2019 Volume 4 Article ID: 20190014
2019 Volume 4 Article ID: 20190014
Objective: Individuals with stroke frequently experience mobility deficits and limited community reintegration. This study aimed to investigate life-space mobility and relevant factors in community-living individuals with stroke. Methods: This was a cross-sectional study of 46 community-dwelling individuals with chronic stroke in Japan (mean age 72.7 ± 7.4 years; mean time post-stroke 63.6 ± 43.3 months; 26 men/20 women). We measured life-space mobility using a Japanese translation of the Life-Space Assessment. The following factors that might affect life-space mobility were assessed: the ability to perform activities of daily living, physical performance, fear of falling, and cognitive function. Results: A total of 41 participants (89.1%) had restricted life-space mobility (Life-Space Assessment score <60 points). A multiple linear regression analysis showed that limitations in activities of daily living, walking speed, and Falls Efficacy Scale-International scores were independently related to Life-Space Assessment scores. This model explained 51.3% of the variance in Life-Space Assessment scores. Conclusions: Most individuals with stroke had restricted life-space mobility. Life-space mobility was associated with the ability to perform activities of daily living, walking speed, and fear of falling. These findings could contribute to the development of rehabilitation interventions for regaining life-space mobility in individuals with stroke.
Stroke is a major cause of disability worldwide and the leading cause of long-term care needs in Japan.1) Mobility limitation is one of the most common problems following stroke; 39.2–82.3% of individuals with stroke have post-stroke limitations in community ambulation.2,3,4) Furthermore, reduced mobility is predictive of the future risk of deteriorations in health and functionality in community-living older adults.5,6) Therefore, the improvement of mobility is the primary rehabilitation goal for individuals with stroke.
Several measures have been used to estimate community mobility among stroke survivors. Self-reported mobility (which encompasses both mobility around the home and mobility in more distant and challenging environments) is an effective and simple outcome measure for clinical use.7) Life-space mobility is quantified using self-report measures of the spatial extent (range), frequency, and independence of mobility, from being confined to the bedroom to being able to access community facilities. Life-space mobility is associated with quality of life8,9) and self-reported health.9) Life-space mobility is the most frequently used measure in gerontology and is a valuable quantitative measure of social integration among community-living stroke survivors. Consequently, the investigation of life-space mobility after stroke and the identification of related factors could help clinicians to plan therapeutic interventions for extending life-space mobility post-stroke.
Many previous studies have shown that life-space mobility is mainly linked to physical performance,9,10,11) the ability to perform activities of daily living (ADL),9,10,11) cognitive function,9,10) and mental health9,10) in community-living older adults. However, only one study has examined in detail factors relevant to life-space mobility after stroke, demonstrating that physical performance, cognitive function, and falls efficacy predicted life-space mobility for stroke patients in Japan 2 months after hospital discharge.12) However, it is not known what factors are associated with life-space mobility in individuals with chronic stroke receiving long-term day care because of self-care disability. Thus, the principal aim of this study was to investigate life-space mobility after stroke and examine the relationship between life-space mobility and selected functionality and cognitive measures in community-living stroke survivors who were receiving long-term day care.
This was a cross-sectional observational study conducted between June and August 2013 in two daycare centers for older adults in Saitama, Japan. The study was approved by the Ethics Committee of the Saitama Cooperative Hospital (approval number 13–1–2). All participants gave informed consent prior to the study.
ParticipantsCommunity-living individuals with stroke who were receiving adult daycare services were recruited. Inclusion criteria were that participants (1) had had a stroke at least 6 months before the study; (2) had no musculoskeletal or neurological disorders other than stroke that affected their gait; and (3) could walk at least 16 m without physical assistance. Exclusion criteria were that participants (1) were younger than 50 years and (2) were unable to understand the instructions because of communicative or severe cognitive dysfunction as indicated by more than 5 out of 10 errors on the Short Portable Mental Status Questionnaire (SPMSQ).13) No statistical power calculation was performed prior to the study: the sample size was determined by the number of stroke individuals using the participating daycare services.
ProcedureData on demographics and stroke-related characteristics were obtained from patients’ medical records. All clinical assessments were conducted by two trained physical therapists. Scores for subjective performance measures were agreed upon by the two assessors.
MeasurementWe assessed life-space mobility using a Japanese translation of the Life-Space Assessment (LSA) (Table 1).14) The LSA was developed to measure the mobility status in older people.9) Our participants reported their mobility over the 4 weeks before assessment. Life space was categorized using 6 levels: 0=bedroom, 1=home, 2=outside the home, 3=neighborhood, 4=town, and 5=beyond the town. Participants were asked how often they spent time in locations at each level (less than once a week, 1–3 times a week, 4–6 times a week, daily) and how independent they were (whether they needed help from another person or used assistive devices). The LSA score ranges from 0 (totally bed-bound) to 120 (able to travel out of town every day without assistance). A score below 60 reflects restricted life-space mobility and indicates that participants generally remained at home or in their neighborhood.15) The LSA has shown excellent test–retest reliability.9)
| Life-space level | × | Frequency | × | Independence | |||
| 1: | Home | 1: | Less than 1/week | 1: | Help from another person | ||
| 2: | Outside the home | 2: | 1≤3/week | 1.5: | Equipment only | ||
| 3: | Neighborhood | 3: | 4 ≤6/week | 2: | No equipment or personal assistance | ||
| 4: | Town | 4: | Daily | ||||
| 5: | Beyond the town | ||||||
We assessed each participant’s ability to perform ADL using the Barthel Index (BI).16) This comprises ten ADL items divided into three subgroups: (1) personal care, including eating, dressing, personal hygiene, and bathing; (2) urinary and fecal continence; and (3) mobility, including transfers to and from the bed and the toilet, walking, and using stairs. We asked participants about their dependence level for each activity. This index has excellent interrater reliability in persons with chronic stroke.17)
Motor function in the lower extremities of individuals with hemiplegia was assessed using the Brunnstrom Recovery Stages (BRS).18) Participants were asked to perform voluntary movements of their lower limbs, and motor function was categorized as indicating 1 of 6 stages. The BRS has almost perfect interrater reliability in stroke patients.19)
Walking speed was measured using a 10-m walking test. Participants were asked to walk 16 m at their maximum speed using their usual assistive and orthotic devices. The time taken to walk the middle 10 m of the 16 m was measured using a digital stopwatch to calculate walking speed. This test has excellent test–retest reliability in persons with chronic stroke.20)
We evaluated cognitive impairment using the SPMSQ,13) which is a widely used 10-item cognitive examination that is useful for rapidly screening cognitive function. A score of 5 or more errors on the SPMSQ indicates moderate to severe cognitive impairment; a score of 3–4 errors indicates mild cognitive impairment; a score of 0–2 errors indicates cognitive intactness.14) The SPMSQ has shown good reliability and validity.21)
Fear of falling was evaluated using a Japanese translation of the Falls Efficacy Scale-International (FES-I).22) The FES-I is a 16-item questionnaire that asks respondents to assess their confidence in performing basic and instrumental ADL, walking outdoors, and going to social events or crowded places without falling.23) Each item is scored from 1 to 4 (1=not at all concerned and 4=very concerned); the total score therefore ranges from 16 to 64. A higher score indicates greater concern about falling. The FES-I has excellent internal and test–retest reliability.23)
History of falling was self-reported by participants, based on their recall of falls in the previous 12 months. Falls were defined as “an unexpected event in which the participants come to rest on the ground, floor, or lower level.”24) We classified participants as either with or without a history of falls.
Statistical AnalysesWe analyzed the data using SPSS, version 19.0 (IBM Japan Ltd., Tokyo, Japan). The Shapiro–Wilk test was used to examine the normality of variables. We used Pearson’s correlation to examine the relationships between the LSA score and the independent variables. For ordinal variables, including BRS of lower extremities, SPMSQ errors, and FES-I score, we conducted Spearman’s correlation analysis. An unpaired t test was used to assess the relationship between the LSA score and categorical variables.
We used stepwise multiple linear regression analysis to examine whether the potential factors were associated independently with the LSA score. Variables were entered into the regression model if their P value was less than 0.10 in a univariate analysis with the LSA score. The statistical significance level was P <0.05 for all analyses.
After excluding data from those participants aged less than 50 years (n=2) and those with cognitive dysfunction (SPMSQ >5; n=4), we analyzed data from 46 participants (26 of which were men). The average age of participants was 72.7 ± 7.4 years and the average time since stroke was 63.6 ± 43.3 months (Table 2). Two participants with double vision/spatial neglect were included in the statistical analysis because excluding their data did not affect the results. The mean LSA score was 42.1 ± 14.4, and 41 (89.1%) participants had restricted life-space mobility (Table 2 and Fig. 1).
| Mean ± SD or n | Median (interquartile range) | |
| Age (years) | 72.7 ± 7.4 | 73.5 (67–77.75) |
| Sex, male/female (n) | 26/20 | |
| BMI (kg/m2) | 24.0 ± 3.7 | 23.2 (21.6–26.1) |
| Type of stroke, ischemic/hemorrhagic (n) | 35/11 | |
| Paretic side, right/left (n) | 23/23 | |
| Time since stroke (months) | 63.6 ± 43.3 | 49.5 (32–90.5) |
| BI score (0–100) | 89.8 ± 10.1 | 90 (85–100) |
| BRS of lower extremity, 2/3/4/5/6 (n) | 2/16/8/3/17 | 4 (3–6) |
| Walking speed (m/s) | 0.70 ± 0.38 | 0.68 (0.38–0.94) |
| SPMSQ errors (0–10) | 1.8 ± 1.3 | 2 (1–3) |
| FES-I score (16–64) | 41.8 ± 10.7 | 43.5 (34–50) |
| Fall history, yes/no (n) | 19/27 | |
| LSA score (0–120) | 42.1 ± 14.4 | 39 (29.5–51) |
| Life-space restriction (LSA score <60, n) | 41 |
BMI, body mass index; BI, Barthel Index; BRS, Brunnstrom Recovery Stages; SPMSQ, Short Portable Mental Status Questionnaire; FES-I, Falls Efficacy Scale-International; LSA, Life-Space Assessment.
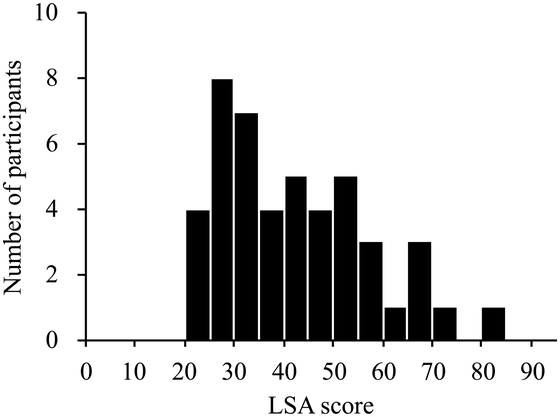
Distribution of Life-Space Assessment scores.
Table 3 shows the relationship between the LSA score and the other variables. There was a significant correlation between the LSA score and the BI score (r=0.715, P <0.001) and the LSA score and walking speed (r=0.584, P <0.001). There were no differences in LSA scores between men and women, the type of stroke, the side of hemiplegia, and individuals with or without a history of falling.
| Correlation coefficient | P | |
| Age | 0.129 | 0.392 |
| BMI | 0.085 | 0.576 |
| Time since stroke | –0.037 | 0.806 |
| BI score | 0.715 | <0.001 |
| BRS of lower extremity | 0.218 | 0.145 |
| Walking speed | 0.584 | <0.001 |
| SPMSQ errors | –0.125 | 0.408 |
| FES-I score | –0.259 | 0.083 |
We performed multiple regression analysis to determine whether the BI score, the walking speed, or the FES-I score were associated with the LSA score after stroke. The results are shown in Table 4. The factors retained in this model were the BI score (β=0.404, P=0.005), the walking speed (β=0.339, P=0.017), and the FES-I score (β=–0.224, P=0.039). Overall, 51.3% of the variance in the LSA score was explained by this regression model (F2,45=16.776, P <0.001).
| B | 95% CI | β | P | ||
| Lower limit | Upper limit | ||||
| BI score | 0.580 | 0.190 | 0.970 | 0.404 | 0.005 |
| Walking speed | 12.847 | 2.460 | 23.234 | 0.339 | 0.017 |
| FES-I score | –0.303 | –0.590 | –0.015 | –0.224 | 0.039 |
B, unstandardized regression coefficient; CI, confidence interval; β, standardized regression coefficient
This study used a linear regression model to investigate the association between life-space mobility and physical performance, cognitive function, psychosocial factors, and sociodemographic variables in community-living stroke survivors who were receiving long-term day care. Notably, the life-space mobility for most participants was restricted to the home or immediate neighborhood. The main study finding was that the ability to perform ADL, the walking speed, and the fear of falling were associated with life-space mobility in individuals with stroke. These results indicate that community-living individuals with stroke usually experience restricted life-space mobility. ADL ability, walking speed, and fear of falling are factors that may be important when considering how to improve life-space mobility in stroke survivors.
In this study, 89.1% of participants had restricted life-space mobility. This was higher than that found in previous studies of community-living adults (including those who had a stroke) aged 65 years or older (41.3%)25) and aged 75–90 years (41.0%).26) Moreover, the average LSA score for community dwelling older adults in the USA is 64.1 ± 24.9,10) and for Japanese older adults using preventive health care services, the average LSA score is 51.4 ± 25.2.14) The median score for stroke survivors 2 months after hospital discharge in Japan was 64 (quartiles, 41.5–96),12) which is higher than that for our participants. However, taken together, these findings indicate that most stroke survivors receiving long-term day care have limited community mobility. The above-mentioned results may have arisen from differences in the characteristics of the participants in that study;12) participants were younger (median age, 65 years; quartiles, 58–73 years) and had better lower limb function (median BRS, 5; quartiles, 4–6) than those in the present study. These factors may affect life-space mobility directly and/or indirectly through physical depression. Overall, restricted life-space mobility was a dominant factor for our participants, and the results suggested that regaining the ability to walk outdoors and reintegration into the community are important post-stroke rehabilitation goals even for individuals in the chronic stage of stroke recovery who are receiving long-term day care.
We found that walking speed was associated with life-space mobility among stroke individuals. Walking speed is a reliable, valid measure of mobility in individuals with stroke7) and is strongly associated with levels of community ambulation.2,3,27) Individuals with impaired walking ability resulting from stroke exhibit neuromotor problems.28,29,30,31) Slower walking speed is one of the most common problems in the stroke population32); this was confirmed in our participants. Furthermore, walking speed has been used as an important physical indicator of community ambulation levels of people with stroke.2,3,4,7) Therefore, improving walking speed should be prioritized in efforts to extend life-space mobility in stroke rehabilitation.
In this study, ADL performance was related to life-space mobility. This result is in accord with reports that ADL disability is negatively associated with life-space mobility in older adults.10,11) It is possible that ADL disability was one reason why our participants were disinclined to leave their homes. One literature review33) indicated improvements in ADL in stroke survivors from 3 to 12 months post-stroke, but no significant change in ADL from 1 to 3 years post-stroke. In addition, 12–40% of stroke survivors retained some ADL disability.33) Most of our participants experienced one or more difficulties with ADL, which may have reduced life-space mobility. We observed that an ability to perform ADL tasks is necessary to extend life-space mobility.
Our regression model indicated that greater fear of falling was associated with restricted life-space mobility. This result is in accord with previous findings that fear of falling leads to unnecessary avoidance of activities and social participation among elderly adults34,35) and among those with stroke.35,36,37,38,39) Tsai et al.40) reported fear of falling in almost 70% of community-dwelling stroke survivors, who also had related balance deficits41) and falls.40,41) Therefore, to optimize community reintegration, reduction of fear of falling should be a focus in rehabilitation settings. Notably, none of our study subjects stated that they were confident in carrying out all daily activities without falling. It is not known whether reducing fear of falling is effective in extending life-space mobility in community-living individuals with stroke. Future studies should examine whether exercises may reduce fear of falling and the effects of such programs on community reintegration.
Overall, we found that the ability to perform ADL, the walking speed, and fear of falling were associated with life-space mobility in individuals with stroke and accounted for 51.3% of the variance in LSA score; these components and the associated variance are similar to those identified in previous studies of community-dwelling elderly people10,11) and in stroke patients 2 months after hospital discharge.12) These findings could help therapists and community-dwelling individuals with chronic stroke to set clear and appropriate rehabilitation goals to regain community mobility. Moreover, routine monitoring of LSA and measurement of the relevant factors discussed here may help to encourage and/or maintain community mobility in stroke survivors.
The present study has several limitations. First, the study design was cross-sectional; consequently, we could examine only correlations between life-space mobility and the independent variables. We could not clarify whether the time since onset or since hospital discharge can affect life-space mobility in this population. Second, our sample comprised only elderly adults with chronic stroke receiving daycare services. Our findings cannot therefore be generalized to other populations of stroke survivors who are high functioning and independently living in the community. Third, LSA, BI, and history of falling were determined by retrospective self-reports. This method may have been affected by recall bias because some participants had mild cognitive impairment. Additional studies encompassing longitudinal analysis and involving more participants from a wider range of backgrounds are needed to investigate the determinants of life-space mobility.
Most of our participants had restricted life-space mobility. The findings indicated that restricted life-space mobility was associated with limitations in ADL, poorer physical performance, and fear of falling. Our findings may contribute to the development of comprehensive strategies to help individuals with chronic stroke reintegrate into the community.
The authors thank the participating facilities and their staff for cooperation and assistance in data collection. We thank Diane Williams, PhD, from Edanz Group (www.edanzediting.com/ac) for editing a draft of this manuscript.
The authors declare no conflicts of interest.