2022 Volume 7 Article ID: 20220017
2022 Volume 7 Article ID: 20220017
Background: Esophageal cancer is increasing in incidence in Japan and is usually treated by radical surgery. However, pulmonary complications are a major cause of perioperative mortality. Here we report a case in which bilateral pneumothorax after thoracoscopic esophagectomy was managed successfully by a combination of chest physiotherapy, mobilization, and delayed oral intake.
Case: The patient was a 72-year-old man with a diagnosis of lower thoracic esophageal cancer and a medical history that included chronic obstructive pulmonary disease. He underwent thoracoscopic and laparoscopic subtotal esophagectomy and two-field lymphadenectomy. On postoperative day (POD) 1, he was diagnosed as having bilateral pneumothorax. An additional drainage tube was inserted in the right chest. Chest physiotherapy was started using a combination of methods, including diaphragmatic breathing, respiratory muscle stretching, and postural drainage. Mobilization was started on POD 2 but was limited to sitting upright and standing. On POD 5, gentle walking training (Borg Scale score, 9–11) was started when air leakage from the drain was observed only during expiration. Oral food intake was resumed on POD 9, by which time the pneumothorax had resolved completely. The patient was discharged on POD 27 with near-complete independence in activities of daily living.
Discussion: We successfully managed the rehabilitation of a patient diagnosed with bilateral pneumothorax after esophagectomy. In a tailored strategy, we took the following measures to avoid worsening the pneumothorax and other surgery-related pulmonary complications: chest physiotherapy, avoiding procedures that increase intrathoracic pressure; delayed mobilization and reduced intensity of exercise; and delayed oral intake.
The incidence of esophageal cancer in Japan has increased in recent years.1) Radical surgery with curative intent is typically performed for esophageal cancer2,3) but is complex and highly invasive. Esophagectomy has high perioperative mortality, with a recent review reporting a 30-day mortality rate of 2.4%–5.0%.4) Pulmonary complications are the most common cause of perioperative mortality in these patients5) and result in prolonged hospitalization, increased medical costs, and compromised quality of life.6) Therefore, a perioperative rehabilitation strategy that prevents or alleviates pulmonary complications is critical for good prognosis after surgery for esophageal cancer.7)
Rehabilitation for pulmonary complications includes a physiotherapy regimen of postural drainage, manual hyperinflation, breathing exercises, and training of respiratory muscles.7) These procedures can be expected to prevent alveolar collapse and improve airway clearance and gas exchange.7) However, such treatments may increase intrathoracic pressure, which should be avoided in cases of pneumothorax.8)
We encountered a patient who developed bilateral pneumothorax after surgery for esophageal cancer. A pneumothorax is rare as a pulmonary complication after esophageal cancer surgery, accounting for about 0.6% of all pulmonary complications.9) Therefore, it requires careful attention in rehabilitation management. Although there are few reports about pulmonary rehabilitation for perioperative bilateral pneumothorax and no established rehabilitative protocols, ongoing evaluation and implementation of an individualized program are important.10) Herein, we report the successful rehabilitation management implemented in this case.
A 72-year-old man who was fully independent in activities of daily living (ADL) was referred to our university hospital for detailed examination of an esophageal tumor detected at a local community hospital. Written informed consent was obtained from the patient for publication of this report. He had no symptoms related to the tumor. He had smoked 20 cigarettes per day for approximately 50 years and was a heavy drinker. His comorbidities were chronic obstructive pulmonary disease, diabetes mellitus, atrial fibrillation, hypertension, and hyperlipidemia.
The patient underwent upper gastrointestinal endoscopy and was diagnosed as having esophageal cancer. Computed tomography (CT) revealed a tumor with thickening of the wall in the lower portion of the esophagus (Fig. 1). Lymphadenopathy was detected in the mediastinum. Superimposition of images obtained by positron emission tomography on the CT images indicated accumulation of fluorodeoxyglucose in the tumor (Fig. 1). The cancer was classified as a stage II squamous cell carcinoma (T2N1M0).2,3) The patient was scheduled to receive three courses of neoadjuvant chemotherapy followed by radical esophagectomy with curative intent.
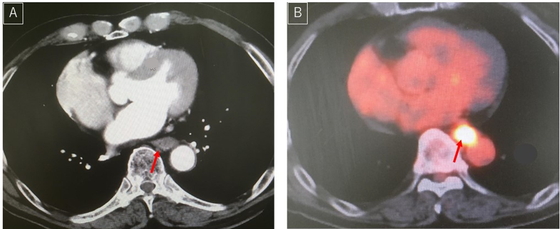
Images acquired for diagnosis of esophageal cancer. (A) Computed tomography image showing a tumor and thickening of the wall in the lower portion of the esophagus (red arrow). (B) Superimposition of a positron emission tomography image on a computed tomography image shows accumulation of fluorodeoxyglucose in the area corresponding to the tumor (red arrow).
Perioperative rehabilitation was started 3 days before surgery. In the preoperative stage, the patient showed no signs of acute distress other than mild tachycardia (106 beats/min) caused by atrial fibrillation. He had a body mass index of 23.1 (weight 70.0 kg, height 174 cm) and a full range of motion in the upper and lower extremities. His grip strength was 32.8 kg on the right and 38.4 kg on the left. The knee extension strength was 34.2 kg and 30.3 kg on the right and left sides, respectively. The 6-min walking distance was 451 m. Laboratory investigations indicated mild renal dysfunction (creatinine clearance 57.4 mL/min), mild anemia (hemoglobin 11.1 g/dL), and hypoalbuminemia (albumin 3.3 g/dL). Respiratory function tests showed obstructive lung disease with a vital capacity of 81.5% of the predicted value and a forced expiratory volume in 1 s that was 65.1% of the forced vital capacity. The percent predicted forced expiratory volume in 1 s was 40.5%. Echocardiographic findings were within normal limits except for atrial fibrillation. The Functional Independence Measure (FIM)11) score (an indicator of ADL performance) was 126 (full score), with scores of 91 for the motor component and 35 for the cognitive component.
Thoracoscopic and laparoscopic subtotal esophagectomy with two-field lymphadenectomy and construction of a trans-gastrointestinal fistula were performed uneventfully. After the operation, the patient was admitted to the intensive care unit (ICU) for ventilatory support with placement of right chest and cervical drains. A small air leak from the chest drain was detected at this time. The patient was extubated on postoperative day (POD) 1. The maximum phonation time12) was 13 s and there was no hoarseness. Bronchoscopy showed no obvious sign of a bronchial fistula. Approximately 5 h after extubation, subcutaneous emphysema was observed upon palpation but no respiratory exacerbation was observed. A CT scan of the chest revealed bilateral pneumothorax and mediastinal emphysema (Fig. 2). A second right chest drain was inserted, and a persistent air leak was detected during both inspiration and expiration. There was only mild collapse of the left lung, and no chest drain was inserted on that side. Given that the patient was in postoperative recovery from a highly invasive procedure and his respiratory status was maintained, we decided to continue chest drainage without surgery for bilateral pneumothorax.
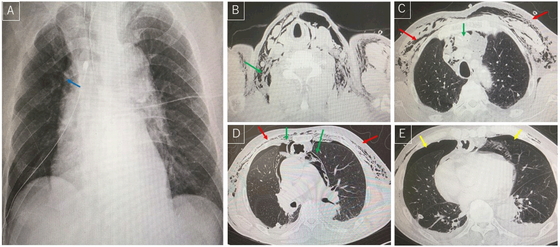
Radiographical findings obtained on postoperative day 1. (A) Plain radiograph showing an air space line on the right side of the mediastinum (blue arrow). (B–E) Computed tomography images showing mediastinal emphysema (green arrows), subcutaneous emphysema (red arrows), and pneumothorax (yellow arrows).
Figure 3 shows the patient’s postoperative clinical course. Physical therapists implemented chest physiotherapy that included diaphragmatic breathing, respiratory muscle stretching, and postural drainage. We avoided the use of aggressive expectorant procedures, such as manual hyperinflation and thoracic compression. Chest physiotherapy was performed with continuous monitoring of the respiratory pattern, the volume of air leakage in the chest drainage bag, and the degree of oxygen saturation recorded by pulse oximetry. Plain radiographs were obtained daily to assess the extent of the pneumothorax.
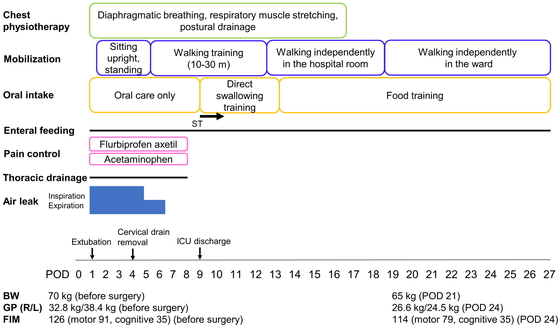
Clinical course after surgery. BW, body weight; GP, grip power; ST, swallowing training by a speech therapist.
Mobilization proceeded under the same observation conditions. There was a large volume of air leakage from the chest drains during both inspiration and expiration until POD 4. During this time, we limited the mobilization protocol to sitting upright and standing (Fig. 3). Walking training was started on POD 5 when air leakage was only observed during expiration. An electrocardiogram and respiratory movement were monitored continuously in the ICU. The intensity of walking training was set at 20%–30% of the heart rate reserve (equivalent to a Borg Scale score of 9–11).13) Flurbiprofen axetil and acetaminophen were administered for pain control to promote mobilization and to facilitate the removal of devices (e.g., drainage tubes). On POD 7, the air leak was no longer observed and the pneumothorax had resolved satisfactorily. All drains were removed on POD 8. On POD 9, the patient was transferred from the ICU to a regular ward, where he was able to walk independently by POD 18.
To minimize the risk of aspiration, oral feeding was withheld until the pneumothorax improved, with only oral care provided by nurses in the meantime. Enteral feeding was started via an enterocutaneous fistula on POD 1. Direct swallowing training was started by a speech therapist on POD 9, and oral intake of meals (three times a day) was started on POD 12. Laryngeal endoscopy on POD 22 showed no laryngeal nerve palsy. The patient resumed oral intake of food with a full porridge texture. Because of low oral intake, supplemental enteral feeding via the enterocutaneous fistula was continued until discharge.
By POD 21, the patient’s weight had decreased to 65.0 kg (body mass index 21.5). By POD 24, his grip strength had decreased to 26.6 kg on the right side and 24.8 kg on the left side. However, the patient’s ADL performance had recovered to near-full independence by this time; the FIM score was 114 (motor component, 79; cognitive component, 35). The patient was discharged home on POD 27.
This report describes a rare case of bilateral pneumothorax after esophagectomy. In this case, we needed to implement effective rehabilitation while preventing exacerbation of the pneumothorax. Careful consideration was needed before implementing therapeutic procedures, which included chest physiotherapy, graded mobilization, and gradual resumption of oral intake. Thoughtful rehabilitation management was successful in allowing this patient to achieve almost full recovery in terms of ADL without exacerbation of the pneumothorax or other serious complications.
Effective airway clearance by chest physiotherapy is important in postoperative pulmonary rehabilitation after esophagectomy.7) Some studies have examined the role of chest physiotherapy after esophagectomy and reported its benefits after both open and laparoscopic surgery.14,15) A retrospective review of 70 patients found that the incidence of pulmonary complications was lower in patients who received chest physiotherapy following esophagectomy than in those who did not receive such treatment.15) Manual hyperinflation is contraindicated in patients with a pneumothorax without thoracic drainage.16) Furthermore, manual chest compression and some breathing exercises (e.g., huffing) may exacerbate a pneumothorax. In our case, the maximum phonation time, which reflects cough strength,17) was well maintained. Accordingly, we decided to avoid expectorant procedures and tailored our chest physiotherapy procedures to the specific needs of our patient.
The ERAS (Enhanced Recovery after Surgery) guidelines recommend early mobilization, starting on the day of surgery whenever feasible.18) Although mobilization goals vary across different clinical pathways, recommendations for POD 1 range from sitting out of bed for 2 h or longer to short (e.g., 10-m) walks. In our case, air leakage on both inspiration and expiration from the chest drains persisted until POD 4. Being concerned that aggressive mobilization might exacerbate the pneumothorax in this patient, we decided to start walking training with reference to the extent of the air leak. We applied pain control and removed devices as early as possible to facilitate comfortable early mobilization.7) At this stage, we needed to decide on the intensity of training. A case-control study had indicated that moderate aerobic exercise is effective in the early postoperative period.19) However, we found that there was no consensus regarding the intensity of physical exercise, including walking training. Therefore, to avoid exacerbation of the pneumothorax, we started walking training at a very mild level (Borg Scale score, 9–11).
Some studies have found that early oral intake after esophagectomy (starting from POD 1) promotes recovery of bowel function and decreases the likelihood of rehospitalization.20,21) However, a recent review found no difference in complications or morbidity between early oral intake and delayed oral intake with supplemental feeding (starting from POD 6–15).22) Moreover, the ERAS guidelines do not make a recommendation regarding the appropriate time to start oral intake.4) Accordingly, in this case, we implemented only oral care until oral intake was started on POD 9 after complete resolution of the pneumothorax.
The rehabilitation strategy outlined in this report has some limitations. First, it was difficult to quantify the severity of the bilateral pneumothorax. Most cases of pneumothorax are unilateral, and their severity is assessed by the degree of lung collapse on a chest radiograph.8) However, there is no tool that can be used to assess the severity of bilateral cases. Second, our patient did not recover fully in terms of physical function, as assessed by grip strength and FIM score. The neoadjuvant chemotherapy administered in this 72-year-old man had a minimal effect on his physical performance. The decrease in physical performance after surgery might reflect delayed mobilization and the low intensity of walking training. Third, it is not possible to compare the effectiveness of our procedure with that of other methods based on a case report. Very few publications have reported rehabilitative treatments for bilateral pneumothorax, and there are no established protocols for this treatment. Therefore, we elected to personalize some existing therapeutic procedures depending on the patient’s condition and complications.10,23) Given the rarity of bilateral pneumothorax after esophagectomy, there is a need to accumulate further case reports. Despite these limitations, this report describes an example of successful rehabilitative management after esophagectomy in the presence of bilateral pneumothorax.
The authors thank the staff in the Department of Rehabilitation Medicine and the Department of Upper Gastrointestinal Tract Surgery, Hyogo College of Medicine Hospital, for their assistance with this research.
The authors report no conflicts of interest.