2017 Volume 2 Article ID: 20170006
2017 Volume 2 Article ID: 20170006
Objective: We retrospectively investigated the preoperative and postoperative sports and physical activities (SPA) of elderly patients with medial compartment knee osteoarthritis who underwent opening-wedge high tibial osteotomy (OWHTO). Methods: Fifty-six patients (62 knees) with medial compartment knee osteoarthritis were included in the study. The patients comprised 45 women and 11 men with a mean age at surgery of 71.6 years (range, 65–81 years). The mean follow-up period was 51±7 months. Patients who performed SPA to maintain their health for at least 30 min per session more than once a week were defined as SPA cases. The preoperative and postoperative ratios of SPA cases, the time to resuming or starting postoperative SPA, and the frequency of performing postoperative SPA were investigated. Clinical results were assessed using the Lysholm score. Results: Fifteen patients (26.7%) performed SPA before OWHTO and 14 (25.0%) performed SPA after OWHTO (P=0.21). The mean time to resuming or starting SPA after surgery was 14.1±10.0 months, and the frequency of postoperative SPA sessions was 4.2±2.1 per week. The mean Lysholm score significantly improved from 60.8±8.9 preoperatively to 92.5±2.5 postoperatively (P<0.0001). Conclusion: The ratio of patients who performed SPA after OWHTO was still <30% , and it took a comparatively long time for patients to resume or start SPA after surgery.
Knee osteoarthritis (OA) is a frequently disabling health condition in adults and is costly in terms of healthcare resources. Opening-wedge high tibial osteotomy (OWHTO) is a surgical procedure used to treat relatively early-stage medial compartment knee OA.1,2) By changing the axis of the lower limb using an extra-articular approach, OWHTO preserves the native articular surface and decreases the excess stress in the medial compartment of the knee.3,4,5) After OWHTO, patients generally have no limits on their activities of daily living. Excellent clinical results of OWHTO have been reported.1,2,3,4,5) However, the activities performed by patients with knee OA before and after osteotomy have rarely been described. The sports and physical activities (SPA) performed by patients with knee OA before and after valgus knee osteotomy have been investigated and several reports have been published.6,7,8) These studies involved patients with a wide range of ages and included younger patients who resumed high-impact sports such as tennis and rugby postoperatively.
Differences exist in the physical abilities and lifestyles of younger versus elderly people. Elderly people experience a decline in mobility, which can cause sarcopenia and frailty.9,10,11,12) Moreover, elderly patients with gait disorders such as knee OA are thought to be at higher risk of lifestyle-related diseases and disuse syndrome. Aerobic and muscle-strengthening exercises have been recommended for elderly people. Knee OA and other conditions, however, may impede aerobic exercise. Improvement in the knee function and the amelioration of pain of elderly patients with knee OA can create opportunities for increased activities and therefore offer the potential to prevent various diseases postoperatively. Many people in Japan retire at 65 years of age. Consequently, people aged >65 years have adequate time to enjoy various health-promoting activities, including SPA. SPA performed by elderly patients before and after OWHTO have not been reported. We retrospectively investigated the preoperative and postoperative SPA of elderly patients aged >65 years with medial compartment knee OA who underwent OWHTO. The excess stress in the medial compartment of the knees and knee pain significantly would decrease after OWHTO. We considered that the amount and variety of SPA performed by elderly patients might improve postoperatively.
Fifty-six patients (62 knees) with medial compartment knee OA were investigated. The patients comprised 45 women and 11 men with a mean age at surgery of 71.6 years (range, 65–81 years). The mean follow-up period was 51±7 months. The correction angle was planned to produce a lower-limb mechanical axis passing through approximately 70% of the width of the tibial articular surface from its medial margin on anteroposterior full-length radiographs of the lower limbs in the supine position. All surgical procedures were performed by the method employed by Lobenhoffer and Agneskirchner.13) The superficial medial collateral ligament and pes anserinus were dissected from the medial cortex of the tibia, and an osteotomy was performed. Lower limb alignment was confirmed under an image intensifier during the operation. Beta-tricalcium phosphate blocks were inserted into the osteotomy gap, and the osteotomy site was fixed using a locking compression plate. The average preoperative and postoperative lower limb alignments were evaluated by the femorotibial angle (FTA) and the passing point of the lower-limb mechanical axis on the tibial plateau (%MA: the medial margin of the tibial plateau is defined as 0% and the lateral margin is defined as 100%) on anteroposterior full-length radiographs of the lower limbs while weight bearing.
Muscle strengthening exercises and range-of-motion exercises were started 1 day after surgery. Partial weight bearing was permitted from 1 week after surgery, and full weight bearing was permitted from 4 weeks after surgery. Partial weight bearing was, however, not permitted until 3 weeks after surgery in patients with microfractures.14,15) SPA were generally permitted after the patients were able to go smoothly up and down stairs without postoperative knee pain.
The preoperative FTA and %MA were 181.8°±6.3° and 18.6%±12.7%, respectively, whereas the average postoperative FTA and %MA were 170.9°±3.2° and 64.0%±9.8%, respectively.
Fifteen patients (26.7%) performed SPA before OWHTO, whereas 14 (25.0%) performed SPA after OWHTO. There was no significant difference between the preoperative and postoperative numbers of patients performing SPA (P=0.21). The types of preoperative and postoperative SPA are shown in Table 1. One patient participated in three activities preoperatively and the other 14 patients participated in one activity. Postoperatively, nine patients performed two or three activities. Three of the 15 patients who performed SPA before OWHTO resumed the same type of SPA postoperatively. Two of the 15 patients quit performing SPA altogether; their preoperative SPA had been softball and tennis, respectively. Two other patients changed the type of SPA postoperatively. The remaining eight patients were able to perform other types of SPA postoperatively in addition to their preoperative SPA. Three patients who did not perform SPA preoperatively started performing SPA postoperatively. Overall, 11 (19.6%) patients were able to improve the amount of SPA performed postoperatively. In the 14 patients performing SPA postoperatively, the mean time to resuming or starting SPA after surgery was 14.1±10.0 months, and the frequency of activities postoperatively was 4.2±2.1 per week. The mean Lysholm score significantly improved from 60.8±8.9 preoperatively to 92.5±2.5 postoperatively (P<0.0001) (Fig. 1).
| Before OWHTO* | After OWHTO** |
|---|---|
| Walking (5) | Walking (11) |
| Swimming (4) | Swimming (9) |
| Golf (1) | Golf (2) |
| Tai chi (1) | Tai chi (1) |
| Japanese archery (1) | Japanese archery (1) |
| Trekking (1) | Trekking (2) |
| Cycling (1) | Sports gym*** (1) |
| Table tennis (1) | Social dancing (1) |
| Tennis (1) | Gardening (1) |
| Softball (1) |
*One patient participated in three activities before OWHTO.
**Nine patients participated in two or three activities after OWHTO.
***The term "sports gym" refers to moderate exercise at a workout gym.
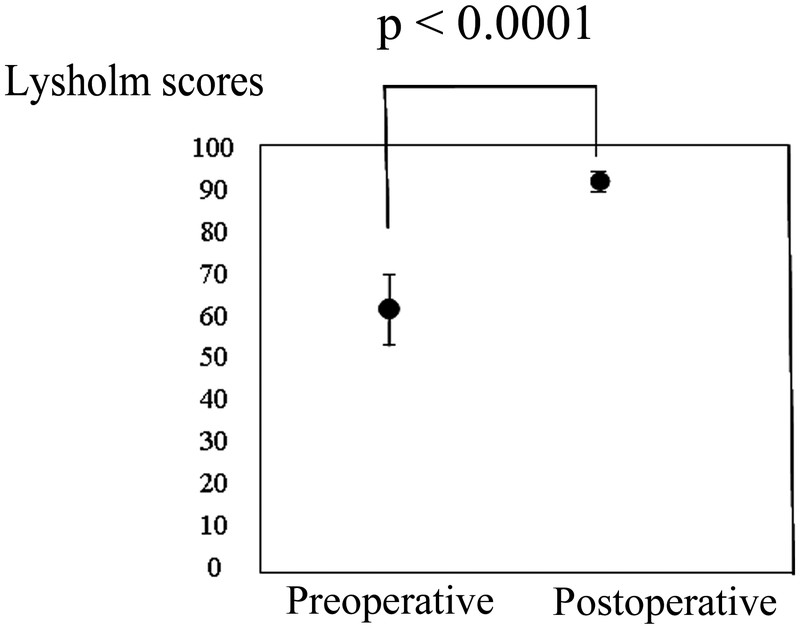
Lysholm scores. The mean Lysholm score significantly improved from 60.8±8.9 preoperatively to 92.5±2.5 postoperatively (P<0.0001).
A 72-year-old woman developed right knee pain without a trigger and eventually had difficulty walking. She was diagnosed with Kellgren–Lawrence grade III OA in her right knee (Fig. 2). Arthroscopy before OWHTO revealed cartilage wear on the medial femoral condyle and surface of the tibia on the opposite site and exposure of subchondral bone (Fig. 3). OWHTO was performed. The preoperative FTA and %MA were 180° and 24.3%, respectively, whereas the postoperative FTA and %MA were 170° and 60.0%, respectively (Figs. 2 and 4). The preoperative Lysholm score was 65 points and the 2-year postoperative Lysholm score had improved to 89 points. Preoperatively, the patient enjoyed table tennis twice a week, whereas she enjoyed ground golf (a recreational sport for elderly people similar to golf) twice a week postoperatively.
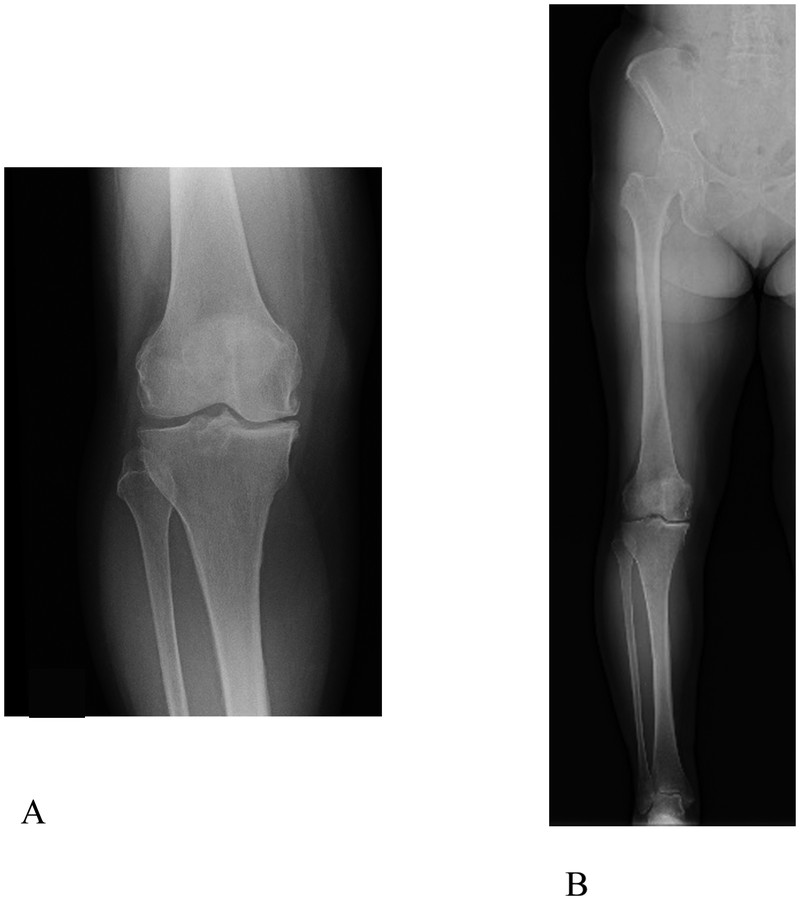
Preoperative radiographs of a 72-year-old woman with OA of the right knee. (A) The OA was determined to be Kellgren–Lawrence grade III. (B) The preoperative FTA and %MA were 180° and 24.3%, respectively.
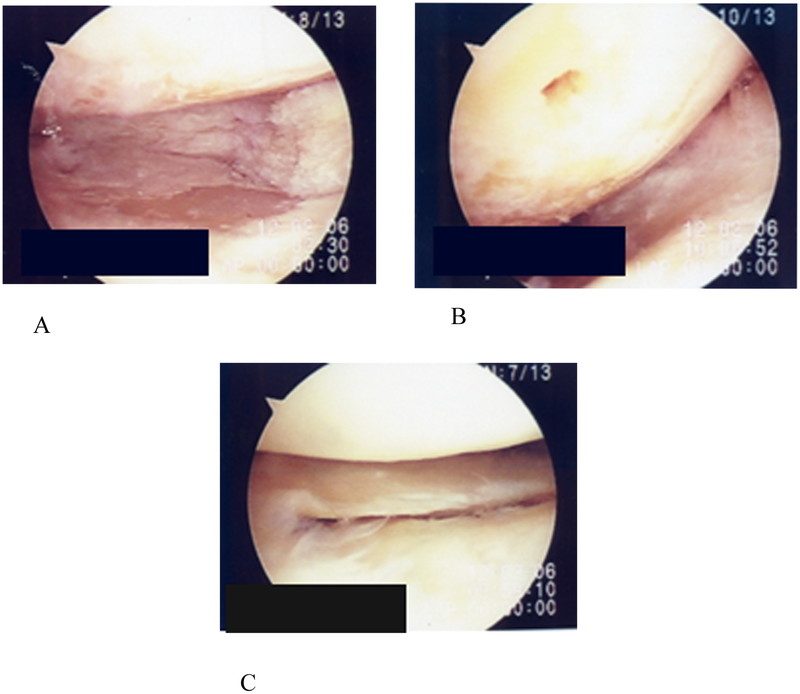
Arthroscopic findings at the time of the operation. (A) The cartilage on the medial femoral condyle and surface of the tibia on the opposite site was worn and the subchondral bone was exposed. Debridement was performed. (B) Microfracture was performed in the medial compartment under arthroscopy. (C) The lateral compartment was almost normal.

Postoperative radiographs of a 72-year-old woman with OA of the right knee. (A) Anteroposterior radiograph of the right knee 4 weeks after OWHTO. Beta-tricalcium phosphate blocks were inserted into the osteotomy gap, and the osteotomy site was fixed using a locking compression plate. (B) The postoperative FTA and %MA were 170° and 60%, respectively, at the latest follow-up.
In this study, we investigated the preoperative and postoperative SPA of elderly patients aged >65 years with medial compartment knee OA who underwent OWHTO. In Japan, people generally retire from work at the age of 65 years. Some people’s work involves heavy labor, and not all people aged <65 years who perform heavy labor have a habit of also performing SPA. Accurate evaluation of the postoperative improvements in the activities of patients aged <65 years cannot be achieved by investigating SPA only: the types and quality of labor also require consideration. Most patients in this study had retired from work; additionally, none of the patients had performed heavy labor. Evaluation of changes in activities other than SPA was not possible in our study. However, the patients who did not regularly perform SPA in their daily life postoperatively likely experienced improvements in activities such as stair climbing because of the improvements in their Lysholm scores. Research on patients’ actual preoperative and postoperative lifestyles or physical abilities is needed in a format other than a question-based study.
The lower limb alignment in our patients was considered to be sufficiently corrected after OWHTO because our results were comparable with those of previous reports.5,16) Our hypothesis was that the amount of SPA performed by elderly patients might improve after OWHTO. However, the improvement ratio of SPA was 19.6% (<20%). The number of patients with medial compartment knee OA who performed SPA after OWHTO was not significantly higher than that before surgery in this study. Thirteen patients continued SPA preoperatively and postoperatively in some way, and some of these patients performed two or three activities postoperatively.
Faschingbauer et al.8) reported that patients with an average age of 42 and the highest work intensity returned to work 19.1±9.1 weeks after OWHTO. In the present study, the average time until resuming or starting SPA after surgery was more than 1 year. It took our patients a comparatively long time to resume or start SPA postoperatively, although there were differences in the work-related and non-work-related activities between our patients and those of Faschingbauer et al. This long delay may have caused our patients’ difficulty in resuming or starting SPA postoperatively. Advancing age during the rehabilitation period might influence whether these elderly patients want to resume or start SPA. Patients might either have no established aims or even forget their aims of OWHTO and rehabilitation. After OWHTO, two patients in our study quit performing their preoperative SPA of softball and tennis. These activities are high-demand sports that are difficult to resume after OWHTO. These two patients did not perform other SPA postoperatively. Postoperative residual pain and loss of muscle strength might be a larger burden to these patients than previously considered.6) Takeuchi et al.17) reported that early weight-bearing exercises enabled full weight bearing at 2 weeks after OWHTO. Accelerating the start of walking postoperatively could help to maintain patients’ motivation for rehabilitation and resuming SPA. However, detailed studies of treatment after OWHTO for elderly patients are needed from viewpoints other than orthopedic surgery.
The duration and frequency of SPA when performed for health improvement should be either more than 20 min per session more than three times a week or more than 30 min intermittently almost every day.18,19) The exercise intensity should be minimal in consideration of each patient’s exercise capability at the beginning. The exercise regimen should be designed for the long term, preventing patients from growing tired of performing SPA. Additionally, rehabilitation programs for elderly patients should be based on the physiological and psychological changes associated with aging. However, application of these recommendations to elderly patients performing SPA might be difficult because many of them have various chronic diseases in addition to the above-mentioned changes. Instead, elderly patients could be advised to perform SPA based on their subjective complaints, including pain, respiratory discomfort, and palpitation. An established protocol for smoother performance of SPA after OWHTO is needed.
The proportion of elderly patients with medial compartment knee OA who performed SPA after OWHTO was still <30%, which was unchanged from the preoperative value. Moreover, it took a relatively long time for patients to resume or start SPA after surgery.
The authors declare that there are no conflicts of interest.