Article ID: cr.2018-0279
Article ID: cr.2018-0279
Trigeminal neuralgia is caused by compression of the trigeminal nerve by arteries or veins in the posterior fossa. A persistent primitive trigeminal artery variant (PPTAv) is an anomalous artery that may cause trigeminal neuralgia. A 65-year-old man presented with left facial pain. Brain magnetic resonance imaging revealed a PPTAv. Constructive interference in steady state showed that both the PPTAv and the superior cerebellar artery (SCA) compressed the trigeminal nerve. Thus, we performed microvascular decompression and the patient’s symptoms improved. PPTAv is a rare anomaly in the posterior fossa that can cause trigeminal neuralgia. Dual compression of the trigeminal nerve by the SCA and PPTAv demonstrates that trigeminal neuralgia may originate from multiple sources. It is therefore important to check preoperative images to adequately treat trigeminal neuralgia.
Trigeminal neuralgia is caused by pressure exerted by the arteries and veins in the posterior fossa on the trigeminal nerve. The most common artery involved in the condition is reportedly the superior cerebellar artery (SCA), which features in 75–80% of trigeminal neuralgia cases.1) An anomaly that occurs between the carotid and basilar arteries, referred to as a persistent primitive trigeminal artery variant (PPTAv), can cause trigeminal neuralgia. We report a case of trigeminal neuralgia caused by both SCA and PPTAv, as well as its subsequent treatment with vascular decompression.
A 65-year-old man experienced pain in his left face for 10 years, for which he visited the Department of Dental Surgery in our hospital. His facial pain was sharp and lasted for 1–2 min, due to a lesion of the second branch of the left trigeminal nerve. He was prescribed drugs, including pregabalin and carbamazepine, but they were not effective and induced dizziness. Magnetic resonance imaging (MRI) revealed compression of the left trigeminal nerve by the SCA, and he was introduced to our department for operative treatment. A head computed tomography (CT) scan was performed and revealed no abnormalities. CT angiography (CTA) was subsequently conducted and revealed that the PPTAv originated from the internal carotid, passed through Meckel’s cave, and was located in the posterior fossa. Constructive interference in steady state (CISS) showed that the left trigeminal nerve was compressed by both the SCA and the PPTAv.
We determined the diagnosis to be trigeminal neuralgia due to compression by the PPTAv and SCA. As his disease was drug-resistant, we planned to perform an operation by left lateral suboccipital approach. We built 3D reconstruction images from the MRI and CT scans to plan for craniotomy (Fig. 1). As the operation risks causing deafness, we measured the auditory brain-stem response during the operation. Spikes indicative of a normal response were clearly observed. The preoperative image showed that the PPTAv compressed an extensive area of the trigeminal nerve from below (Fig. 2) and that the SCA compressed the nerve from above. We detached the PPTAv from the root entry zone of the trigeminal nerve, after which we observed an impression in the trigeminal nerve. We changed the course of the PPTAv by attaching it to the petrous bone with Teflon felt. We incised and peeled surrounding arachnoid around the trigeminal nerve and SCA for decompression, because it was difficult to achieve a good collimation axis. After the operation, the patient’s symptoms improved and he was discharged from the hospital on foot 8 days after the operation. Postoperative 3D imaging showed that both PPTAv and SCA courses had been changed (Fig. 3). The patient received outpatient medical check-ups for 4 months and his symptoms completely disappeared.

Three-dimensional multimodality image (A: CISS, B: MRI, C: 3D multimodality image) shows that the trigeminal nerve (green) is compressed by both the PPTAv (yellow) and SCA (red).
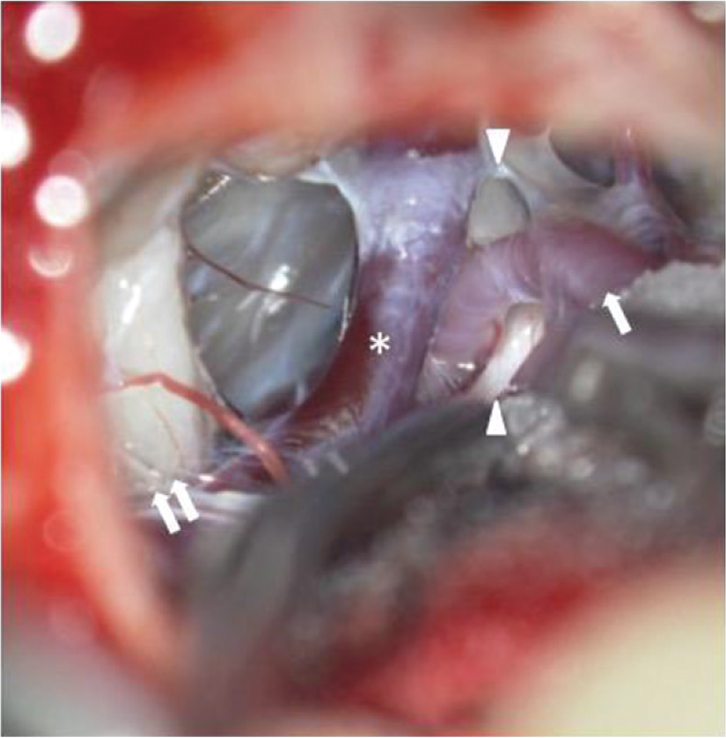
Intraoperative view of left lateral suboccipital approach shows PPTAv compression of the trigeminal nerve from below (arrow head: trigeminal nerve, white arrow: PPTAv, *: petrosal vein, white double arrow: auditory nerve).

Preoperative 3D multimodality imaging (A: normal size, B: expansion) and postoperative 3D multimodality imaging (C: normal size, D: expansion) show that the courses of the PPTAv and SCA were changed postoperatively; moreover, the root entry zone of the trigeminal nerve was freed from compression.
The SCA is one of the most frequent vessels responsible for trigeminal neuralgia, as it contributes to 75–80% of cases.1) Other blood vessels known to cause trigeminal neuralgia include the anterior inferior cerebellar artery (AICA) and vertebral artery, as well as (to a lesser extent) the petrosal vein. The PPTA or PPTAv also cause trigeminal neuralgia in rare cases,2–4) with a frequency of approximately 0.6%.5)
The PPTA is an anomaly originating in the carotid artery that passes through Meckel’s cave, isolating the dural foramen and perfusing the posterior fossa;4) its frequency of occurrence is approximately 0.1–0.6%.5–8) The PPTAv is a distinct type of PPTA that directly supplies the cerebellum without basilar artery anastomosis.3) Notably, the PPTAv is also rare; its frequency of occurrence is only 0.18%.7) Both PPTA- and PPTAv-induced types of trigeminal neuralgia are extremely rare; moreover, the PPTAv is more likely to cause trigeminal neuralgia than the PPTA.3,5) As the courses of the PPTA and PPTAv cover an extensive area and their patterns of compression are varied, few reports have described compression of the trigeminal nerve by the PPTA or PPTAv. Some studies have reported compression of the PPTA or PPTAv themselves. Furthermore, the PPTA and PPTAv are reportedly associated with aneurysms;8–10) Ladner11) reported that aneurysms originated from PPTA-induced compression of the trigeminal nerve.
We can recognize the vessels responsible for trigeminal neuralgia by using preoperative MRI.4) A combination of MRI and CISS is especially useful in revealing the point of compression and the vessel responsible. In our case, the CISS image helped us to establish that both the PPTAv and SCA caused trigeminal neuralgia; the former was situated below the trigeminal nerve, while the latter was above the nerve.
In addition, trigeminal neuralgia in our case was caused by multiple vessels. There has been no report regarding the frequency of such cases. However, Morita et al.5) reported that eight cases of trigeminal neuralgia were caused by the PPTA or PPTAv. Three of those eight cases were caused by multiple vessels: one included the PPTAv, AICA, and SCA; another was caused by the PPTAv and SCA; the last case was attributed to the PPTA, AICA, and SCA. Thus, to the best of our knowledge, only Morita et al.’s5) report has described cases with combined involvement of the SCA and rare PPTA or PPTAv in onset of trigeminal neuralgia.
We have described a case of trigeminal neuralgia in which the PPTAv and SCA compressed the trigeminal nerve. The potential rarity and complexity of the causes underlying trigeminal neuralgia thus requires careful preoperative assessment. In our case, we avoided re-operation by careful preoperative assessment, which showed that the PPTAv and SCA were the causes of compression; moreover, we established a surgical plan for craniotomy, which avoided the compressed arteries. Indeed, it was difficult to achieve a good collimation axis with respect to the point of compression by the SCA; however, we selected a related artery, and then incised and peeled surrounding arachnoid near the trigeminal nerve and SCA, to enable decompression. Based on these changes, the pain was relieved; thus, we report this encounter as an instructive case for surgical correction of trigeminal neuralgia.
None.