pathology of the L5 root inside the canal, foramen, and extraforaminal zone to avoid the so-called “failed back surgery syndrome (FBSS).” Here, we present a case of double-crushed L5 nerve root due to spinal stenosis and LSPA.
A 78-year-old male who had a history of L2–4 level lumbar decompression surgery 20 years ago, presented with moderate paresis of his left toe extension and left leg pain that persisted for seven years. He was treated conservatively at another institution over 4 years before our consultation, however, symptoms gradually deteriorated. On initial examination, he complained severe left leg pain during walking and he had hyperesthesia of his left L5 dermatome and manual muscle test (MMT) 4/5 weakness of his left toe and ankle extension. Radiographical examination revealed a Meyerding grade I spondylolisthesis indicating anterior slippage of L3 and L4 vertebral body and moderate spinal stenosis at L3/4, 4/5 level (Fig. 1). Dynamic radiographs did not show apparent instability, therefore, the patient underwent partial laminectomy using spinous process splitting. After surgery, outside femoral pain had quickly disappeared and his 6-min walk distance (6MWD) gradually extended up to 320 m; a considerable improvement compared with his record of 195 m before surgery (Fig. 2). However, 9 months after surgery, dysesthesia of his toes and moderate weakness of the toe muscles deteriorated, which resulted in decrease his 6MWD down to 270 m. Neither magnetic resonance imaging (MRI) nor dynamic plain radiographs demonstrated any obvious changes and the spinal canal was widely decompressed, both of which implied that there was no new lesion inside both the spinal canal and the intervertebral foramen. However, a close review of MR myelogram and 3D multiplanar reconstructed computed tomography (CT) images concluded bilateral lumbosacral transverse vertebra (LSTV) of the Castellvi Type IIB that had severe bony spur formation compressing the left L5 nerve root toward the anterior exit zone (Fig. 3). Selective nerve root block of his left L5 provided temporary amelioration, and therefore, we diagnosed as having double crush of inside and outside of the left L5 nerve root. He underwent second decompression surgery of the L5/S1 extraforaminal area via the Wiltse approach. A linear skin incision was made at the point 4 cm lateral from the midline. A blunt dissection between the multifidus and the longissimus muscle was made, then the lateral aspect of L5 superior facet, caudal part of L5 transverse process, and the cranial part of the sacral ala were exposed. The space surrounded by those structures was quite narrowed. Bone removal using a 4-mm coarse diamond burr was made on transverse process and ala so that the L5 nerve root could decompressed and the depth was occasionally measured to safely decompress the L5 root (Figs. 4a and 4b). After the second surgery, the patient’s toe muscle power improved up to MMT 5/5, his dysesthesia almost disappeared and his 6MWD improved up to 305 m. His symptoms as FOS had not recurred for over two years after surgery (Fig. 5).

Preoperative MRI showing moderate spinal stenosis at the L3/4 level (a) sagittal, (b) axial view, (c) and recessus stenosis at L4/5.

Postoperative MRI revealed no compressive lesion inside the spinal canal at L4/5. (a) sagittal and (b) axial view.

(a) Plain radiograph showed bilateral Castellvi type IIb LSTV, (b) 3D-CT showed severe degenerative change and bony spur formation at left LSTV, (c) MRI axial image revealed pinched L5 nerve root at far out zone of L5/S1, (d) CT axial image showed developed spur formation at LSTV.
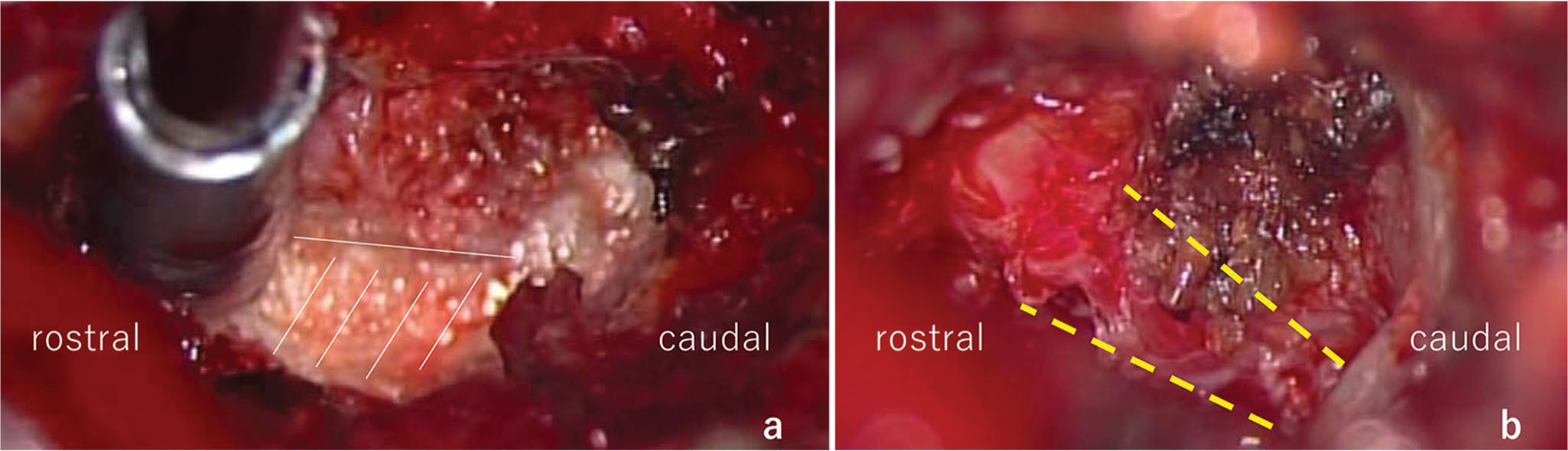
Intrasurgical view. (a) bone removal of LSTV (white oblique line), (b) decompressed L5 root (dotted line).

MRI (a) and CT (b) revealed decompressed far out zone after surgery via posterior Wiltse approach.
A number of previous reports associated with LSTV discussed the relationship between the existence of LSTV and the prevalence of low back pain (LBP).1–3) Prevalence of LSTV was 18.1% with a higher rate in men than in women, and 41.72% were Castellvi Type I (dysplastic enlarged transverse process), 44.1% Type II (pseudoarticulation), 11.5% Type III (fusion), and 5.2% were Type IV (one transverse process fused and one with pseudoarticulation). The prevalence of LBP for Type II and IV was significantly higher. Other authors mentioned that the significance of LSTV had an effect on the surgical outcome of discectomy,4) or idiopathic scoliosis.5)
Recently, several authors reported LSTV associated with radicular symptoms as a formation of “FOS”.6–10) Within the category of “FOS”,11) the L5 nerve root impingement is due to the degenerative spur of LSTV, not by disc bulging. The L5 radiculopathy is often experienced in the daily clinical practice, therefore, when there is a canal +/− lateral recess stenosis at L4/5 or foraminal stenosis at L5/S1, we usually diagnose as responsible lesion(s). In our current case, the extraforaminal lesion may be identified by careful reading of the MR and reconstructed coronal plane CT images of the extraforaminal zone,12) however, it remained concluded as a clinically culprit lesion after the first L4/5 decompression surgery. Sasaki et al. reported a case of L5 radiculopathy that the discectomy inside the L4/5 canal stenosis that had once improved but subsequently reoccurred 1 month after the surgery. The secondary surgery of the L5/S1 lateral disc resulted in complete disappearance of both leg pain and numbness, which concluded to the diagnosis of the double crush of the L5 nerve root.13)
The term of “LSTV” sometimes can be both confusing and misunderstood as congenital “sacralized L5” and “lumbarized S1”.14) It should be kept in mind that the pseudoarticulation between the transverse process and the sacrum includes the degenerative change after the reduction of the disc height and/or scoliosis over the years. Castellvi himself reported that only Type II LSTV presented a herniated lumbar disc at the level of transition,15) which might imply that Type II is the result of spinal degeneration.
In this aging society, Castellvi Type II LSTV may not be a rare entity: a highly developed spondylosis caused by the closer distance between the L5 transverse process and the sacral ala due to the reduction in the disc height following pseudoarticulation at the contact aspects by the loading force over the years. The spur projected inside the articulation easily compresses the L5 root at the extraforaminal zone.3) The formation of LSTV may serve as compensatory responses to inadequate load-bearing capacity of the sacrum,16) or spinal instability secondary to weak iliolumbar ligaments.
Previous reports associated with both spur formation of LSTV and FOS including our case were reviewed (Table 1).6–10) Spur formation at the pseudoarthorosis and/or the lateral osteophyte of the vertebrae between the L5 transverse process and the sacral ala was the reason for the L5 radiculopathy in all nine cases. Mean age was 41.6-year-old (male: female = 6:3). Six patients had low back pain, all had leg pain corresponding to the L5 root, and three patients had paresis of extensor digitorum/halluces longus muscle. Of all, seven L5 radiculopathy was recognized on the left side. Plain radiographs showed Castellvi type IIA (unilateral pseudoarticulation) in four cases and type IIB (bilateral) in five cases. Selective nerve root block of the L5 root was performed in eight cases. The CT findings revealed a bony spur of L5 vertebral lateraltas wall or pseudoarthrosis as the responsible lesion in all cases. It should be noted that except for our case, the MRI findings showed no spinal canal stenosis at L4/5 disc level, and therefore, our case first reported the double crush of the L5 root due to L4/5 spinal stenosis and the spur formation of LSTV pseudoarticulation. Except for two conservatively treated cases, seven patients underwent decompression surgery with no instrumentation. Three surgeries were done via the anterior approach, four were done via the posterior approach, and both resulted in good postoperative course. Sciatica relief was obtained by means of selective nerve root blocks or posterior decompression via a dorsomedial approach. Park et al. recommended microsurgical decompression via a midline posterior approach and obtained enough pain relief without posterior fixation surgery in patients with FOS.17) In contrast, several authors insisted that the anterior approach was better to attain enough decompression around the anterior exit zone of the L5 nerve root.6,8) Weber et al. described two cases of extraforaminal entrapment of the spinal nerve in LSTV Type IIA and implied that the dysplastic facet joints on the level below the transitional vertebra could be one reason for “micromotion” resulting in pseudoarthrosis following osteophytes formation.10) Moreover, the osteophytes of pseudoarthrosis or the lateral side of vertebra implies that a slight amount of motion may occur in L5 and S1 vertebra.10,18) For the above reasons, fixation surgery, such as transforaminal lumbar interbody fusion may be considered as one of the combined strategies.
| Author | Year | Age | Sex | uni/bi | Castellvi’s type | Side | Back pain | L5 leg pain | Paresis | L4/5 canal stenosis | Select RB | Treatment |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Abe E | 1997 | 37 | M | B | IIB | Left | Y | Y | N | N | Y | Anterior decompression |
| Ichihara K | 2004 | 34 | F | B | IIB | Left | Y | Y | N | N | Y | Posterior decompression |
| Ichihara K | 2004 | 36 | M | B | IIB | Left | Y | Y | N | N | Y | Conservative |
| Kikuchi K | 2013 | 70 | F | U | IIA | Left | Y | Y | Y(ext. hallucis) | N | N | Anterior decompression |
| Kikuchi K | 2013 | 53 | M | U | IIA | Left | N | Y | Y(ext. hallucis) | Y(disc) | Y | Anterior decompression |
| Miyoshi Y | 2011 | 29 | M | B | IIB | Right | N | Y | N | N | Y | Posterior decompression |
| Weber J | 2010 | 53 | F | U | IIA | Right | N | Y | N | N | Y | Posterior decompression |
| Weber J | 2010 | 50 | M | U | IIA | Left | Y | Y | N | N | Y | Conservative |
| Present case | 2016 | 78 | M | B | IIB | Left | Y | Y | Y | Y | Y | Posterior decompression |
N: no, RB: root block, Uni/Bi: unilateral or bilateral, Y: yes.
We report a case of double-crushed L5 nerve root due to L4/5 spinal stenosis and the L5/S1 spur formation of LSPA. Double crush syndrome of the L5 nerve root both inside and outside the canal should be noted as a cause of FBSS. Since L4/5 spinal or lateral recess stenosis could be a main cause of L5 nerve root symptoms, posterior decompression or posterior fusion surgeries widely performed. However, concomitant spur formation at pseudoarticulation between the L5 lateral vertebral process and the sacral ala (LPSA) could be an etiology of L5 radiculopathy, this pathology should be considered to treat the persistent or recurred L5 root symptoms after surgery.
None of the authors has any potential conflict of interest.