2019 Volume 4 Article ID: 20190002
2019 Volume 4 Article ID: 20190002
Objective: Repetitive overhead movements stress the dominant shoulder of volleyball players, potentially causing glenohumeral internal rotation deficit (GIRD) and suprascapular neuropathy. The aim of this study was to determine the prevalence of pathological GIRD and suprascapular neuropathy in male collegiate volleyball players. Methods: We evaluated 22 male collegiate volleyball players and compared the range of motion, the isometric shoulder strength, the thickness of the infraspinatus (ISP) muscle, and the latency and amplitude of the suprascapular nerve [in a nerve conduction study (NCS)] between the hitting and contralateral shoulders. Correlations between the physical findings and each parameter were also determined. Results: The internal rotation angle of the hitting shoulder (55.1±8.7°) was significantly less than that of the contralateral shoulder (64.5±10.2°) (P<0.001); pathological GIRD (≥20°) was found in four players (18.2%). Three players (13.6%) showed abnormal electrophysiological findings of the suprascapular nerve on the ISP muscle in the hitting shoulder. The external-to-internal rotation (ER/IR) torque ratio in the hitting shoulder (99±18%) was significantly lower than that in the contralateral shoulder (106±12%) (P=0.04); no significant differences were observed in ISP muscle thickness or NCS data between the hitting and contralateral shoulders. Conclusion: The prevalence of pathological GIRD in male collegiate volleyball players was consistent with that of previous studies. Meanwhile, the prevalence of suprascapular neuropathy was less than that previously reported in high-level volleyball players. Preventive posterior rotator cuff strengthening programs are recommended to correct imbalances between ER and IR in the hitting shoulder, thereby decreasing the risk of shoulder injury.
The dominant shoulders of overhead-throwing athletes, such as volleyball, tennis, and baseball players, are required to perform repetitive high-speed motions. These motions may cause several asymmetric changes between the dominant and contralateral shoulders, particularly in high-level athletes.1) Multiple studies have demonstrated that the dominant shoulder in overhead-throwing athletes develops decreased internal rotation compared with that of the contralateral shoulder. This decrease is called the glenohumeral internal rotation deficit (GIRD).2,3,4) Tightness of the rotator cuff and posterior capsule and humeral retrotorsion are considered to be responsible for GIRD, which may induce various injuries, such as internal impingement, rotator cuff injury, superior labrum anterior and posterior lesion (SLAP), and glenohumeral joint instability.5) The current perception is that GIRD is a chronic adaptation that leads to an increased risk of pathologic conditions in the dominant extremity, specifically shoulder or elbow injuries in overhead-throwing athletes.6)
Furthermore, a high prevalence of suprascapular neuropathy accompanied by infraspinatus (ISP) muscle atrophy, which may decrease the strength of external rotation of the dominant shoulder,7,8) has been reported in male professional volleyball players.9,10,11) During the cocking and follow-through phases of a volleyball serve, the terminal branches of the suprascapular nerve to the belly of the infraspinatus are stretched by the maximum eccentric contraction of the infraspinatus muscle across the lateral edge of the spine of the scapula.12) This entrapment of the suprascapular nerve at the spinoglenoid notch is frequently painless and is therefore overlooked in volleyball players.9) In a nerve conduction study of professional beach volleyball players, Lajtai et al.11) found a significantly higher latency and lower amplitude of the suprascapular nerve in the hitting shoulder of the entire study group and in the subgroup with ISP muscle atrophy. These findings suggest the presence of a subclinical asymptomatic suprascapular neuropathy in male volleyball players.
Although previous studies have shown that high-level professional athletes develop physiological changes, such as GIRD and ISP muscle atrophy, in their hitting shoulders, no information is available about these changes in collegiate-level volleyball players. The objective of the current study was to determine the prevalence of pathological GIRD and suprascapular neuropathy of the hitting shoulder in male collegiate volleyball players. We hypothesized that male collegiate volleyball players have asymmetric changes in the range of internal rotation, ISP muscle thickness, external rotation torque, and latency and amplitude [in a nerve conduction study (NCS)] of the suprascapular nerve between the hitting and the contralateral arms, similar to those found in male professional volleyball players in previous reports. We also aimed to determine correlations between physical findings, such as impingement sign and rotator cuff test results, and shoulder strength and NCS data of the hitting shoulders.
Twenty-two male collegiate volleyball players aged between 18 and 23 years (mean age: 20.7 years) participated in this cross-sectional study. The average height and weight of the players were 174±6 cm and 68±6 kg, respectively. Their average duration of playing volleyball was 7.5±3.3 years with a mean of 10±2 training hours per week. None of the players had a history of shoulder surgery or neurological disease. The hitting arm, defined as the arm used to spike and serve, was the right arm in 21 players and the left arm in 1 player. The participants comprised 11 wing spiker, 4 middle blockers, 4 setters, and 3 liberos. All study participants provided informed consent, and the study design was approved by the appropriate ethics review board of Hirosaki University, School of Medicine (EK No. 2016–266). The study was performed according to the ethical standards of the Declaration of Helsinki.
Clinical AssessmentThe bilateral shoulders of each player were examined using Neer’s test13) and Hawkins–Kennedy test14) to determine whether subacromial impingement was present. The presence of rotator cuff lesions was also examined using the empty can test15) and the full can test.16) If shoulder pain was reproduced by Neer’s test or Hawkins-Kennedy test, this was considered to be evidence of positive subacromial impingement. Similarly, if shoulder pain and weakness was reproduced by either the empty can test or the full can test, it was considered to be a positive rotator cuff test (RCT).
Range of MotionTo evaluate the shoulder range of motion (ROM), the athlete was placed in the supine positioned, shoulder at 90° abduction, elbow at 90° flexion, and forearm in the neutral position. This position is useful to eliminate scapulothoracic movement.3) For all measurements, the axis of the goniometer was positioned over the olecranon, the fixed arm remained perpendicular to the ground, and the adjustable arm was aligned parallel to the ulna (with the center over the styloid process). The assessment of the external and internal rotation ROM was performed passively, with one examiner stabilizing the athlete’s shoulder and the other measuring the ROM (Fig. 1A, B). The final ROM was measured after a firm endpoint was reached and no shoulder compensations were observed. Passive external and internal rotations were both measured with the goniometer by the same investigator. The total ROM was calculated by summing the internal and external rotations of each limb. GIRD measurements were calculated from the difference in internal rotation ROMs between the hitting and contralateral arms.
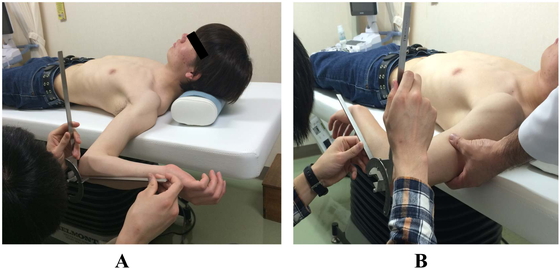
(A) Measurement of external rotation angle with a goniometer. (B) Measurement of internal rotation angle to eliminate scapulohumeral motion.
The maximal isometric strengths of four shoulder muscles (i.e., elevators, lower trapezius, external rotators, and internal rotators) were bilaterally assessed using a hand-held dynamometer (HHD; microFET2; Hoggan Health Industries Inc, West Jordan, UT, USA), as previously described.17) Elevators were measured with the subject in the sitting position with the arm in the scapular plane at 90° of elevation, the elbow extended, and the forearm in the neutral position (Fig. 2A). For the lower trapezius, the participant was lying prone with the arm located diagonally overhead in line with the lower fibers of the trapezius and the thumb pointed upward. The investigator applied pressure against the forearm in a downward direction toward the table (Fig. 2B). External and internal rotators were measured with the subject in the supine position with knees flexed, the shoulder at 90° abduction, the elbow at 90° flexion, and the forearm in the neutral position. The participant was instructed to rotate the shoulder joint internally or externally against the HHD placed on the wrist (Fig. 2C, D). Force was directly applied downward 3 cm proximal to the styloid process of the radius, and the participant was asked to perform elevation against the resistance of the examiner. In each measurement, the participant was asked to maintain the position of the tested arm for 5 s as the examiner pushed against the limb until the maximal effort was overcome and the joint being tested gave way. Three measurements with a 30-s rest period between each measurement were recorded and averaged for each muscle. The peak isometric strengths (N) of the elevator and lower trapezius were multiplied by the distance (m) from the center of the shoulder joint to the wrist where the HHD was applied (Nm) and then normalized by the body weight (Nm/kg). Similarly, the peak isometric strength (N) of the internal and external rotators was multiplied by the distance (m) from the center of the elbow joint to the wrist where the HHD was applied (Nm) and then normalized by body weight (Nm/kg). We also calculated the external-to-internal rotation (ER/IR) torque ratio and identified athletes with abnormal strength ratios.3,17)

Measurement of isometric strength of muscles with a handheld dynamometer: (A) elevators, (B) lower trapezius, (C) external rotators, and (D) internal rotators.
The thicknesses of both the supraspinatus (SSP) and ISP muscles of bilateral shoulders were measured using an ultrasound scanning system with a 45-mm linear-array transducer (SONIMAGE 613; Konica Minolta, Tokyo, Japan). Imaging began with the left shoulder for all participants, regardless of which side was dominant. Participants were asked to sit upright on a stool with their head in a neutral position, shoulders abducted to 0°, and forearm fully pronated on their thigh. The examiner initially positioned the ultrasound transducer on the midpoint of the scapular spine and perpendicular to the long axis of the SSP muscle belly. The examiner measured the thickness of the SSP muscle below the upper trapezius muscle (Fig. 3A, B). Thereafter, the transducer was moved to just below the scapular spine and positioned to the medial fourth of the scapular spine and perpendicular to the ISP muscle fiber where the deltoid muscle does not overlap the ISP muscle (Fig. 3C, D). Examiners exerted as little pressure through the ultrasound head as possible to avoid compressing the ISP muscle and inadvertently changing its shape and/or thickness.18) Following data collection, the images were downloaded to a laptop computer. The thicknesses of the SSP and ISP muscles were measured in the center of the image using Image J software (V1.38t, National Institutes of Health, Bethesda, MD, USA) and reported in millimeters (to the nearest hundredth). This measurement was taken from the inferior-most aspect of the superficial fascia to the most superior aspect of the infraspinous fossa, which appeared as a bright, continuous hyperechoic line spanning the width of the screen (Fig. 3B, D). This process was repeated on every image. The averaged value of three measurements was calculated for analysis. If the thickness of the SSP or ISP muscle of the hitting shoulder was 2 mm less than that of the contralateral shoulder, it was defined as SSP or ISP muscle atrophy.

(A) Measurement of SSP muscle thickness using ultrasonography. (B) SSP muscle thickness was measured as the distance between the underlining fascia of the upper trapezius and the supraspinous fossa. (C) Measurement of ISP muscle thickness. (D) ISP muscle thickness was measured as the distance between the superficial fascia of the infraspinatus and the infraspinous fossa.
A NCS of the suprascapular nerve of the bilateral shoulders was performed using surface electrodes with the KEYPOINT system (Medtronic Dantec, Minneapolis, MN, USA). Subjects were examined in the seated position with the elbow flexed and the forearm allowed to rest gently on the lap. To record the SSP muscle activity, the active electrode was placed 2 cm medial to the midpoint of the spine of the scapula. The reference electrode was placed over the midline of the thoracic spine at the same level. To record the ISP muscle activity, the active electrode was placed 2 cm below the midpoint of the spine of the scapula. The reference electrode was placed over the midline of the thoracic spine at the same level (Fig. 4A). The ground electrode was placed over the acromion. Nerve stimulation was applied at Erb’s point with the cathode placed slightly above the upper margin of the clavicle and lateral to the clavicular head of the sternocleidomastoid muscle (Fig. 4B). In all determinations, a supramaximal stimulus was applied. Values for onset latency and amplitude (baseline to negative peak) were recorded (Fig. 4C). Standard values for the latency to the SSP and ISP muscles are approximately 3.2 and 3.6 ms, respectively.19) According to Buschbacher et al.,19) a side-to-side difference greater than 20% of latency and greater than 50% of amplitude is defined as abnormal.

(A) Surface electrodes for the nerve conduction study of the suprascapular nerve on the ISP muscle. (B) Stimulation at Erb’s point with a cathode. (C) Compound muscle action potential of suprascapular nerve. Latency of the SSP (1) and ISP muscles (2) was measured as L1 and L2 (mS), respectively. The amplitude for the SSP and ISP muscles was measured as A1 and A2 (mV), respectively.
Paired Student’s t-tests were used to compare ROM, shoulder strength, thickness of rotator cuff muscle, and latency and amplitude of suprascapular nerves between the hitting and the contralateral shoulders. Wilcoxon signed rank tests were carried out to determine the effect of positive impingement sign (positive in either Neer’s test or Hawkins-Kennedy test), positive RCT (positive in either full can test or empty can test), and ISP muscle atrophy of the hitting shoulder on shoulder strength and NCS data. Statistical analysis was performed using SPSS version 23 for Macintosh (SPSS Inc., Chicago, IL, USA). The level of significance was set at P < 0.05.
In the assessment of the hitting shoulder, the subacromial impingement test was positive in five players (22.7%) and RCT was positive in six players (27.2%). Three players showed positive signs in both tests, and two regularly complained of pain in their hitting shoulders during the cocking phase of spiking when their arms were elevated. No players were positive in either the subacromial impingement test or RCT in the contralateral shoulder.
Shoulder ROMThe external rotation of the hitting shoulder (96.4±9.2°) was significantly greater than that of the contralateral shoulder (91.9±9.7°, P=0.001), whereas the internal rotation of the hitting shoulder (55.1±8.7°) was significantly less than that of the contralateral shoulder (64.5±10.2°, P<0.001). The average GIRD of the hitting shoulder was −9.4±10.6° (Table 1). Pathological GIRD (greater than 20°) was found in four players (18.2%).
| Hitting arm | Contralateral arm | P-value | ||
| Range of motion: | ||||
| External rotation (°) | 96.4±9.2 | 91.9±9.7 | 0.001 * | |
| Internal rotation (°) | 55.1±8.7 | 64.5±10.2 | <0.001 * | |
| GIRD | -9.4±10.6 | |||
| Total rotation (°) | 151.5±12.8 | 156.4±15.0 | 0.058 | |
| Isometric shoulder strength: | ||||
| Elevators (Nm/kg) | 0.65±0.20 | 0.64±0.19 | 0.296 | |
| Lower trapezius (Nm/kg) | 0.45±0.09 | 0.44±0.09 | 0.609 | |
| External rotators (Nm/kg) | 0.43±0.10 | 0.45±0.07 | 0.305 | |
| Internal rotators (Nm/kg) | 0.45±0.09 | 0.43±0.08 | 0.315 | |
| ER/IR torque ratio (%) | 99±18 | 106±12 | 0.040 * | |
| Thickness of rotator cuff muscle: | ||||
| SSP muscle (mm) | 20.6±2.4 | 20.4±3.0 | 0.678 | |
| ISP muscle (mm) | 12.7±1.8 | 12.9±2.1 | 0.439 | |
| Nerve conduction study: | ||||
| SSP: | ||||
| Latency (mS) | 2.9±0.3 | 2.9±0.4 | 0.347 | |
| Amplitude (mV) | 2.2±0.5 | 2.3±0.6 | 0.651 | |
| ISP: | ||||
| Latency (mS) | 3.0±0.3 | 3.0±0.5 | 0.963 | |
| Amplitude (mV) | 4.3±1.91 | 4.4±1.8 | 0.821 | |
Data are presented as mean ± standard deviation.
*Significant difference between hitting and contralateral shoulders (P<0.05).
No significant differences were found between the hitting and contralateral shoulders in the isometric strength of elevators (0.65±0.20 Nm/kg, 0.64±0.19 Nm/kg; P=0.296), lower trapezius (0.45±0.09 Nm/kg, 0.44±0.09 Nm/kg; P=0.609), external rotators (0.43±0.10 Nm/kg, 0.45±0.07 Nm/kg; P=0.305), and internal rotators (0.45±0.09 Nm/kg, 0.43±0.08 Nm/kg; P=0.315)(Table 1). However, the external rotation torque of the hitting shoulder in seven players (31.8%) was less than 90% of that of the contralateral shoulder, and the mean ER/IR torque ratio in the hitting shoulder (0.99±0.18) was significantly less than that in the contralateral shoulder (1.06±0.12, P=0.04) (Table 1).
UltrasonographyNo significant difference was found in SSP muscle thickness between the hitting shoulder (20.6±2.4 mm) and contralateral shoulder (20.4±3.0 mm, P=0.678), or in ISP muscle thickness (12.7±1.8 mm, 12.9±2.1mm, P=0.439) (Table 1). SSP and ISP muscle atrophy, in which the thickness of each muscle of the hitting shoulder was 2 mm less than those of the contralateral shoulder, was found in six players (27.3%) and three players (13.6%), respectively.
Nerve Conduction StudyNo significant differences between the hitting shoulder and the contralateral shoulder in the latency or amplitude of the suprascapular nerve were recorded for the SSP or ISP muscles (Table 1). Two players (9%) had more than a 20% increase in latency recorded in the SSP muscle of the hitting shoulder compared with that of the contralateral shoulder, whereas no players had more than a 50% difference in amplitude recorded in the SSP muscle between the shoulders. Three players (13.6%) exhibited more than a 20% increase in latency recorded in the ISP muscle of the hitting shoulder compared with that of the contralateral shoulder. One of them had more than a 50% decrease in amplitude of the suprascapular nerve recorded in the ISP muscle, but the strength of the external rotators in the hitting shoulder was not less than 90% of that of the contralateral shoulder.
Correlations with Clinical FindingsThe players with positive impingement sign had a significantly lower external rotation strength of the hitting shoulder (76±21% of the contralateral side) than those with negative impingement sign (100±16% of the contralateral side) (P=0.048)(Table 2). There were no significant differences in shoulder strength or NCS findings between the RCT-positive and RCT-negative groups (Tables 2 and 3). Players with ISP muscle atrophy had lower strength in their elevators (92±08% of contralateral side) than those without ISP muscle atrophy did (104±09% of contralateral side), although the difference was not significant (P=0.053) (Table 2).
| Impingement sign | Rotator cuff test | ISP muscle atrophy | |||||||
| (+) n=5 | (−) n=17 | P-value | (+) n=6 | (−) n=16 | P-value | (+) n=3 | (−) n=19 | P-value | |
| Side-to-side ratio§ | |||||||||
| Elevators (%) | 100±10 | 103±10 | 0.595 | 101±11 | 103±09 | 0.693 | 92±08 | 104±09 | 0.053 |
| Lower Trapezius (%) | 96±14 | 106±21 | 0.401 | 96±16 | 106±20 | 0.329 | 94±16 | 105±20 | 0.408 |
| ER (%) | 76±21 | 99±16 | 0.048* | 86±19 | 100±15 | 0.178 | 95±10 | 96±18 | 0.718 |
| IR (%) | 105±18 | 104±15 | 1 | 108±19 | 103±14 | 0.641 | 96±09 | 106±16 | 0.308 |
| ER/IR torque ratio of hitting shoulder |
93±25 | 100±15 | 0.762 | 90±22 | 102±15 | 0.407 | 114±28 | 96±15 | 0.408 |
Data are presented as mean ± standard deviation.
§Side-to-side ratio: percentage of hitting shoulder compared to contralateral shoulder.
*Significant difference between groups (P<0.05)
| Impingement sign | Rotator cuff test | ISP muscle atrophy | |||||||
| (+) n=5 | (−) n=17 | P-value | (+) n=6 | (−) n=16 | P-value | (+) n=3 | (−) n=19 | P-value | |
| SSP muscle | |||||||||
| Latency (ms) | 2.9±0.3 | 2.9±0.3 | 0.858 | 2.8±0.2 | 2.9±0.3 | 0.464 | 2.9±0.3 | 2.9±0.3 | 0.858 |
| Amplitude (mV) | 2.0±0.4 | 2.3±0.5 | 0.134 | 2.4±0.3 | 2.2±0.5 | 0.787 | 2.0±0.4 | 2.3±0.5 | 0.134 |
| ISP muscle | |||||||||
| Latency (ms) | 3.1±0.3 | 3.0±0.2 | 0.541 | 2.9±0.3 | 3.0±0.3 | 0.308 | 3.1±0.3 | 3.0±0.2 | 0.541 |
| Amplitude (mV) | 5.0±2.3 | 4.0±1.7 | 0.329 | 4.4±2.7 | 4.2±1.9 | 1 | 5.0±2.3 | 4.0±1.7 | 0.329 |
Data are presented as mean ± standard deviation.
Repetitive stress on the hitting shoulder during volleyball spiking and serving is assumed to be the cause of GIRD and suprascapular neuropathy with weakness of external rotators and ISP muscle atrophy, particularly in high-level male volleyball players.1,9,10,11) The current study is the first to present a set of data on ISP muscle thickness and electrophysiological data on the suprascapular nerve for male volleyball players. The prevalence of suprascapular neuropathy in male collegiate volleyball players in the current study (13.6%), determined by NCS, was less than that found in high-level male professional volleyball players (34%) reported in a previous study.10) However, significant decreases in the internal rotation angle and ER/IR torque ratio were observed in the hitting shoulder of collegiate volleyball players, which is consistent with previous studies.
Glenohumeral Internal Rotation DeficitThe asymmetry in ROMs observed in the current study is consistent with previous studies showing a decrease in internal rotation and an increase in external rotation in the hitting shoulder compared with the contralateral shoulder in male volleyball players.3,11,20) The mean magnitude of GIRD in the current study (9.4°) was similar to that found by Saccol et al.3)(10.5°), who investigated 19 young male beach volleyball players. Moreover, the average decrease in total rotation in the hitting shoulder in the current study (4.9°) was similar to that recorded in the study of Schwab et al. (4.4°), who studied male elite volleyball players.20) The prevalence of pathological GIRD (18.2%), which is considered to be a risk of shoulder injury,4,5) identified in the current study was similar to that reported by Whiteley et al.21)(15.4%), who evaluated 162 professional male overhead athletes. A recent meta-analysis covering 2195 athletes with a mean age of 20.8 years demonstrated that shoulders with GIRD favor an upper extremity injury, with a mean difference of 3.11° (95% CI, −0.13° to 6.36°; P=0.06).22) It has also been reported that increasing the eccentric overload to the posterior rotator cuff during the deceleration phase might result in rotator cuff stiffness of the hitting shoulder and subsequent internal rotation deficits.5) Several studies reported that humeral retroversion of the dominant arm is increased in overhead-throwing athletes.10,20) A change in humeral torsion toward retroversion is considered to result in an external rotation shift of the rotation range of motion with an increase in ER range and a decrease in IR range that is proportional to the retroversion change.
Muscular StrengthThe balance of muscular strength of the internal and external rotators is critical to maintain a suitable position of the humeral head on the glenoid during overhead-throwing activity.7,23) The current study demonstrated a significant decrease in ER/IR torque ratio of the hitting shoulder compared with that of the contralateral shoulder in male collegiate volleyball players. This result is consistent with previous studies that investigated 84 professional beach volleyball players10) and young competitive tennis players with a history of shoulder problems.17) A decrease in the ER/IR torque ratio in the hitting shoulder is explained by decreased muscular strength in external rotators,7) increased strength in internal rotators,3) or both. Cornu et al.7) concluded that high-level volleyball practice induces a strong external rotator deficit because ER/IR torque ratios were always significantly lower among professional (0.42±0.03) versus amateur volleyball players (0.56±0.03) for pooled isometric and concentric conditions. Meanwhile, Saccol et al.3) showed an increase in internal rotator strength in the dominant shoulder caused by the higher demand imposed on these muscles during the overhead-throwing motion. Muscle imbalance between ER and IR in the hitting shoulder may cause glenohumeral instability during spiking or serving in volleyball, predisposing volleyball players to a greater risk of shoulder injury. Preventive posterior rotator cuff strengthening programs for athletes performing high-level overhead activities are recommended to correct imbalances of rotator strength ratios.10)
ISP Muscle AtrophyISP muscle atrophy is usually present only in the dominant arm of players, and blockers are less affected than smashers.10) Clinically, the affected shoulder has a deficiency of external rotators, but many players with objective signs of ISP muscle atrophy do not have subjective symptoms.11) The prevalence of ISP muscle atrophy on visual inspection in professional male volleyball players ranges from 25% to 34%,10,11,24,25,26) and it is usually accompanied by weakness of external rotation. In contrast, ISP muscle atrophy of the hitting shoulder was found in only three players (13.6%) on ultrasonography in the current study, and only one of these had less than 90% of the external rotation torque of the contralateral shoulder. The differences in the prevalence of ISP muscle atrophy between previous studies and the current study may be explained by the difference in performance level of the athletes (i.e., professional level vs. collegiate level) or by the difference in methods used to determine ISP muscle atrophy (visual inspection vs. ultrasonography). It is worth noting that the range of the inspection window is limited in ultrasonography.
Nerve Conduction StudySuprascapular neuropathy can be caused by direct compression of the suprascapular nerve at the level of the scapular notch or at the spinoglenoid notch as a result of a ganglion cyst or a hypertrophied transverse scapular or spinoglenoid ligament. A single atrophy of the ISP muscle can be observed if the inferior branch of the suprascapular nerve only is injured. Ferretti et al.9) reported that the cause of ISP muscle atrophy in volleyball players is a stretching neuropathy of the suprascapular nerve caused by repetitive hitting. In a study of professional male beach volleyball players, Lajtai et al.11) found significantly longer latency and lower amplitude in the suprascapular nerve in the ISP muscle of the hitting shoulder in both the total study group and in the subgroup with ISP muscle atrophy. Although we hypothesized that the majority of volleyball players may have a measurable neurological lesion of the suprascapular nerve in the hitting arm (resulting in ISP muscle atrophy), no significant differences were found in the latency and amplitude of the suprascapular nerve between the hitting and contralateral shoulders in the present study. These results are similar to those of Pieber et al.26) who found no significant differences in latency or amplitude between the hitting and contralateral shoulders of 20 high-performance beach volleyball players, although atrophy of the suprascapular innervated muscles was present in five players. Pieber et al. concluded that, because no lesion of the suprascapular nerve was found in any players on NCS or electromyography (EMG) investigations, either pain-induced disuse atrophy or secondary impingement syndrome as a result of damage or instability of the shoulder should be considered when infraspinatus muscle atrophy is present in volleyball players. In contrast, we found more than a 20% increase in latency of the ISP muscle (which suggested demyelination) in three players (13.6%), and one of these (4.5%) showed more than a 50% decrease in amplitude of the ISP muscle (suggesting an injury of the axons). However, these findings were not correlated with significant decreases in external rotation torque. Consequently, our findings suggest that the prevalence of suprascapular neuropathy in collegiate players may be less than that in high-level male professional volleyball players.
Correlations with Clinical FindingsIn this study, the impingement sign and RCT of the hitting shoulders were positive in five players (23%) and six players (27%), respectively. In particular, we found significantly lower external rotation torque in players with a positive impingement sign than in those with a negative impingement sign (P=0.048). It is possible that painful rotator cuff tendinopathy could influence the external rotation torque of the hitting shoulders, because RCT was also positive in three of the five players with a positive impingement sign.27)
Study LimitationsThe first limitation of this study is the small sample size; only 22 players were examined. Further studies with a larger number of subjects are needed to clarify the pathophysiology of the hitting shoulder in volleyball players. However, the results for the prevalence of pathological GIRD and the strength measurements are very similar to those of previous studies, suggesting that the population seems to be representative. Second, a limited range of visualization during ultrasonography may affect the measurement of the thickness of the rotator cuff muscle. Magnetic resonance imaging would be better than ultrasonography for quantifying and comparing the muscle thickness and volume and for evaluating other shoulder pathologies such as SLAP lesions, paralabral cysts, or thickened spinoglenoid ligament, which might contribute to muscle weakness, loss of ROM, and a suprascapular nerve lesion. A third potential limitation is that NCS alone was used to evaluate the suprascapular nerve in the SSP and ISP muscles. Better or more accurate results might have been produced by surface or needle EMG to evaluate denervation potential. Finally, rotator cuff tear, which may correlate with shoulder strength or infraspinatus muscle atrophy, was not evaluated in this study. Further studies are needed to elucidate the relation between internal impingement and shoulder muscle strength.
ConclusionThe prevalence of pathological GIRD in male collegiate volleyball players was consistent with the findings of previous studies, whereas the prevalence of suprascapular neuropathy was less than that previously reported in high-level volleyball players. Preventive posterior rotator cuff strengthening programs are recommended to correct imbalances between ER and IR in the hitting shoulder and to decrease the risk of shoulder injury.
The authors thank Yusuke Okubo, Yuri Oshima, Sho Noda, and Yusuke Matsuoka for their technical support and help in collecting the data in this study. Furthermore, we would like to thank Editage (www.editage.jp) for English language editing.
The authors have no conflicts of interest directly relevant to the content of this article.