2018 Volume 3 Article ID: 20180017
2018 Volume 3 Article ID: 20180017
Objective: We set out to examine the effectiveness of early rehabilitation for maintaining mobility status during hospitalization in elderly patients with heart failure. Methods: Using the Japanese Diagnosis Procedure Combination inpatient database, we retrospectively examined the eligibility of 527,440 consecutive patients aged ≥60 years who were diagnosed with heart failure with New York Heart Association class ≥ II at admission between July 2010 and March 2014. Of the 146,735 eligible subjects, 39,357 underwent early rehabilitation and 107,378 underwent non-early rehabilitation. Early rehabilitation was defined as rehabilitation starting within 3 days after admission. A multivariable logistic regression analysis and an instrumental variable analysis were carried out to examine the association of early rehabilitation with changes in mobility status during hospitalization. Results: The proportion of heart failure patients with maintained or improved mobility status during hospitalization was higher in the early rehabilitation group. Multivariable logistic regression analysis revealed that the early rehabilitation group had a significantly higher proportion with maintained or improved mobility status (odds ratio, 1.32; 95% confidence interval, 1.21–1.43; P<0.001). The instrumental variable analysis showed that early rehabilitation was associated with an increased proportion of patients with maintained or improved mobility status (risk difference, 0.8%; 95% confidence interval, 0.4%–1.1%; P<0.001). Conclusions: The present study suggests that early rehabilitation is associated with an increase in the proportion of patients with maintained or improved mobility status compared with non-early rehabilitation in elderly inpatients with heart failure.
Heart failure (HF) patients are commonly frail, and HF is associated with adverse health outcomes.1,2,3,4,5,6) Because there is no gold standard diagnosis for frailty, frailty within the HF population1) was defined as patients meeting three of the following five phenotypic criteria for compromised ability to address stressors7): unintentional weight loss, exhaustion, weakness, low physical activity, and slow walking speed. Transitions between frailty states (non-frail, pre-frail, and frail) are not irreversible,8,9) and interventions that prevent the inability to perform essential activities, such as walking at home without assistance, constitute an important therapeutic strategy.
Previous studies showed that immobilization of elderly patients during hospitalization after a cardiac event led not only to multiple complications,10) but also to the development of disability.11) Other studies showed that the loss of muscle mass through immobilization was associated with decreased functional ability within 2 days of hospitalization,12) and with higher risks of morbidity, higher hospital readmission rates, and prolonged periods of physical therapy after hospitalization.13) Therefore, early ambulation within the first 3 days of hospitalization, along with careful planning, a suitable workload, and monitoring, has been recommended to enable inpatients to achieve appropriate levels of activity as outpatients.14,15)
Previous studies of cardiovascular rehabilitation have provided long-term evidence that comprehensive programs reduced mortality,16) reduced HF-related hospital admissions,17) improved patient quality of life,17) and improved self-reported health status.18) However, the short-term effectiveness of early rehabilitation on mobility status, such as walking ability, in elderly inpatients with HF remains to be elucidated.
The purpose of the present retrospective cohort study was to examine, using a national inpatient database in Japan, the association (with adjustment for multiple factors) of early rehabilitation with changes in mobility status during hospitalization among elderly patients.
The Japanese Diagnosis Procedure Combination database is a national acute-care inpatient database. The database includes administrative claims data and some detailed clinical data for approximately 7 million inpatients per year (representing approximately 50% of all acute-care inpatients in Japan) in more than 1,000 participating hospitals. All 82 academic hospitals are obliged to participate in the database, whereas community hospitals participate on a voluntary basis. For all patients, the main diagnosis, the comorbidities present at admission, and the complications occurring during hospitalization are coded using International Classification of Diseases and Related Health Problems 10th Revision (ICD-10) codes and text data in Japanese. The database also includes each hospital’s unique identifier and the following patient details: age; sex; medical procedures, including types of surgery coded with original Japanese codes; daily records of drug administration and devices used; New York Heart Association (NYHA) Functional Classification at admission; activity of daily living scores (including mobility status) at admission and discharge; and the discharge status. The discharge status has three categories: discharged to home; discharged to somewhere other than home; and in-hospital death. The database also includes the dates of the start and cessation of rehabilitation.
In Japan, hospitals authorized as cardiac rehabilitation facilities must have one or more full-time cardiologists and two or more well-experienced physiotherapists or nurses, in addition to a dedicated training room. As of 2015, the number of hospitals providing cardiac rehabilitation was 782 (51.9%) of 1506 facilities with departments of cardiology.
For this study, we extracted data on the following complications associated with acute heart failure occurring during hospitalization: renal failure19)(N19, N170, N178, N179, N180, N189); pneumonia20)(I189); sepsis21)(A419); and stroke22)(I60, I61, I62, I63, I64, I65, I67, I68, I69). We also extracted data on each patient’s pre-rehabilitation treatments: catecholamine administration (dopamine, dobutamine, noradrenaline), carperitide administration, and cardiac surgery (coronary artery bypass grafting, valvuloplasty, and valve replacement). Use of the following procedures before starting rehabilitation was also examined: invasive and noninvasive ventilation; intra-aortic balloon pumping (IABP); percutaneous cardiopulmonary support (PCPS); and continuous hemodiafiltration (CHDF).
Based on Quan’s algorithm,23) each ICD-10 comorbidity code was converted to the Charlson Comorbidity Index (CCI). The CCI was divided into three categories: 2, 3–4, and ≥5. The body mass index (BMI) was calculated and categorized as24) underweight (<18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), and obese (≥30.0 kg/m2).
The hospital volume was defined as the average number of HF patients per year admitted to each hospital, and was categorized into tertiles. Because of the anonymous nature of the data, the requirement for informed consent was waived. The study was approved by the Institutional Review Board of The University of Tokyo.
Patient SelectionWe identified patients who were diagnosed with HF (ICD-10 codes I110, I500, I501, and I509); were NYHA class II, III, or IV; and were discharged between July 2010 and March 2014. We excluded the following patients: (i) those aged less than 60 years; (ii) those designated NYHA class I; (iii) those who underwent cardiac surgery; (iv) those who died during hospitalization; (v) those who had missing outcome data; and (vi) those who did not undergo rehabilitation during hospitalization.
Early RehabilitationWe defined early rehabilitation as rehabilitation provided by physical therapists and occupational therapists within 3 days after admission, in line with the definition in a previous guidline.14)
Outcome MeasuresThe outcome was maintained or improved mobility status between admission and discharge for each patient. Based on the Barthel Index, the level-surface mobility status was evaluated using four scores: immobile (0); wheelchair independent (1); walking with the help of one person (2); and independent, but patients may use an aid, such as a stick (3).25) In the present study, we calculated the difference in mobility scores between admission and discharge. Patients were categorized into two groups: mobility maintained or improved (≥0) and mobility unmaintained (<0).
Statistical AnalysisThe χ2-test and Mann-Whitney U-test were used to compare categorical variables and continuous variables, respectively, between the early and non-early rehabilitation groups. The number needed to treat (NNT) was calculated to estimate the number of patients who would need to be treated with early rehabilitation rather than non-early rehabilitation for one additional patient to benefit. A multivariable binary logistic regression analysis was carried out to analyze the relationship between early rehabilitation and mobility status during hospitalization with adjustment for age, sex, mobility status at admission, NYHA class, BMI, CCI, pre-rehabilitation cardiopulmonary support (i.e., catecholamine administration, mechanical ventilation, IABP, and PCPS), carperitide administration, receipt of CHDF, complications (pneumonia, renal failure, sepsis, and stroke), and hospital volume.
Because the data derived from multiple hospitals were structured by two strata (hospitals and patients), we accounted for clustering within hospitals using a generalized estimating equation with an exchangeable working correlation matrix and a robust estimator variance–covariance matrix.26,27) All statistical analyses were carried out using IBM SPSS statistics, version 22.0 (IBM, Armonk, NY). Values of P<0.05 were considered significant.
Instrumental Variable (IV) AnalysisConventional approaches, such as multivariable logistic regression analyses, cannot adjust for hidden biases caused by unmeasured confounders. Consequently, we conducted an IV analysis as a confirmatory investigation. The key assumptions of IV analysis are28,29): (i) the IV is highly correlated with the treatment, (ii) the IV is not correlated with any measured or unmeasured variables among the patient characteristics, and (iii) the IV does not affect patient outcomes except through the treatment.
The provision of early rehabilitation to HF patients may depend on the attending physicians’ attitudes toward rehabilitation and the availability of cardiovascular rehabilitation staff at an individual hospital. If a given hospital tends to conduct early rehabilitation independently of patient characteristics, early rehabilitation will be determined more strongly by the hospital in which the patient is treated than by the patient’s particular risk factors. Under such conditions, the proportion of patients receiving early rehabilitation provision per hospital can act as an IV, thereby permitting a “natural experiment” for an unbiased estimate of the outcome even in the presence of unmeasured confounders.28,29) IV analysis assumes that a patient’s choice of hospital is made independently of the hospital’s orientation toward early rehabilitation, and that a hospital’s conduct of early rehabilitation is independent of the outcome. A consistent result from an IV analysis can serve as a useful confirmation of a conventional analysis.
In the IV analysis, we included only patients admitted to hospitals treating at least 20 eligible HF patients during the study period. The continuous variable of the IV analysis (the proportion of patients receiving early rehabilitation provision per hospital) was dichotomized using the cut-off value of the 75th percentile of the proportions among the eligible patients. A two-stage least-squares method was used to estimate the risk difference in maintained or improved mobility status and its 95% confidence interval between the early and non-early rehabilitation groups with adjustment for measured and unmeasured variables. For this step, we used the ivreg2 procedure in Stata version 12 (StataCorp, College Station, TX). To confirm that the proportion of patients receiving early rehabilitation provision per hospital was not a weak IV, we used a partial F-test.30) The null hypothesis was that there was no association between the IV and the outcome. An F-statistic of >10 was considered to suggest that the IV was not weak.30)
We identified a total of 527,440 patients who were diagnosed with HF at admission in 1,279 hospitals during the study period. We selected 146,735 eligible patients including 39,357 (26.8%) who underwent early rehabilitation and 107,378 (73.2%) who underwent non-early rehabilitation (Fig. 1). The mean (standard deviation: SD) age was 82.0 (8.6) years. The mean (SD) interval from admission to starting rehabilitation and the length of hospital stay were 9.1 (11.8) days and 31.8 (30.0) days, respectively. The period between admission and the start of rehabilitation was shorter in the early rehabilitation group than in the non-early rehabilitation group [2.3 (0.6) vs. 11.5 (12.9) days]. The early rehabilitation group also had a shorter length of stay than the non-early rehabilitation group [24.3 (21.8) vs. 34.4 (31.6) days].
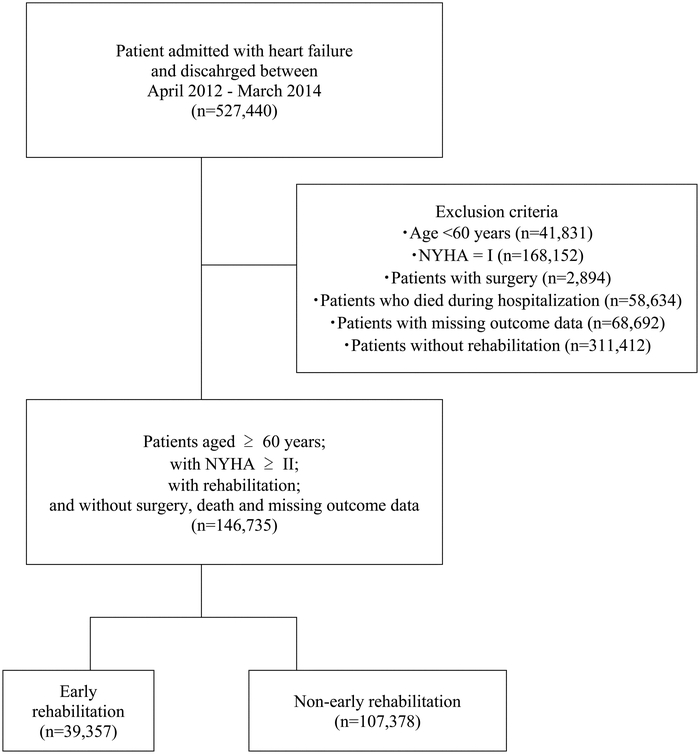
Schematic showing the patient selection process.
Table 1 shows the patient characteristics for the early and non-early rehabilitation groups. The patients in the early rehabilitation group were significantly more likely to be older, and to have a lower NYHA class, lower BMI, and lower CCI scores. Patients in the early rehabilitation group were significantly less likely require cardiopulmonary support, to be administered carperitide, to undergo CHDF, or to have complications. Moreover, high-volume hospitals were more likely to conduct early rehabilitation.
| All patients (n =146,735) |
Early rehabilitation (n =39,357) |
Non-early rehabilitation (n =107,378) |
P | |||||
| Age category (years), n (%) | <0.001 | |||||||
| 60–69 | 14,630 | (10.0) | 3,641 | (9.3) | 10,989 | (10.2) | ||
| 70–79 | 35,906 | (24.5) | 9,269 | (23.6) | 26,637 | (24.8) | ||
| 80–89 | 68,754 | (46.9) | 18,224 | (46.3) | 50,530 | (47.1) | ||
| ≥90 | 27,445 | (18.7) | 8,223 | (20.9) | 19,222 | (17.9) | ||
| Sex, n (%) | 0.064 | |||||||
| Male | 67,019 | (45.7) | 17,819 | (45.3) | 49,200 | (45.8) | ||
| Female | 79,716 | (54.3) | 21,538 | (54.7) | 58,178 | (54.2) | ||
| NYHA class at admission, n (%) | <0.001 | |||||||
| II | 43,410 | (29.6) | 13,194 | (33.5) | 30,216 | (28.1) | ||
| III | 56,020 | (38.2) | 14,869 | (37.8) | 41,151 | (38.3) | ||
| IV | 47,305 | (32.2) | 11,294 | (28.7) | 36,011 | (33.5) | ||
| Body mass index (kg/m2), n (%) | <0.001 | |||||||
| 18.5–22.9 | 58,339 | (39.8) | 15,953 | (40.5) | 42,386 | (39.5) | ||
| <18.5 | 21,809 | (14.9) | 6,061 | (15.4) | 15,748 | (14.7) | ||
| 23.0–24.9 | 20,447 | (13.9) | 5,666 | (14.4) | 14,781 | (13.8) | ||
| 25.0–29.9 | 21,930 | (14.9) | 5,729 | (14.6) | 16,201 | (15.1) | ||
| ≥30 | 5,829 | (4.0) | 1,502 | (3.8) | 4,327 | (4.0) | ||
| missing | 18,381 | (12.5) | 4,446 | (11.3) | 13,935 | (13.0) | ||
| Charlson Comorbidity Index | <0.001 | |||||||
| 2 | 92,267 | (62.9) | 25,461 | (64.7) | 66,806 | (62.2) | ||
| 3–4 | 49,310 | (33.6) | 12,617 | (32.1) | 36,693 | (34.2) | ||
| ≥5 | 5,142 | (3.5) | 1,273 | (3.2) | 3,869 | (3.6) | ||
| missing | 16 | (0.0) | 6 | (0.0) | 10 | (0.0) | ||
| Pre-rehabilitation treatment, n (%) | ||||||||
| Receipt of cardiopulmonary support | 41,368 | (28.2) | 8,020 | (20.4) | 33,348 | (31.1) | <0.001 | |
| Use of catecholamine | 25,825 | (17.6) | 4,001 | (10.2) | 21,824 | (20.3) | <0.001 | |
| Receipt of ventilation | 24,219 | (16.5) | 5,114 | (13.0) | 19,105 | (17.8) | <0.001 | |
| Receipt of IABP | 9,490 | (6.5) | 63 | (0.2) | 9,427 | (8.8) | <0.001 | |
| Receipt of PCPS | 67 | (0.0) | 1 | (0.0) | 66 | (0.1) | <0.001 | |
| Use of carperitide | 61,579 | (42.0) | 14,346 | (36.5) | 47,233 | (44.0) | <0.001 | |
| Receipt of CHDF | 1,161 | (0.8) | 77 | (0.2) | 1,084 | (1.0) | <0.001 | |
| Complications, n (%) | ||||||||
| Pneumonia | 5,898 | (4.0) | 1,176 | (3.0) | 4,722 | (4.4) | <0.001 | |
| Renal failure | 640 | (0.4) | 202 | (0.5) | 438 | (0.4) | 0.007 | |
| Sepsis | 790 | (0.5) | 141 | (0.4) | 649 | (0.6) | <0.001 | |
| Stroke | 2,073 | (1.4) | 386 | (1.0) | 1,687 | (1.6) | <0.001 | |
| Hospital volume (per year), n (%) | <0.001 | |||||||
| ≤256 | 49,018 | (33.4) | 12,259 | (31.1) | 36,759 | (34.2) | ||
| 257–454 | 47,360 | (32.3) | 12,414 | (31.5) | 34,946 | (32.5) | ||
| ≥455 | 50,357 | (34.3) | 14,684 | (37.3) | 35,673 | (33.2) | ||
| Mobility status at admission, n (%) | <0.001 | |||||||
| 3 | 41,121 | (28.0) | 11,584 | (29.4) | 29,537 | (27.5) | ||
| 2 | 21,971 | (15.0) | 5,961 | (15.1) | 16,010 | (14.9) | ||
| 1 | 13,927 | (9.5) | 3,503 | (8.9) | 10,424 | (9.7) | ||
| 0 | 69,716 | (47.5) | 18,309 | (46.5) | 51,407 | (47.9) | ||
| Mobility status at discharge, n (%) | <0.001 | |||||||
| 3 | 74,000 | (50.4) | 20,845 | (53.0) | 53,155 | (49.5) | ||
| 2 | 30,796 | (21.0) | 7,723 | (19.6) | 23,073 | (21.5) | ||
| 1 | 12,635 | (8.6) | 3,107 | (7.9) | 9,528 | (8.9) | ||
| 0 | 29,304 | (20.0) | 7,682 | (19.5) | 21,622 | (20.1) | ||
IABP, intra-aortic balloon pumping; PCPS, percutaneous cardiopulmonary support; CHDF, continuous hemodiafiltration.
Mobility refers to indoors mobility about the house or ward and may include the use of an aid. If using a wheelchair, patients must be able to negotiate corners/doors unaided. Mobility 3 denotes independent (but patients may use any aid, e.g., a stick); mobility 2 denotes the ability to walk with the help of one person (verbal or physical support); mobility 1 denotes wheelchair independent, including the ability to negotiate corners, etc.; and mobility 0 denotes immobile.
The proportion of patients with immobility decreased from 47.5% at admission to 20.0% at discharge. As shown in Table 2, the crude proportion of patients with maintained or improved mobility status was significantly higher in the early rehabilitation group than in the non-early rehabilitation group (94.7% vs. 93.3%; P<0.001) and the NNT was 71.4 (95% confidence interval, 61.1–93.0).
| All patients (n=146,735) | Early rehabilitation (n=39,357) | Non-early rehabilitation (n=107,378) |
P | Number needed to treat | 95% confidence interval | |
| Maintained or improved mobility status, n (%) | 137,494 (93.7) |
37,269 (94.7) |
100,225 (93.3) |
<0.001 | 71.4 | 61.1–93.0 |
| Unmaintained mobility status, n (%) | 9,241 (6.3) |
2,088 (5.3) |
7,153 (6.7) |
Table 3 shows the results of multivariable binary logistic regression analysis for changes in mobility status during hospitalization. Compared with the non-early rehabilitation group, the early rehabilitation group was significantly more likely to have maintained or improved mobility status (odds ratio, 1.32; 95% confidence interval, 1.21–1.43, P<0.001). The following factors were significantly associated with a lower probability of maintained or improved mobility status: higher age, being female, being NYHA class III or IV, having higher CCI, receipt of CHDF, and complications of pneumonia, sepsis, and stroke. Receipt of carperitide and the complication of renal failure were associated with a higher probability of maintained or improved mobility status.
| Odds ratio | 95% confidence interval | P | ||||
| Rehabilitation | ||||||
| Non-early rehabilitation | Reference | |||||
| Early rehabilitation | 1.32 | 1.21 | – | 1.43 | <0.001 | |
| Age (years) | ||||||
| 60–69 | Reference | |||||
| 70–79 | 0.56 | 0.50 | – | 0.63 | <0.001 | |
| 80–89 | 0.33 | 0.29 | – | 0.37 | <0.001 | |
| ≥90 | 0.21 | 0.18 | – | 0.24 | <0.001 | |
| Sex | ||||||
| Male | Reference | |||||
| Female | 0.84 | 0.80 | – | 0.88 | <0.001 | |
| NYHA class at admission | ||||||
| II | Reference | |||||
| III | 0.80 | 0.76 | – | 0.86 | <0.001 | |
| IV | 0.83 | 0.77 | – | 0.91 | 0.457 | |
| Body mass index (kg/m2) | ||||||
| 18.5–22.9 | Reference | |||||
| <18.5 | 0.88 | 0.83 | – | 0.94 | <0.001 | |
| 23.0–24.9 | 1.08 | 1.01 | – | 1.16 | 0.028 | |
| 25.0–29.9 | 1.16 | 1.08 | – | 1.24 | <0.001 | |
| ≥30 | 1.06 | 0.94 | – | 1.21 | 0.339 | |
| missing | 0.98 | 0.90 | – | 1.06 | 0.620 | |
| Charlson Comorbidity Index | ||||||
| 2 | Reference | |||||
| 3–4 | 0.78 | 0.61 | – | 1.00 | <0.001 | |
| ≥5 | 0.58 | 0.52 | – | 0.65 | <0.001 | |
| Pre-rehabilitation treatment | ||||||
| Receipt of cardiopulmonary support | 0.95 | 0.88 | – | 1.01 | 0.092 | |
| Use of carperitide | 1.08 | 1.01 | – | 1.16 | 0.029 | |
| Receipt of CHDF | 0.78 | 0.61 | – | 1.00 | 0.046 | |
| Complications | ||||||
| Pneumonia | 0.63 | 0.57 | – | 0.70 | <0.001 | |
| Renal failure | 1.57 | 1.06 | – | 2.31 | 0.024 | |
| Sepsis | 0.56 | 0.44 | – | 0.72 | 0.001 | |
| Stroke | 0.45 | 0.42 | – | 0.58 | <0.001 | |
| Hospital volume (per year) | ||||||
| ≤256 | Reference | |||||
| 257–454 | 1.08 | 0.96 | – | 1.22 | 0.214 | |
| ≥455 | 1.07 | 0.94 | – | 1.23 | 0.272 | |
In the IV analysis, we included 146,263 patients admitted to 1,142 hospitals that treated at least 20 eligible HF patients during the study period. The continuous IV variable (the proportion of patients receiving early rehabilitation provision per hospital) was dichotomized by the cut-off value of 27.0%, which was the 75th percentile of the proportions. The F-statistic showed that the proportion of patients receiving early rehabilitation was a strong IV (F=46.8; P<0.01). In the IV analysis, early rehabilitation was associated with an increased proportion of maintained or improved mobility status (risk difference, 0.8%; 95% confidence interval, 0.4%–1.1%; P<0.001).
In the present study, we used a large nationwide acute-care inpatient database to examine the association of early rehabilitation with changes in mobility status during hospitalization in HF patients with NYHA class II, III, or IV. The results showed that early rehabilitation intervention within 3 days after admission was associated with a higher proportion of HF patients with maintained or improved mobility status.
The association between early rehabilitation and mobility status is likely related with the symptom of frailty. Generally, frailty develops in older people; consequently we excluded patients aged less than 60 years.
Cardiac rehabilitation is generally divided into three phases: inpatient program (phase I), outpatient program (phase II), and maintenance (phase III). In phase I, physical rehabilitation aims to minimize the influence of inactivity and maintain or improve muscle strength and mobility. However, to the best of our knowledge, no previous studies have analyzed the effectiveness of early rehabilitation for elderly inpatients with HF at improving or maintaining mobility during phase I. It is noteworthy that a previous study found that the length of hospital stay in patients with HF in Japan was longer than those in other countries.31) The reason for this was the difference in clinical practice patterns between Japan and western countries. This may limit the generalizability of the findings, however, the management of maintaining mobility status remains important considering activity of daily living after discharge.
Maintaining mobility status is also important for preventing frailty. Frailty is generally defined as a multidimensional syndrome arising from the interplay of genetic, biological, physical, psychological, social, and environmental factors.32) Therefore, a comprehensive rehabilitation program including patient education, psychological intervention, and nutrition management is recommended to prevent frailty. Previous studies showed that frailty was associated with reduced lower-limb muscle strength,33) and that muscle weakness with muscle wasting was a frequent comorbidity among patients with HF.34) Consequently, early physical exercise training may represent a core component of inpatient rehabilitation to prevent physical inactivity, muscle weakness, and reduced muscle strength.
Previous studies have reported the effects of physical exercise in patients with heart disease in terms of muscle fibers and the mitochondrial apparatus,35,36,37) the neuroendocrine system,38) cardiac function through anti-remodeling effects,36) and improvement of heart perfusion.39) In the present study, the details of the rehabilitation programs were not determined, and the mechanism for the effectiveness of early rehabilitation on maintaining mobility remains unclear. However, we speculate that interventions such as early rehabilitation could play an important role in preventing the progression of disability.
The present study has several limitations. First, the database does not include detailed information about the severity of cardiac dysfunction (e.g., the left ventricular ejection fraction or underlying diseases). Second, the database includes information relating to the period of hospitalization only. Consequently, we were unable to analyze pre-hospital and post-discharge outcomes, including long-term mobility. Third, mobility status may be affected not only by the level of performance, but also by risk management to prevent falls. Fourth, in the present study, we used mobility status as the outcome, but the validity and reliability of recorded data on the outcome have not been evaluated. Moreover, approximately 15% of the outcome data were missing, and the distribution of the missing data might not have been random.
Although the changes in mobility status were multifactorial, the present retrospective study using a national inpatient database showed that early rehabilitation was independently associated with a reduction in unmaintained mobility status in elderly HF patients with NYHA class II, III, or IV.
This study was funded by grants from the Ministry of Health, Labour and Welfare, Japan and The Japan Agency for Medical Research and Development.
The authors declare that there are no conflicts of interest.