2020 年 5 巻 論文ID: 20200017
2020 年 5 巻 論文ID: 20200017
Objective: There are no reports describing in detail postoperative rehabilitation after double-level osteotomy (DLO). Consequently, the establishment of a safe and effective rehabilitation protocol is required.
Methods: This retrospective study included 26 patients with varus knees who underwent DLO. No patient had obvious fracture around the femoral osteotomy sites, as evaluated using computed tomography (CT) 3 weeks postoperatively. From 3 days postoperatively, gait training with early weight bearing was performed using our parallel bar protocol. Range of motion exercises were permitted as tolerated. Radiological evaluation was performed to confirm the presence or absence of fracture around the femoral osteotomy sites using CT at 3 weeks and X-ray at 6 weeks postoperatively. X-ray imaging 6 months postoperatively indicated no femoral correction loss. Additionally, the time from initiation to completion of the protocol and the time from initiation to achievement of independent gait were recorded.
Results: No fractures around the femoral osteotomy sites in any patient were found using CT 3 weeks postoperatively and X-rays 6 weeks postoperatively. There was no correction loss at the femoral osteotomy site according to X-ray findings 6 months postoperatively. The mean time until completion of the parallel bar protocol was 19.8 ± 6.2 (7–30) days, and that from the initiation of rehabilitation to the achievement of independent gait was 26.8 ± 7.1 (16–45) days.
Conclusion: Patients without fracture around the femoral osteotomy site during the rehabilitation period could achieve independent gait within an average of <1 month using the parallel bar protocol. Early weight-bearing walking and independent walking could be achieved using this protocol.
In patients with varus knee, both the femur and tibia are occasionally deformed. In such cases, single osteotomy may result in extreme joint-line obliquity,1) thereby increasing the shear stress at the joint surface2) and resulting in a new bony deformity. Consequently, in recent years, double-level osteotomy (DLO) has attracted the attention of knee surgeons and has been reportedly useful in preserving physiological articular surface tilt (Fig. 1).3,4,5)
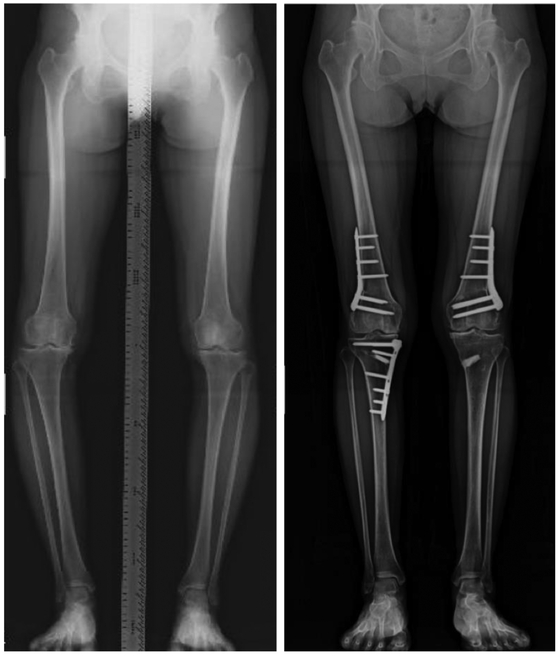
Osteotomy around the knee. Depending on the locations of varus and valgus deformities, the medial and lateral osteotomy sites differ in distal femoral osteotomy cases. In DLO cases, most patients presented genu varum. Consequently, in addition to distal femoral osteotomy through a lateral approach, medial, open-wedge, high tibial osteotomy was performed.
Early weight bearing starting several days after medial, open-wedge, high tibial osteotomy (MOWHTO) has become common and has proven to be safe.6,7,8,9) Additionally, several reports have described the timing for initiating weight-bearing gait training in rehabilitation after distal femoral osteotomy (DFO).10,11,12,13) In these studies, early weight-bearing gait training was not recommended, and weight bearing was restricted for as long as 3–4 weeks after surgery. Therefore, long-duration restricted weight bearing is an important issue.
According to our recent literature search, no reports have described postoperative rehabilitation for DLO in detail. Therefore, a routine, safe, and effective rehabilitation protocol is needed. In 2016, we established a standardized parallel bar protocol at our hospital that can be used after osteotomy around the knee, including DLO. Early weight-bearing gait rehabilitation is allowed in this protocol. Therefore, the purpose of this study was to clarify the time required to complete our aggressive early rehabilitation program and to clarify the time required to achieve independent walking for patients who underwent DLO and suffered no postoperative correction loss using this rehabilitation program.
This study was conducted at the Department of Orthopedic Surgery of Toyokawa City Hospital. The Institutional Review Board of the Ethics Committee at our institution approved the study protocol (approval number: 85), which was carried out in accordance with the Helsinki Declaration, 1964. Written informed consent was obtained from all individuals participating in this study.
Initially, 27 patients who underwent DLO between February 2016 and December 2018 were included. However, one patient was excluded because fracture around the femoral osteotomy site was detected by intraoperative fluoroscopy imaging and postoperative computed tomography (CT). As a result, 26 patients were included in this study.
Indication of SurgeryThe indications for DLO were patients with varus malalignment of the leg who, despite conservative treatment, had persistent pain because of medial compartment knee osteoarthritis. DLO combined with MOWHTO was determined when the planning of an MOWHTO indicated a medial proximal tibia angle of more than 95° or when there was a deformity of the lateral distal femoral angle of more than 90°. Patients with a history of infectious knee disease, rheumatoid arthritis, or flexion contracture of more than 15° were excluded.
Preoperative EvaluationPatient demographics are shown in Table 1. The severity of knee osteoarthritis was evaluated using the Kellgren–Lawrence radiographic grading scale.14)
| Parameter | All cases (n=26) |
| Sex (male/female) | 15/11 |
| Age | 60.2 ± 4.7 (53–68) years |
| Height | 159.7 ± 7.0 (148.9–179.8) cm |
| Body weight | 68.5 ± 11.0 (50.5–83.0) kg |
| Body mass index | 26.7 ± 2.9 (21.3–31.3) |
| Total correction angle | 14.2° ± 2.8° (11.2°–19.0°) |
| Femoral correction angle | 5.0° ± 1.2° (3.6°–8.2°) |
| Kellgren–Lawrence grade | |
| Grade II | 3 cases |
| Grade III | 18 cases |
| Grade IV | 5 cases |
Values are expressed as mean ± standard deviation (range).
Surgical planning was performed with the postoperative hip–knee angle set to 2° valgus, the medial proximal tibia angle in the range 90°–94°, and the lateral distal femoral angle in the range 85°–89°. Routine arthroscopic debridement was performed before DLO in all cases. No chondral transplantation was performed.
We performed lateral closed-wedge DFO first in all DLO cases using the biplanar technique developed by a Dutch working group organized by van Brinkman et al.3,12) The contralateral side of a TomoFix Medial Distal Femur plate (DepuySynthes; Solothrun, Switzerland) was bent to fit the lateral femoral cortex after lateral closed-wedge DFO. This plate was set beneath the vastus lateralis muscle, and bridging plating was performed. No suction drain was placed, and the surgical incision was closed in layers. Following DFO, the MOWHTO procedure described by Staubli et al. and Lobenhoffer et al.15,16) was performed to additionally correct the varus deformity. Further, a block (Bonish, NGK SPARK PLUG, Nagoya, Japan) was prepared to fit the pre-planned open-wedge site.
Postoperative Radiological EvaluationAnteroposterior knee X-ray images were taken immediately after surgery to detect the presence of any femoral osteotomy site fracture. CT (SOMSTOM Definition AS+, Siemens, Erlangen, Germany) was performed 3 weeks after surgery to determine whether a fresh fracture had occurred at the femoral osteotomy site. Routine radiological evaluation was performed at 6 weeks and 6 months after surgery to assess the level of correction loss, any newly developed fracture, or femoral implant failure (Fig. 2).
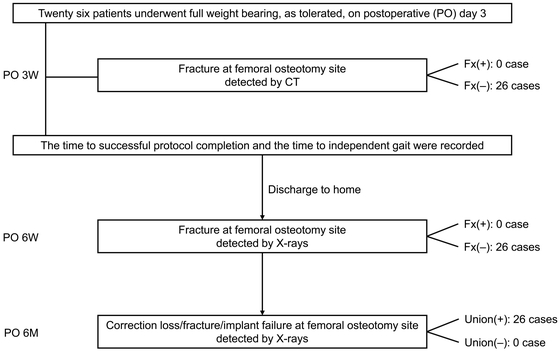
Patient flow chart.
Active range of motion exercises and muscle strengthening were permitted, as tolerated, on the first day after surgery. Early weight-bearing gait training was permitted using the parallel bar protocol on day 3 after surgery. Load-bearing training was stopped if any femoral fracture was detected on CT performed 3 weeks after surgery, in which case, patients were instructed not to put their weight on the affected limb until callus formation was observed on X-ray images.
The height of the parallel bars was set according to patient’s height, i.e., located between the superior anterior iliac spine and the greater trochanter. The distance between the parallel bars was consistently set at 562 mm.
Parallel Bar ProtocolThe parallel bar protocol comprised the six phases described below (Figs. 3 and 4).
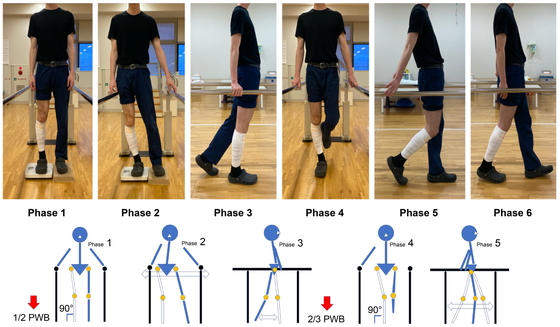
Parallel bar protocol (right leg underwent surgery). With the concept of “simple content that can be understood by anyone,” we created six subcategories covering each phase of stance and gait. The utmost importance was placed on straightening the leg in the stance phase, and in all phases, if gait disturbance occurred, the subject was instructed not take another step, and form acquisition was reinforced.

Straightening of the leg (right leg underwent surgery).
Phase 1: The goal was to apply at least half partial-weight bearing (PWB) on the operated side while standing.
Phase 2: The goal was to achieve lateral pelvic movement in a standing weight-bearing position with, as far as possible, no twisting of the trunk, pelvis, or lower limbs and to acquire lateral movement to the extent of the patient hitting their pelvis on the parallel bars simply by shifting their center of gravity laterally.
Phase 3: The goal was to sense the midstance from the initial contact and to be able to apply weight-bearing to approximately 2/3 PWB on the operated side.
Phase 4: With the aim of standing on one leg, to enable smooth transition from the midstance to the late stance phase, the goal was to stand on one leg while holding the bar with one hand.
Phase 5: The goal was to sense the initial swing phase from the midstance and acquire a stable form while holding the handrail.
Phase 6: The goal was to be able to walk the length of the parallel bars without disturbance of the gait acquired in phases 1–5.
The importance of straightening the leg in the stance phase and avoiding the stress of femoral torsion over the entire process was emphasized to all patients. When gait disturbance occurred, the subject was instructed to stop, and form acquisition was reinforced.
Furthermore, when exacerbation of pain was evident, the subject was not pushed to overdo it and was instructed not to take another step; the protocol phase was then maintained at a level at which there was no pain exacerbation, and once the pain was relieved, the subject proceeded to the next phase.
Clinical EvaluationSuccessful completion of the parallel bar protocol was defined as the time at which the patient accomplished phase 6, i.e., being able to walk stably the length of the parallel bars. Independent walking was defined as the time at which the patient was able to stably walk without any walking aid, such as a cane.
Clinical examinations comprised both subjective and objective parameters using the Japanese Knee Osteoarthritis Measure (JKOM) and the Japanese Orthopaedic Association score for osteoarthritic knees (JOA). Additional clinical and radiological assessments included the range of motion and possible postsurgical correction loss. These evaluations were conducted before surgery and 6 months postoperatively (Table 2).
| Preoperative | Postoperative at 6 months |
P-value | |
| JKOM | 41.7 ± 19.3 (18–68) | 20.8 ± 7.8 (11–41) | <0.001 |
| JOA | 74.8 ± 11.6 (50–95) | 86.5 ± 6.8 (75–95) | <0.001 |
| Range of knee extension | −3.3° ± 4.3° (−10° to 5°) | −0.8° ± 1.9° (−5° to 3°) | <0.001 |
| Range of knee flexion | 136.9° ± 12.5° (95°–150°) | 140.0° ± 8.7° (120°–155°) | 0.160 |
| Total arc of range of motion of knee | 134.1° ± 13.2° (95°–150°) | 139.5° ± 10.0° (100°–153°) | 0.015 |
| Medial proximal tibial angle | 83.3° ± 2.6° (79.8°–86.7°) | 91.6° ± 1.1° (90°–93.3°) | |
| Lateral distal femoral angle | 91.1° ± 1.7° (88.2°–95.4°) | 85.7° ± 1° (84.1°–88.3°) | |
| Hip–knee angle | −8.8° ± 2.5° (−10.4° to −2.4°) | 1.8° ± 0.9° (0.8°–3.7°) valgus |
We investigated postoperative correction loss using Morland’s method.17) Two points in the middle of the femoral medulla were marked. Then, the line connecting these two points was drawn and extended distally to cross the articular surface line. The angle between the two lines (α angle) was measured immediately after surgery and 6 months postoperatively. The difference between the two α angles was defined as the correction loss (Fig. 5).
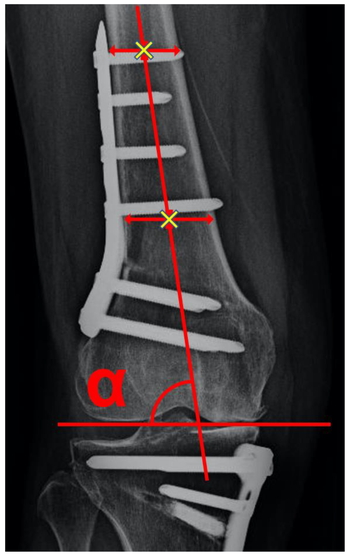
Method for measuring the α angle. Two points in the middle of the femoral medulla were marked (×). The line connecting these two points was then drawn and extended distally to cross the articular surface line. The α angle was the angle formed by these two lines.
Data are presented as the mean ± standard deviation (range). The correlation between the time until independent gait was achieved and the body mass index (BMI) or the total correction angle was analyzed using Spearman rank-order correlation. Comparisons of parametric factors between groups were evaluated using paired t tests. P <0.05 was considered significant. All statistical analyses were performed using EZR software (http://www.jichi.ac.jp/saitama-sct/SaitamaHP.files/statmed.html).
No fracture or implant failure at the femoral osteotomy site was observed on radiological evaluation using CT at 3 weeks and X-rays at 6 weeks and 6 months postoperatively in any of the 26 patients. Furthermore, postoperative physiotherapy and weight-bearing walking training was not delayed in any patient because of pain. To complete the parallel bar protocol took 19.8 ± 6.2 (7–30) days after surgery. Furthermore, it took an average of 26.8 ± 7.1 (16–45) days after surgery to achieve walking without any aid (Table 3). There were no significant correlations between the time until independent gait and BMI (r=−0.114, P=0.536) or the total correction angle (r=0.324; P=0.070). Significant improvements concerning patient-reported outcome measures and clinical evaluations such as the JKOM (41.7 ± 19.3 vs. 20.8 ± 7.8; P <0.001), the JOA score (74.8 ± 11.6 vs. 86.5 ± 6.8; P <0.001), the range of knee extension (−3.3° ± 4.3° vs. −0.8° ± 1.9°; P <0.001), and the total arc of knee range of motion (134.1° ± 13.2° vs. 139.5° ± 10.0°; P=0.015) were observed between the preoperative and 6-month postoperative measurements. There was no significant correlation between the α angle immediately after operation and at 6 months postoperatively (Table 4). One case of wound infection at the tibial site was diagnosed 3 months postoperatively and was successfully treated with oral antibiotics.
| All cases (n=26) | |
| Number of days required for completion of the parallel bar protocol | 19.8 ± 6.2 (7–30) days |
| Number of days required until independent gait was achieved | 26.8 ± 7.1 (16–45) days |
| Patients with fracture observed using CT on POD 21 | 0 |
| Patients with complications on anteroposterior and lateral X-ray images at 6 weeks and 6 months after surgery | 0 |
Values are expressed as mean ± standard deviation (range).
A mean of 35.3 days postoperatively was required before discharge; the shortest time to discharge was post-operative day (POD) 21.
| Immediately after operation | Postoperative at 6 months |
P-value | |
| α angle | 79.6° ± 2.7° | 79.8° ± 2.6° | 0.154 |
Values are expressed as mean ± standard deviation.
The most important findings of the present study were that load-bearing training could be started 3 days postoperatively, and independent walking could be achieved within 1 month using the parallel bar protocol under the condition of no fractures at the femoral osteotomy site.
Patients who underwent this protocol were able to walk independently without any aid within an average of 27 days after surgery. CT was performed 3 weeks after surgery, and multi-planar reconstruction images were used to detect any fractures at the femoral osteotomy site. We found no fractures in these sequences, and all 26 patients successfully completed the protocol. X-ray images taken at 6 weeks and 6 months after surgery showed no delayed union, no correction loss, and no newly developed fracture in any of the 26 patients. According to our recent literature search, this article describes one of the first loading rehabilitation protocols for DLO.
Regarding MOWHTO, Brinkman et al. reported that TomoFix plate-fixated, open-wedge, high tibial osteotomy allowed early full weight bearing without loss of correction. The patients in the early weight-bearing group achieved the same clinical outcomes within a shorter time than those following the standard rehabilitation protocol.18) To our knowledge, no report has yet described weight-bearing gait training that commenced 3 days after DFO and DLO.1,2,3,4,5,6,7,10,11,12,13)
The benefits of shortening the unloaded period are considered to be significant in several past reports. Early loading can reduce the risk of developing deep vein thrombosis19,20) and prevent muscle weakness. However, there is a certain concern regarding newly developed fractures caused by loading and associated correction loss, thereby resulting in delayed union.
Concerning the safety and efficacy of rehabilitation using parallel bars, patients with cerebral infarction and lower limb amputation who cannot walk stably frequently undertake rehabilitation with this equipment and are able to safely perform activities such as walking training and unilateral leg standing; moreover, the frequency of use and the safety of parallel bars have already been established.21)
There were no significant correlations between the time required to achieve independent gait and BMI or total correction angle in our patient cohort. However, compared with the preoperative stance, the postoperative stance was different after osteotomy.22) Furthermore, postoperative lower limb alignment in most patients who underwent DFO and DLO changed significantly after surgery. Therefore, providing a safe environment using parallel bars for these patients is important in terms of safety. Performing gait training with simple set tasks to reacquire smooth weight shift in each phase of standing and walking is safe and efficient for postoperative patients. The transition distance of the parallel bar protocol is short; consequently, it is easy for patients to perform repetitive training. Visual feedback using a mirror and advice to the patient from the physical therapist on ideal movement patterns are likely to improve the effectiveness of rehabilitation.23,24,25)
In our institution, parallel bar protocol rehabilitation is applied to all patients who undergo osteotomy around the knee, regardless of the type of surgical procedure. This protocol comprises separate training for the standing phase and the walking phase. Emphasis is placed on straightening the leg during the entire protocol. To enable a smooth transition to full-scale gait training, we aimed for patients to obtain a sense of the shift in their center of gravity in an environment that reduces the fear of weight bearing and eliminates torsion as much as possible. Biplane-cut DFOs are reportedly able to resist axial pressure better than single-plane cut DFOs. However, biplane-cut DFOs are less resistant to torsional forces.26) Therefore, it is important to reduce torsional stress to prevent new fractures and postoperative correction loss. The extent to which the lower leg is aligned vertically can be easily assessed by a physiotherapist or other health professional, both subjectively and objectively.
There were several limitations in this study. First, it was a retrospective study at a single institution without a control group using the same protocol. Second, it was not a randomized trial. Randomization in postoperative rehabilitation is difficult to achieve in a single institution. This report describes a pilot study, and the sample size was not adequate for robust evaluation. Therefore, the results obtained in this study cannot be applied to all osteotomy patients treated with other procedures and fixation implants.
In conclusion, gait training was performed with early weight bearing using our parallel bar protocol, and all patients were able to acquire full-load walking without complications. In the future, it will be necessary to increase the number of subjects and verify the safety of this protocol.
We thank Tsuneari Takahashi MD, PhD, and Crimson Interactive Pvt. Ltd. (Ulatus, www.ulatus.jp) for their assistance in manuscript translation and editing.
The authors declare that there are no conflicts of interest.