論文ID: cr.2018-0293
論文ID: cr.2018-0293
A 63-year-old man was admitted in our hospital with the chief complaint of upper limb numbness 3 years after undergoing spinous process-splitting laminoplasty (C3–C7) in another hospital. The hydroxyapatite spacers used for the laminoplasty had dislocated, resulting sensory disorders of the upper extremities. Additionally, loosened hydroxyapatite intraspinous spacers and syringomyelia were confirmed. A revision operation was performed, during which the C5 spacer was observed to have dislodged into the spinal canal, and a dural membrane defect, arachnoid membrane tear, cerebrospinal fluid leakage, and marked adhesion change were observed. The adhesion was exfoliated as far as possible; moreover, to prevent the reflux of syringomyelia, a syrinx-subarachnoid shunt (SS shunt) was placed. Although there was concern of further adhesion by putting foreign matter, SS shunt indwelling was chosen to obtain sure disappearance of syringomyelia. The postoperative course was uneventful. A gradual improvement in the upper limb numbness was observed without a recurrence of syringomyelia at 9 years of follow-up.
Laminoplasty is a commonly used procedure for treating cervical spinal myelopathy, with excellent results reported in many studies.1) However, postoperative complications have been reported, including C5 nerve root palsy and axial pain. Here, we describe a rare case of dural laceration and syringomyelia that occurred secondary to a loosened intraspinous spacer. Although there have been only a few reports of dural injury due to artificial bone,2,3) there have been no reports of dural laceration resulting in the formation of syringomyelia. The postoperative adverse event presented here should be recognized as one of the serious surgery-related complications in cervical laminoplasty.
On August 26, 2008, a 63-year-old man presented to our hospital with syringomyelia at the C5 level, as revealed by magnetic resonance imaging (MRI) 10 days earlier (Fig. 1A). Three years prior to this, the patient had been diagnosed with cervical spondylotic myelopathy at another hospital and underwent spinous process-splitting laminoplasty from C3 to C7 with the placement of hydroxyapatite (HA) intraspinous spacers. Following this procedure, he exhibited a good neurological recovery and was discharged home. One year postoperatively, he suffered from progressive upper limb numbness. Radiographs demonstrated the dislocation of all intraspinous spacers, especially a severe dislocation of the C5 spacer, which had dislodged into the spinal canal as revealed by MRI studies (Fig. 1B). However, no further interventions were performed and only follow-up was performed.

(A) Magnetic resonance imaging scan in August 2007, showing cerebrospinal fluid intensity around the dislocated spacer. (B) All the spacers from the laminoplasty are dislocated, with a severe dislocation of the C5 spacer, which impinged on the spinal cord; syringomyelia appeared. (C) Dislocation of HA spacers can be confirmed in Xp (D) HA spacer sticking to spinal cord is seen in CT myelography.
On presentation at our hospital, the patient exhibited numbness, hyperalgesia, and hyperthermia of both upper limbs, although his motor system functioning was within the normal range. The C5 spacers had dislodged into the spinal canal by Xp, CT Myelogram (Figs. 1C and 1D).
The spacer at C5 had dislodged to the spinal canal (Fig. 2A) and was removed during the operation, revealing a dural membrane defect, an arachnoid membrane tear, and cerebrospinal fluid (CSF) leakage (Fig. 2B). The syringomyelia could be seen through a small hole on the surface of the spinal cord. The membrane around this hole had thickened, with considerable adhesion change. The adhesion was exfoliated as far as possible. However, it could not be determined whether the membrane comprised the arachnoid or pia mater, and no distinct subarachnoid space was identified. Subsequently, a shunt tube (1.4 × 50 mm) was inserted into the syringomyelia via the small hole (Fig. 2D), and the dura defect was repaired by patching it with artificial dura (GORE-TEX). Spacers at levels other than C5 had also been dislodged, but the dural membrane was normal. All spacers except C5 were also removed. The postoperative course was uneventful. The patient’s upper limb numbness gradually improved, and the syringomyelia disappeared by the third month after the revision surgery (Fig. 3A). Although there was a subcutaneous CSF retention, no fluctuation on the skin was observed and only follow-up was performed. During the subsequent 9 years of follow-up, no recurrence of syringomyelia was observed (Fig. 3B).

Intraoperative photographs. (A) The dislocated C5 hydroxyapatite spacer can be seen impinging on the spinal cord. (B) After removing the spacer, dural laceration, granulation, and fistula of the spinal cord (arrow) were observed. (C) The arachnoid surface and cerebrospinal fluid flow were confirmed at levels C5–C7. (D) A syringosubarachnoid shunt tube was inserted into the syringomyelia space.

Postoperative magnetic resonance imaging (MRI) confirming the syringomyelia had disappeared. (A) Follow-up at 3 months. (B) Follow-up at 9 years.
Few studies have described the dislocation of HA spacers after laminoplasty;2,3) however, syringomyelia has not previously been reported in such cases. Kanemura et al.2) reported four cases of spacer dislocations, in which dural laceration and CSF leakage were observed, with subsequent dural repair. Our operative findings were similar to those of this report. Ono et al.3) reported two cases. In the first case, a very small dural laceration, the size of a pinhole, was seen but without CSF leakage. In the second case, both dural laceration and CSF leakage were observed, and a dural repair was performed. The appearance of the lamina suggested that the lamina had been eroded by the HA spacer.
In the present case, T2-weighted MRI scan showed a high-intensity area around the dislodged C5 spacer 2 years prior to the revision procedure, inferring that the damage to the dura and pia mater had already occurred. In our opinion, revision surgery should have been considered at that stage.
Consideration of the Mechanism of HA DislocationDislodging of spacers can occur due to several reasons, such as loosening of the sutures, wearing of the suture thread, and the possibility that the spacers did not appropriately fit the lamina, moving unexpectedly and shaving the lamina. In the previously reported cases, the suture thread had worn out. However, these reports do not describe in detail the type of thread used, describing it only as “nylon.” Monofilament nylon thread is very sensitive to friction; therefore, twisted, thick thread should be used for such procedures. At our institution, we use twisted thick thread for fixing HA spacers. In a case where the thread had not worn out, the spacer could have been dislodged because of inappropriate fitting of the spacer. In our case, all the knots were intact; thus, we suspected that these may have acted as a pivot, leading to repetitive quick movements that resulted in the loosening of the spacer. It is therefore important to select spacers of appropriate length, width, and shape, and to trim the lamina and to alternatively perform laminectomy if performing laminoplasty proves difficult. Five types of HA spacers with various widths have been prepared for use in our institution. All these spacers have brims, which apparently help prevent the rotation of the spacers. In our institute, there has been no case of the dislocation of HA spacer, which is to be removed.
Consideration about Selection of More Proper SurgeryWe believe that the syringomyelia in this case was due to a failure of CSF flow. The arachnoid and dura mater had collapsed with strong adhesion of the surroundings. It was obvious that this site was devoid of the normal CSF flows. Similar events are observed in syringomyelia in Chiari malformation type 1. Unlike diffuse adhesion arachnoiditis caused by trauma and inflammation, we believe that the CSF flow disorder in our case was due to local adhesion and physical compression. Although several mechanisms about the cause of syringomyelia have been thought, “Sucking theory” advocated by Williams4) is the most theoretical and easy to understand. Chang and Nakagawa5,6) reported a more theoretical elucidation using electric circuit model, which is easier to understand the mechanism of syringomyelia (Fig. 4).
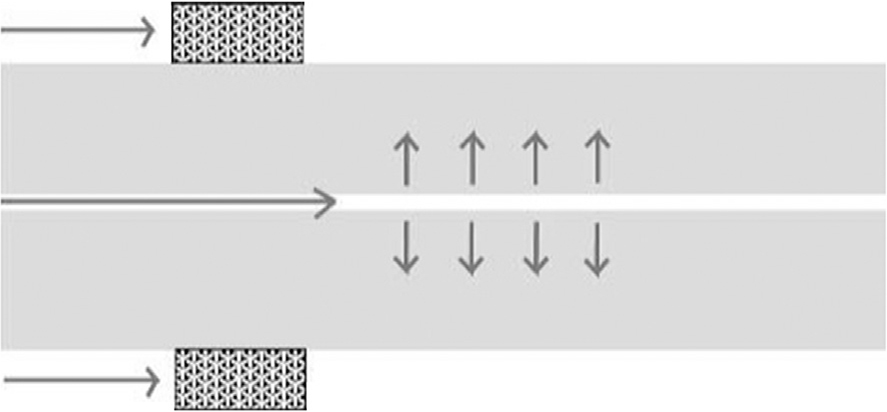
Quotation from Chang and Nakagawa.6) When there is a blockage in the subarachnoid space, the amount of cerebrospinal fluid (CSF) passing through the central canal increases. The CSF in the central canal exceeds a certain amount, and the inside pressure increases. As a result, spinal edema occurs eventually leading to syringomyelia. Arrows show CSF flow.
Syringomyelia gradually should shrink by removing the factor, which inhibits cerebrospinal fluid reflux. However, it is said that there are several recurrences after exfoliating adhesion.7,8) Because there was a partially insufficient exfoliating site in our case, it was not secure to declare whether normal CSF reflux could be obtained and maintained. So insertion of the SS shunt tube was decided through the fistula. There are various reports on the treatment of syringomyelia due to adhesive arachonoiditis, with various opinions. Klekamp et al.9) reported that 61 shunt surgeries without exfoliating adhesion were performed; 40 of them required reoperation within 2 years. On the other hand, in the cases of exfoliating adhesion it is reported that the symptom progression was suppressed in 83%. However, when adhesion range is wide, the performance of operation is poor in either type of surgery (shunt surgery or exfoliating adhesion). Therefore, it is very difficult to decide which surgery is superior. Shikata et al.10) reported cases of shunt surgery (between adhesion site and normal subarachnoid space) in addition to exfoliating adhesion, and posterior fusion surgery was performed; >80% success rate was confirmed in ≥4 years follow-up. Schaan and Jaksche11) reported that arachnoiditis is less likely to occur by performing fusion surgery earlier after a trauma; spinal stabilization also seems to be important.
Kamada et al.12) reported that subarachnoid-pleural (SP) shunt has the highest therapeutic effect. Because there is a pressure difference between the caudal and rostral sides in the case of long syringomyelia, the performance of SP shunt differs depending on the place, where the shunt tube is inserted. Good results were obtained when the shunt was inserted to the caudal side slightly more than the site of maximum diameter. Koyanagi et al.7) reported that SP shunt is an excellent method, but it is presumed that the tube is too long to keep discharging in the low pressure cavity, such as syringomyelia. Therefore, SS shunt dysfunction is said to be less at a site slightly far from adhesion, which is effective in locally suppressing syringomyelia progression. Imae et al.13) reported the usefulness of subarachnoid reconstruction. After inserting SS shunt, the arachnoid and dura are sutured on the upper layer, dural plasty with the artificial dura is performed, and new CSF passageway is formed resulting in the withdrawal of syringomyelia. Our case is similar to this report; it seems that normal CSF reflux obtained by exfoliating adhesion helps to prevent recurrence.
The pathology of syringomyelia due to adhesion arachnoiditis is very complicated, and the appropriate treatment method seems to differ depending on the duration of disease, range of adhesion, size of syringomyelia, etc. In the present case, adhesion existed but remained at a limited site, adhesion of ventral spinal cord did not exist, and the size of syringomyelia remained within two vertebral bodies. Because of these factors, the drainage of SS shunt was considered to be effective in our case.
This case demonstrated a radical cure for a rare complication resulting from spinous process-splitting laminoplasty, which is one of the most basic techniques in cervical spinal surgery. Although it is a relatively easy and versatile method, it is vital that the basic procedures are appropriately performed.
None of the authors have any conflicts of interest to disclose.