2019 Volume 95 Issue 2 Pages 53-66
2019 Volume 95 Issue 2 Pages 53-66
Coronary artery spasm (CAS) plays an important role in the pathogenesis of ischemic heart disease, including angina pectoris, myocardial infarction, and sudden death, occurring most often from midnight to early morning. CAS is prevalent among East Asians and is associated with an aldehyde dehydrogenase 2 (ALDH2)-deficient genotype (ALDH2*2) and alcohol flushing, which is prevalent among East Asians but is virtually non-existent in other populations. ALDH2 eliminates not only acetaldehyde but also other toxic aldehydes from lipid peroxidation and tobacco smoking, thereby protecting tissues and cells from oxidative damage. Risk factors for CAS include smoking and genetic polymorphisms including those of ALDH2*2, endothelial NO synthase, paraoxonase I, and interleukin-6. Accordingly, oxidative stress, endothelial dysfunction, and low-grade chronic inflammation play an important role in the pathogenesis of CAS, leading to increased coronary smooth muscle Ca2+ sensitivity through RhoA/ROCK activation and resultant hypercontraction. Ca-channel blockers blocking the intracellular entry of Ca2+ are specifically effective for treatment for CAS.
Communicated by Hiroo IMURA, M.J.A.
Abbreviations: ACE: angiotensin-converting enzyme; ACh: acetylcholine; ALDH2: aldehyde dehydrogenase 2; ARB: angiotensin II receptor blocker; CAS: coronary artery spasm; CCB: calcium-channel blocker; ECG: electrocardiogram; e-NOS: endothelial nitric oxide synthase; hsCRP: high-sensitivity C-reactive protein; ISDN: isosorbide dinitrate; LDL: low-density lipoprotein; L-NMMA: L-monomethyl-arginine; MI: myocardial infarction; MLC: myosin light chain; MLCK: myosin light chain kinase; MLCP: myosin light chain phosphatase; NO: nitric oxide; NOS: nitric oxide synthase; PCI: percutaneous coronary intervention; ROCK: Rho-associated kinase; ROS: reactive oxygen species.
Angina pectoris is a clinical syndrome caused by transient myocardial ischemia due to an imbalance between myocardial oxygen demand and supply. Classical or effort angina is characterized by: (1) attacks induced by exertion and relieved by rest or nitroglycerin administration, and (2) attacks associated with transient ST segment depression on an electrocardiogram (ECG).1) This form of angina has been well known for more than 200 years since its description by Heberden, and its pathogenesis has been explained by increased myocardial oxygen demand in the presence of fixed organic stenosis of the epicardial coronary arteries. This concept was based on the fact that the majority of patients with angina were found to have severe and extensive atherosclerotic narrowing in their coronary arteries.1) β-adrenergic blocking agents, which reduce myocardial oxygen demand, have been widely used for the treatment of angina. The efficacy of nitroglycerin has been attributed chiefly to its venodilatatory effect, which results in pooling of blood in the venous system leading to decreased myocardial work rather than to its direct effect on the coronary arteries.2)
In 1959, Prinzmetal and colleagues described a new form of angina pectoris that differed sharply from the classical angina and named it a “variant form of angina pectoris”.3) The characteristics of this syndrome were: (1) attacks occurred at rest and were not provoked by exertion, and (2) attacks were associated with ST segment elevation on an ECG. Because the attack occurred at rest and was not induced by exercise, an increase in myocardial oxygen demand could not explain the pathogenesis of this form of angina. They postulated that increased tonus in a vessel with atherosclerotic narrowing might transiently lead to critically diminished blood supply to an area of myocardium.3) However, this syndrome had drawn little attention among cardiologists, probably because attacks were usually not induced by exercise in the daytime, being at odds with the then prevailing concept of increased myocardial oxygen demand in the presence of fixed organic stenosis of coronary arteries as a cause of angina pectoris.1)
In the 1970s, we demonstrated spasm of an epicardial coronary artery or coronary spasm during an attack of variant angina systematically induced by methacholine or exercise in the early morning.4),5) Endo and coworkers reported similar findings almost simultaneously.6) The role of coronary spasm was subsequently extended beyond variant angina to ischemic heart disease in general, including effort angina, unstable angina, acute myocardial infarction (MI), and sudden death.7)–11) Thus, variant angina is now regarded as one aspect of the wide spectrum of myocardial ischemic syndromes caused by coronary spasm, and angina pectoris caused by coronary spasm is called “coronary spastic angina” or “vasospastic angina”.12)–17) We reviewed coronary (artery) spasm previously, and in this article we provide a revised review and updates on our understanding of coronary artery spasm (CAS) based on recent advances in the field.12)–14)
There are insufficient data on the prevalence of CAS in both Eastern and Western countries, probably because it is difficult and cumbersome to examine CAS during coronary angiography. A survey on the prevalence of CAS at multiple institutions in Japan showed that CAS was documented in 921 (40.9%) of the 2251 consecutive patients with angina pectoris who underwent coronary angiography.18) There seems to be a racial difference in the prevalence of CAS between Japanese and Caucasians.19) Recently, however, CAS has been reported less frequently in Japan, probably because calcium-channel blockers (CCBs), very effective drugs for suppression of CAS, are widely used for hypertension as well decreasing rates of smoking.20),21) Increased use of statins, angiotensin-converting enzyme (ACE) inhibitors, or angiotensin II receptor blockers (ARBs) may also have contributed to the reduction in CAS. Many cardiologists consider the provocation test for CAS too cumbersome and time-consuming for a busy cardiac catheterization laboratory and think that a trial with CCBs may be enough for the evaluation of possible spasm.
Common manifestations of myocardial ischemia due to CAS are chest discomfort and ST segment changes on an ECG. Chest discomfort is similar in quality to that of stable effort angina, but is often more severe and prolonged, accompanied by cold sweat, nausea, or vomiting, and sometimes by syncope. It should be noted, however, that myocardial ischemia due to CAS often occurs without accompanying symptoms. Indeed, the incidence of silent myocardial ischemia caused by CAS is more than 2 times higher than that of symptomatic ischemia or angina pectoris (Fig. 1).13),14) The ECG changes that occur during a CAS attack include ST segment elevation and/or depression, peaking and/or increase in the amplitude of the T wave. A negative U wave may also appear at the beginning or near the end of the attack and is often associated with ST segment changes in the anterolateral leads. Total or subtotal occlusion of a major coronary artery by spasm results in ST segment elevation in the leads that represent the area of myocardium supplied by the spasm artery. The ST segment elevation is usually accompanied by reciprocal ST segment depression in the opposite leads. CAS may also cause ST segment depression instead of elevation in the leads that represent the distribution area of the spasm artery. ST segment depression indicates less severe (non-transmural or sub endocardial) myocardial ischemia than ST segment elevation, which represents transmural myocardial ischemia. ST segment depression occurs when: 1) spasm of a major artery is less severe (subtotal and/or diffuse), 2) a major artery receiving collaterals is completely occluded or, 3) a small artery is completely occluded.10) Various forms of arrhythmia often appear during attacks of CAS. These include ventricular arrhythmias such as ventricular premature contractions, ventricular tachycardia, or even ventricular fibrillation, bradyarrhythmias, atrioventricular block, and supraventricular arrhythmias.
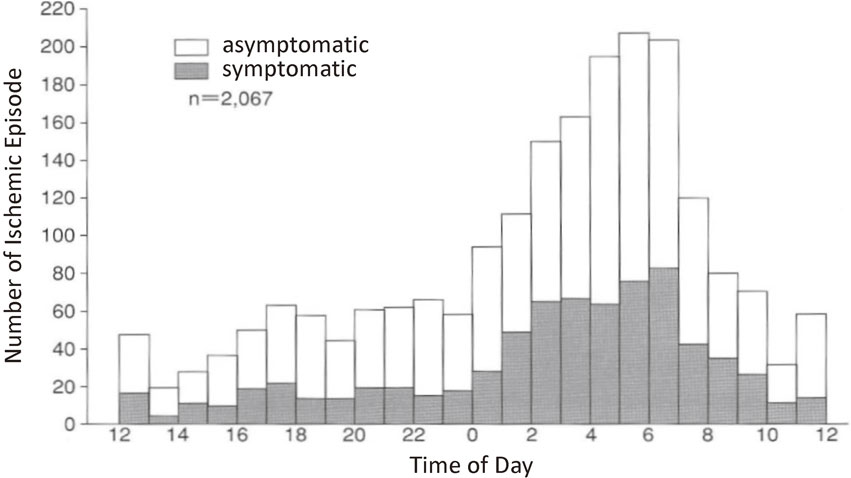
Dirunal distribution of ischemic episodes in patients with variant angina. Attacks occur most often from midnight to early morning. Notably, the number of asymptomatic attacks was larger than that of symptomatic attacks. (From Yasue, H., Kugiyama, K. (1997) Internal Med. 36, 760–765)
CAS had been thought to occur at a site of organic stenosis of a major coronary artery.3) However, CAS appears in angiographically normal arteries as well and often diffusely involves the entire arterial tree (Fig. 2) and may even migrate from site to site.13),14) Spasm preferentially occurs at branch points and at sites different from those of atherosclerotic plaques, which are predominantly localized at non-branch points of the curved proximal segments.22) CAS may thus be a manifestation of a distinct type of coronary disease different from lipid-laden coronary atherosclerosis. Spasm occurs also at two or three arteries at different times or simultaneously in the same patients (multivessel spasm).23),24) Patients with multivessel CAS have the following characteristics: 1) most of them have angiographically normal coronary arteries, 2) they are resistant to treatment, often require larger amounts of CCBs to suppress attacks, and often recur on cessation of the drugs, 3) they are more likely to have lethal arrhythmias such as ventricular tachycardia or ventricular fibrillation and are more likely to suffer from sudden death.13),14)
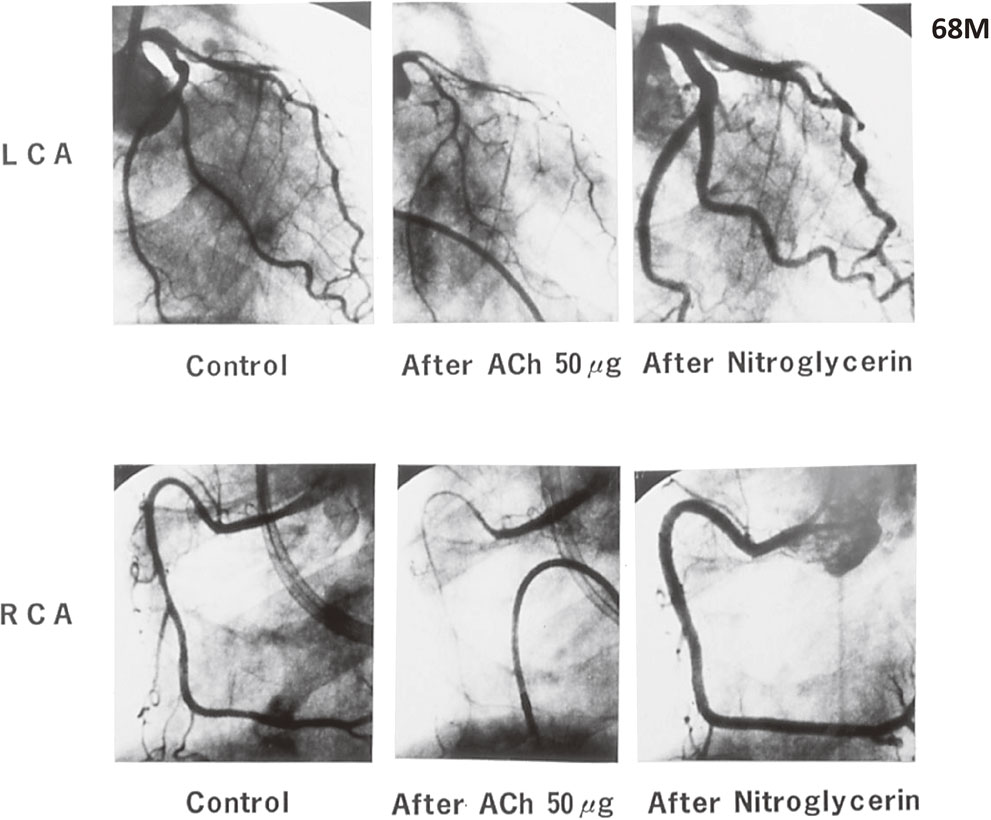
Coronary angiograms in a patient with multivessel CAS. Injection of acetylcholine (ACh) into the left coronary artery (top left) and the right coronary artery (bottom left) induced spasm in each of artery separately. Note that spasm appeared in all 3 major arteries (left anterior descending artery, left circumflex artery, and right coronary artery). Spasm was reversed after intracoronary injection of isosorbide dinitrate (ISDN; top right and bottom right). There was no significant organic stenosis in the arteries. (From Yasue, H. et al. (2008) J. Cardiol. 51, 2–17)
CAS occurs usually at rest, particularly from midnight to early morning (Fig. 1).13),14) Although Prinzmetal and colleagues emphasized that variant angina is not induced by exercise,3) CAS can often be induced even by mild exercise in the early morning but is usually not induced in the afternoon even by strenuous exercise.7)–9) Thus, there is a circadian variation in the exercise capacity of patients with CAS. It is now known that the attacks of all forms of ischemic heart disease including acute MI and sudden death occur most often in the early morning.25) This may be related at least partially to the fact that the tone of an epicardial coronary artery is increased from midnight to early morning, whereas it is decreased in the afternoon. The cause of the circadian variation of CAS remains to be elucidated. Because CAS can be induced by intracoronary injection of acetylcholine (ACh),26) the neurotransmitter of the parasympathetic nervous system, variation in the activity of the autonomic nervous system may be involved in the circadian variation of CAS. CAS can also be induced by stimulation of α-adrenergic receptors.5) Circadian variations in the production of various hormones including catecholamines, cortisol, vasopressin, melatonin, growth hormone, and insulin or inflammatory cytokines including TNF-α or IL-1, may also be related to the circadian variation in CAS.
Precipitating factors.There are several factors that may precipitate CAS. These may be divided into physiological factors and pharmacological agents.
CAS occurs most often at rest, particularly from midnight to early morning. However, in the early morning, even mild exertion may induce CAS.13),14) Physical and/or mental stress, particularly the latter, for several weeks or months may precipitate CAS.27) Exposure to cold,28) Valsalva maneuver, and hyperventilation may also precipitate CAS.29),30) Magnesium deficiency is also associated with CAS.30),31) CAS itself often induces CAS, thus making vicious circle.13),14)
Pharmacological agents include catecholamines (epinephrine, norepinephrine, dopamine, dobutamine), parasympathomimetic agents (ACh, methacholine, pilocarpine), anticholinesterase agents (neostigmine, etc.), ergonovine, serotonin, histamine, β-adrenergic blocking agents, withdrawal from chronic exposure to nitroglycerin, cocaine, smoking, and alcohol.1)–3) Particularly to be noted in daily life is alcohol ingestion. Alcohol drinking after stressful situations often induces CAS, particularly in those with alcohol flushing, usually not immediately but after several hours when blood the levels of alcohol may have disappeared.32),33)
These factors or agents may induce CAS singly. However, when several of these factors are combined, the possibility of occurrence of CAS is high.
The exact mechanisms that underlie CAS remain to be elucidated.
Risk factors.CAS is mostly a disease of middle- and older-aged men and post-menopausal women.1)–3) The disease rarely occurs in young men and pre-menopausal women. Age, low-density lipoprotein (LDL)-cholesterol, hypertension, diabetes mellitus, and smoking are all known to be a significant risk factors for coronary atherosclerosis.34) On the other hand, age, smoking, high-sensitivity C-reactive protein (hsCRP), and remnant lipoproteins are a significant risk factor for CAS.1)–3),35) These facts also suggest that the pathogenesis of CAS may be different from that of coronary atherosclerosis, which is closely related to abnormalities in LDL-cholesterol metabolism. Cigarette smoking is, thus, a crucial environmental risk factor for CAS and may explain the high prevalence of CAS among Japanese smokers. In addition to cigarette smoking and other environmental factors, genetic factors are also involved in the pathogenesis of CAS, as will be described in the next section.
Endothelial dysfunction.The vascular endothelium was once thought of as a simple passive barrier between circulating blood and surrounding tissues. However, evidence indicates that it is a multifunctional organ essential to normal vascular physiology, and its dysfunction can be critical for the pathogenesis of vascular disease.36)
ACh causes vasodilation by releasing nitric oxide (NO) from the endothelium and in humans, intracoronary infusion of ACh induces coronary vasodilation in young healthy subjects, whereas it causes vasoconstriction in patients with coronary atherosclerosis.37)–39) Coronary arteries in patients with coronary spastic angina are highly sensitive to the vasoconstrictor effect of intracoronary injection of ACh, resulting in spasm.40) Intracoronary injection of ACh is thus used as a provocative test for CAS.1)–3) CAS can also be induced by ergonovine, serotonin, or histamine, all of which are endothelium-dependent vasodilators by releasing NO.
On the other hand, nitrates, including nitroglycerin, are endothelium-independent vasodilators and cause vasodilation by being converted into NO in vivo, which stimulates soluble guanylate cyclase, resulting in increased cyclic GMP levels.38) The coronary arteries in patients with CAS are highly sensitive to the vasodilator effect of nitrates.41) Thus, it is possible that the super-sensitivity of spasm arteries to nitroglycerin is due to the deficiency of endogenous NO activity in these arteries. NO is synthesized from L-arginine by NO synthase (NOS), and NO synthesis is specifically blocked by L-monomethyl-arginine (L-NMMA).38) The coronary artery diameter decreases in response to intracoronary infusion of L-NMMA in control subjects, whereas it does not change significantly in patients with CAS.42) These observations indicate that NO is released in the basal state and is involved in the regulation of basal vascular tone in normal humans and that NO activity is deficient in the coronary artery in patients with CAS. There was a significant positive correlation between the response to L-NMMA and that to nitroglycerin, i.e., the smaller the response to L-NMMA, the larger the response to nitroglycerin, indicating that the super-sensitivity to nitroglycerin is related to the deficiency of endogenous NO activity in the coronary artery in patients with CAS.
NO is also known to suppress the production of endothelin 1 and angiotensin II, which are potent vasoconstrictors and proliferators of vascular smooth muscle, and deficiency in NO may enhance the synthesis of these potent vasoconstrictors.43),44) Indeed, intimal thickening and hyperplasia in the coronary arteries are involved in spasm.45),46) CAS rarely occurs in pre-menopausal women except those who smoke1)–3) and estrogens enhance endothelial NO synthase (e-NOS) activity and suppress the attack in post-menopausal women with coronary spastic angina.47),48) Of note, there is a menstrual cyclic variation of the attack in association with changes in the plasma levels of estrogen in pre-menopausal women with CAS.48) Endothelial NO is synthesized by e-NOS, which is constitutively expressed in the endothelium.38) We found polymorphisms of Glu298Asp in exon 7 and T−786 C in the 5′ flanking region of the e-NOS gene are significantly associated with CAS.49),50) Significant associations of e-NOS gene polymorphisms with coronary artery disease have also been reported among both Caucasians and Asians, especially Asians.51) These findings strongly suggest that e-NOS gene polymorphisms compromise endothelial NO production and predispose patients with these alleles to CAS. However, e-NOS polymorphisms are found in only one-third of patients, thus other genes or factors may also be involved in the pathogenesis of CAS, as described in later sections.
Oxidative stress.Reactive oxygen species (ROS) degrade NO and cause vasoconstriction.38) Both basal and ACh-induced endothelial dysfunction in coronary arteries are improved by intracoronary injection of antioxidants such as vitamin C or glutathione in patients with CAS.52)–54) Plasma levels of vitamin E, another antioxidant, are low and those of thioredoxin, a marker of ROS, are high in patients with coronary spastic angina.55)–57) CAS rarely occurs in pre-menopausal women except those who smoke1)–3) and estrogens enhance antioxidant as well as e-NOS activity and suppress attacks in post-menopausal women with coronary spastic angina.47),48) CAS is significantly associated also polymorphism of genes that have an antioxidant effect, including aldehyde dehydrogenase 2 (ALDH2),58) paraoxonase I,59) NADH/NADPH oxidase p22 phox, stromelysin-1, interleukin-6,60) and phospholipase-δ 1,61) and the plasma level of thioredoxin, a marker of oxidative stress, is increased in patients with CAS.57) CAS is more prevalent among smokers, and endothelial function is impaired both in coronary and brachial arteries and is improved by vitamin C infusion in smokers.62),63) Cigarette smoke extracts markedly suppress ACh-induced endothelium-dependent relaxation, and the suppression is prevented by antioxidants in isolated arteries.64) These findings indicate that smoking degrades NO by way of oxygen radicals.
Deficient aldehyde dehydrogenase 2 activity.Oxidative degradation of lipid membrane (lipid peroxidation) generates numerous reactive aldehydes and causes oxidative damage.65),66) ALDH2 activity eliminates not only acetaldehyde but also other toxic aldehydes including 4-hydoxy-2 nonenal from lipid peroxidation or acrolein in tobacco smoke, thereby protecting tissues and cells from oxidative damage.67),68) The deficient variant ALDH2 genotype (ALDH2*2) is prevalent (30–50%) among East Asians, but rare in other populations, and is characteristically associated with alcohol flushing syndrome.68) We have shown recently that ALDH2*2 is an important risk factor for CAS (Fig. 3)58) and that the combination of tobacco smoking and ALDH2*2 synergistically amplifies the risk of CAS.59),69),70) We have thus identified deficient ALDH2 activity, and hence reactive aldehydes and ROS, as risk factors for CAS. Indeed, CAS patients have increased ROS levels and are liable to acute MI, and ALDH2*2 is also a significant risk factor for MI.70) Takeuchi and coworkers recently identified the genetic locus of ALDH2*2 (rs671) as the strongest predictor of MI in a genome-wide association study in Japanese patients.71) There are also increasing numbers of studies showing the association of ALDH2*2 with coronary artery disease and MI both in China and Korea.72) ALDH2 also plays an essential role in the bioactivation of nitroglycerin widely used for the treatment of ischemic heart disease.73) However, continued administration of nitroglycerin leads to tolerance or even cardiac events through the inactivation of ALDH2 and increased ROS levels.68),73) Accordingly, carriers of ALDH2*2 genotypes are less responsive to nitroglycerin and are more susceptible to nitroglycerin tolerance and ROS. Deficient ALDH2 activity and hence increased reactive aldehyde are identified as a causative risk factor to be targeted for the treatment of CAS. High prevalence of ALDH2*2 and smoking rate may explain at least partially why CAS is prevalent among East Asians compared with Westerners.19),58)
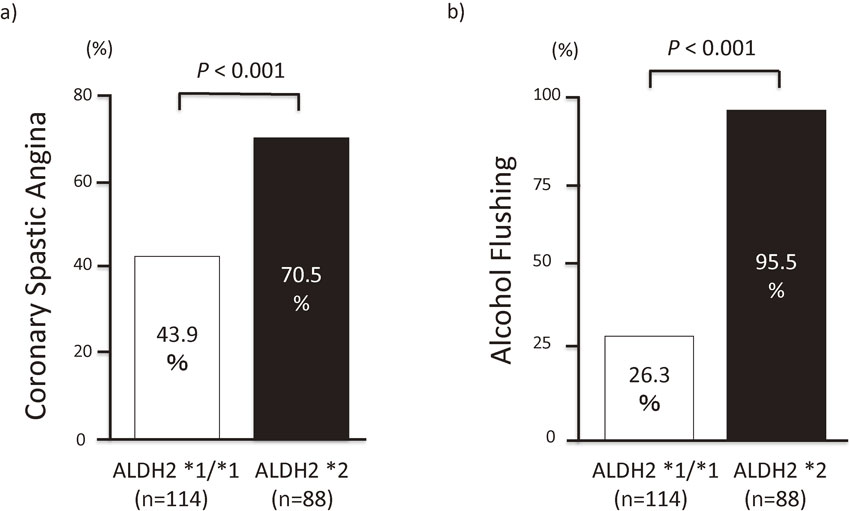
Comparison of the frequency of coronary spastic angina (CSA) and alcohol flushing syndrome by ALDH2 genotype group. The frequencies of CSA (a) and alcohol flushing response (b) were both significantly higher in the variant genotype ALDH2*2 group compared with the wild-type genotype ALDH2*1/*1 group. ALDH2 indicates aldehyde dehydrogenase 2. (From Mizuno, Y. et al. (2015) Circulation 131, 1665–1673)
Shimokawa and co-workers have developed a swine model of CAS by chronically applying interleukin-β to the coronary artery of animals.74) Adhesion molecules such as P-selection are increased in the coronary artery involved in spasm.75) Plasma levels of hsCRP, a sensitive marker of inflammation, are also increased in patients with CAS compared with those of non-CAS patients.76) Chronic tobacco smoking, the number one risk factor for CAS, is also associated with chronic low-grade inflammation.77) These findings indicate that chronic low-grade inflammation plays an important role in the pathogenesis of CAS. A recent study reported that coronary adventitial and perivascular adipose tissue also are involved in inflammation of CAS.78)
Hypercontractility of coronary smooth muscle.Contraction and relaxation of vascular smooth muscle are regulated by myosin light chain (MLC) kinase (MLCK) and myosin light chain phosphatase (MLCP) through phosphorylation and dephosphorylation of MLC.79) The classical pathway through which contracting stimuli induce MLC phosphorylation is an increase of the free intracellular Ca2+ concentration. The complex of Ca2+ and calmodulin then activates MLCK, leading to increased MLC phosphorylation. CAS may be regarded as hypercontraction of coronary smooth muscle triggered by an increase of intracellular Ca2+, and CCBs, which block the entry of Ca2+ into cells, are highly effective in suppressing CAS.12)–16)
It has shown recently that Ca2+-independent regulation also occurs through the inhibition of MLCP and that the level of MLC phosphorylation is determined by a balance between MLC phosphorylation and dephosphorylation. Accumulating evidence indicates that small GTPase RhoA and its downstream effector, ROCK/Rho-kinase, inhibit MLCP, leading to augmentation of MLC phosphorylation and Ca2+ sensitization in response to vasoconstrictor stimuli.80),81) Shimokawa and colleagues showed that ROCK activity was enhanced in smooth muscles of the coronary artery involved in spasm, and specific inhibitors of ROCK relieved CAS.82),83) Statins, which block the RhoA/ROCK pathway and increase endothelial NO84),85) also suppress CAS.86) It is thus quite probable that enhanced Ca2+ sensitization via increased Rho/ROCK activity as well as increased intracellular Ca2+ may play a critical role in the genesis of CAS. Decreased endothelial NO activity also has been shown to enhance Rho/ROCK activity in the coronary arteries.84),85),87) Enhanced phospholipase C activity may also be involved in CAS through enhanced contraction of vascular smooth muscle cells.61)
Magnesium.Magnesium is said to be an endogenous calcium antagonist, and infusion of magnesium suppresses hyperventilation-induced attacks in patients with CAS.30) There is magnesium deficiency in 45% of the patients with variant angina, and magnesium deficiency may be related to the genesis of CAS in some of the patients.31),33)
CAS and atherosclerosis.Impairment of endothelial function also plays a central role in the initiation and progression of coronary atherosclerosis.34) However, the relationship between the two disease conditions remains to be elucidated. In our study, the predictors for CAS were being male, smoking, low diastolic blood pressure, and hsCRP, whereas those for atherosclerosis were age, diabetes mellitus, low levels of high-density lipoprotein-cholesterol, systolic hypertension, uric acid, and being male in that order.35) This finding may suggest that CAS may precede and contribute to the progression of atherosclerotic stenosis. However, the prevalence of CAS declines, whereas that of atherosclerotic stenosis increases with age in the older group. Coronary atherosclerotic stenosis, therefore, may rather restrain CAS, although the two conditions often coexist. CAS appears in angiographically normal arteries as well as atherosclerotic arteries and often diffusely involves the entire arterial tree and may even migrate from site to site.13),14) Spasm preferentially occurs at branch points and at sites different from those of atherosclerotic plaque, whereas atherosclerotic lesions are predominantly localized at non-branch points of the curved proximal segments, as describe previously.22) CAS may thus be a manifestation of a distinct type of coronary disease different from the lipid-laden coronary atherosclerosis. Recent studies show that percutaneous coronary intervention (PCI) with stenting for atherosclerotic stenosis does not influence the recurrence of CAS and that spasm often occurs diffusely in the distal segments of the stented lesion.88)–90)
CAS and coronary thrombosis.Coronary thrombosis is now known to be the cause of acute coronary syndromes including acute MI, unstable angina and ischemic sudden death.91),92) CAS may also be involved in the pathogenesis of acute coronary syndromes including acute MI.13)–16) Plasma levels of fibrinopeptide A, a marker of thrombin generation, are increased after attacks of CAS, and there is a circadian variation in the levels in parallel with that of CAS attacks.93),94) Plasma levels of plasminogen activator inhibitor 1 also show a circadian variation in parallel with that of the attacks of CAS.95) Platelets are activated after attacks of CAS but not after those of stable effort angina.96) These findings indicate that CAS can trigger coronary thrombosis and may play an important role in the pathogenesis of acute coronary syndromes including acute MI. Indeed, coronary thrombosis has been demonstrated by angioscopy in patients with CAS.97)
Attacks of CAS can usually be promptly relieved by sublingual administration or oral spray of nitroglycerin or isosorbide dinitrate (ISDN). In refractory spasm, intravenous or intracoronary injection of the drugs may be necessary. Nitrates are converted in vivo to NO, and the administration of nitrates may be regarded to be a replacement therapy for deficiency of endogenous endothelial NO in patients with CAS. Indeed, coronary arteries involved in spasm are highly sensitive to nitrates.
Prevention.Though the sublingual administration of nitroglycerin or ISDN rapidly relieves the attack, the duration of actions of these drugs is short and less than an hour. For the prevention of attacks, long-acting drugs are needed, and CCBs are very effective for this purpose. CCBs inhibit the inflow of Ca2+ into the smooth muscle cells through voltage-sensitive Ca2+ channels, thereby causing vasodilation.
Notably, the timing of administration of these drugs is very important because attacks of CAS usually occur at rest from midnight to early morning. These drugs should be given before going to bed at night. Doses should also be gradually increased in the individual patient, paying due attention to the side effects. In patients with multivessel CAS, CCBs should not be withdrawn even if symptomatic attacks occur rarely because silent myocardial ischemia often occurs, and there is a danger of sudden death from lethal arrhythmias in these patients.
Statins increase endothelial NO activity, decrease ROS, and suppress the RhoA/ROCK pathway.84),85),87) We and others have shown that statins suppress CAS and improve its prognosis and we recommend statins for the treatment of CAS.86),98)
Long-acting nitrates (oral or transdermal) have been used for preventing CAS.16) However, chronic administration of organic nitrates leads to increased ROSs, endothelial dysfunction, and nitrate tolerance and may thereby increase cardiac events including CAS,99)–101) particularly in those with ALDH2*2. Accordingly, intermittent therapy with a nitrate-free window of at least 8 hours added on CCBs, and/or cotreatment with direct and indirect antioxidants such as statins,84),86),98) ACE-inhibitors, ARBs,102),103) vitamin C and E,52)–56) hydralazine, and estrogen in postmenopausal women,47) all of which suppress nitrate tolerance and endothelial dysfunction, are recommended. Nicorandil, (a nitrate and K-channel activator)104) and pioglitazone (a peroxisome proliferator-activated receptor γ agonist)105),106) are also effective in suppressing CAS. For refractory CAS, larger doses and combinations of different classes of CCBs or together with statins, ACE-inhibitors, ARBs, antioxidants such as vitamin C and E, or estrogen in postmenopausal women may also be necessary. Because contraction of vascular smooth muscle is under the dual control of intracellular Ca2+ and RhoA/ROCK activity, inhibitors of the RhoA/ROCK pathway may also prove useful for the treatment of CAS.82),83)
General measures.Because patients with CAS have endothelial dysfunction, the elimination or control of the factors that may impair endothelial function or increase oxidative stress, particularly smoking, is very important. Drinking alcohol may induce attacks of CAS usually not immediately but several hours after drinking, particularly in susceptible patients with the deficient ALDH2*2 genotype.58) Sudden exercise may also induce the attacks in the early morning. However, mild to moderate aerobic exercise in the afternoon suppresses CAS by increasing endothelial NO activity and should be strongly recommended.107) Emotional stress is a very important substratum for the attacks and anger or fear may induce the attacks. Hyperventilation and exposure to cold may also precipitate an attack. Magnesium, which is an endogenous calcium antagonist, must be supplied in the patients deficient in this element. Drugs that may induce CAS must be avoided. Such drugs include catecholamines, muscarinic agonists, ergot alkaloids, prostaglandins, alcohol, and β-blockers. In postmenopausal women with refractory CAS, estrogen replacement therapy may be useful.47),48)
Prognosis.There are seasonal or monthly as well as circadian variations in episodes of CAS, depending on precipitating or environmental factors. Long-term survival is usually good so long as patients are on CCBs and abstain from smoking.108) The predictors for prognosis are the number of coronary arteries with significant organic stenosis, medication with CCBs, and multivessel spasm.108) In many patients, attacks tends to diminish with time after the few months of recurrent attacks. There is still no definite answer as to how long the administration of Ca antagonists should be continued. It is our opinion that patients with multivessel spasm should be on CCBs indefinitely because these patients often have lethal arrhythmias (ventricular tachycardia, ventricular fibrillation, high-degree AV block, or asystole) and are at higher risk of sudden death, even though they may be asymptomatic.109),110) They should be watched closely and followed by a knowledgeable physician.
The incidence of CAS seems to be decreasing, probably because of the widespread use of medications such as CCBs, statins, ACE-inhibitors, or ARBs for cardiovascular disease. Decreases in smoking habits also may have contributed to the reduced prevalence of CAS. Many cardiologists, particularly the younger ones, now tend to be more interested in PCI and pay less attention to CAS. Multi-detector computed tomography scanning is increasingly being applied for the evaluation of coronary heart disease in place of coronary angiography. In these circumstances, it is possible that there will be fewer and fewer cardiologists who are familiar with CAS in the future. Because there are many patients with CAS who are refractory to conventional medications and may suffer from lethal arrhythmias or sudden death, and because PCI is not the right answer for CAS,61),87),88) it is very important for every clinician to be alert to the presence of CAS, which may be silent and lethal. Further studies are required to elucidate the pathogenesis of this intriguing disease and develop more effective and disease-modifying drugs for its treatment.
We appreciate the secretarial assistance of Ms. Oda A. in the preparation of the manuscript.

Hirofumi Yasue was born in 1934 in Kagoshima Prefecture and graduated from Kyoto University School of Medicine in 1959. After an internship, he majored in internal medicine, specifically endocrinology and hypertension. He received his Ph.D. degree from Kyoto University School of Medicine in 1968. He worked as a research fellow at Cedars-Sinai Medical Center affiliated with University of California at Los Angeles from 1968 to 1969. He then worked as a chief of internal medicine at Shizuoka City Hospital from 1969 to 1983. Angina pectoris had been regarded as being caused by increased myocardial oxygen demand in the presence of fixed organic stenosis of coronary arteries, and β-blockers, which decrease myocardial oxygen demand, were recommended as the mainstay for the treatment of angina pectoris until the 1970’s. In the early 1970’s, he and co- workers demonstrated for the first time that coronary spasm is the cause of resting angina pectoris by systematically inducing the attack by the injection of methacholine or exercise stress in the early morning.
His group further showed that the newly introduced calcium-channel blockers suppressed coronary spasm specifically, whereas β-blockers aggravated it.
Coronary spasm is now established to play an important role in the pathogenesis of ischemic heart disease in general, including rest angina, exertional angina, silent myocardial ischemia, acute myocardial infarction (AMI) and sudden cardiac death.
He became Professor of Cardiovascular Medicine at Kumamoto University in 1983 and established the intracoronary injection of acetylcholine as the standard test for the diagnosis of coronary spasm, which is prevalent among East Asians. He retired from Kumamoto University in 2000 and is currently the director of Kumamoto Aging Research Institute. Recently, he and his coworkers revealed that a deficient variant of the aldehyde dehydrogenase 2 (ALDH2) gene, which is prevalent among East Asians, is causally associated with coronary spasm and AMI. They thus identified toxic aldehydes derived from lipid peroxidation or tobacco smoking to be intervened for the treatment and prevention of coronary spasm and AMI. For his accomplishments, he received Takeda Medical Award, Jokichi Takamine Memorial Award, and Honorable Award from the Japanese College of Cardiology.