2022 年 7 巻 論文ID: 20220020
2022 年 7 巻 論文ID: 20220020
Background: There are no reports on the therapeutic application of perceptive exploration activity in patients with unilateral spatial neglect (USN). This study monitored the course of acute occupational therapy using perceptive exploration activities in a patient with USN who had difficulty in manipulating tools for daily living after a stroke.
Case: A 70-year-old man was admitted to our hospital for conservative treatment of hemiparesis and USN caused by stroke. He was previously diagnosed with cerebral infarction due to middle cerebral artery occlusion. His main symptoms were hemiparesis, egocentric spatial neglect in personal space and peripersonal space, and allocentric neglect, which made it difficult to use tools for daily living. Within 24 h of admission, perceptive exploration activities were initiated as the main therapy in addition to preparatory therapies, such as the facilitation of selective movement of limbs affected by paralysis. These therapies were provided over a 30-day period in 40-min sessions, 5 days a week. This treatment resulted in improved test results for the Fugl-Meyer Assessment, Bisiach’s body neglect and anosognosia scales, and the Behavioral Inattention Test. The Functional Independence Measure scores also improved with the improvement of neglect symptoms.
Discussion: This case study monitored the improvements of egocentric spatial neglect and allocentric neglect during therapy using perceptive exploration activities in a patient with USN who had difficulty manipulating tools for daily living. The effectiveness of the therapy should be confirmed by increasing the sample size in future studies.
Unilateral spatial neglect (USN) occurs in up to 85% of patients that show neurological disorder after subacute phase right hemisphere stroke.1) It is characterized by difficulty in exploring and responding to stimuli on the opposite side of the brain lesion.2) The poor exploratory response to self and the environment caused by USN affects re-adaptation to activities of daily living (ADL) and social life. USN occurs in the personal space (self-body that is visually recognizable by ADL), the peripersonal space (reachable space around the self-body), and the extrapersonal space (distal space).3,4) Neglect is classified into egocentric spatial neglect (space on the left side is ignored) or allocentric neglect (the left part of the object with reference to the entire object is ignored, and each expression mode is different) according to the presentation of reaction stimuli.5,6) Egocentric spatial neglect is associated with damage to the frontoparietal lobe network, whereas allocentric (object-based) neglect is associated with damage to the temporoparietal lobe network.7)
Rehabilitation for USN still lacks effective therapeutic strategies. For example, the Japanese Stroke Guidelines 2015 recommend a grade B impairment-oriented approach and self-care training.8) Impairment-oriented approaches include visual search training, presentation of clues to the neglected space, and prism adaptation; however, the involvement of improved USN with improved ADL function is unclear.9,10,11,12) In self-care training, a repetitive task is recommended to help acquire compensatory movement rather than to facilitate recovery from USN.13) However, these therapies are intended for egocentric spatial neglect rather than allocentric neglect. Given that 60% of USN cases show allocentric neglect, it is necessary to devise therapy focusing on an individual’s pathological condition.14) To date, there has been no report of an effective therapy that can facilitate complete recovery from USN neurological deficiencies. Therefore, USN can result in permanent disability, and its management is an important factor in planning rehabilitation goals and functional outcome decisions.15)
Perceptive exploration is an impairment-oriented approach that facilitates the organization of actions by refining motor skills while using daily items and tools as therapeutic aids.16) Perceptual information required to perform a task refers to tactile motor sensory information that is used to adapt one’s body to the environment. This therapy has been introduced as a tool for patients with stroke and developmental disorders and has been proven to be safe and beneficial for such patients.16,17) However, there are no reports on the therapeutic application of perceptive exploration activities to USN patients. Perceptive exploration activities may provide clues to movement in the daily space and the handling of target objects affected by USN and may facilitate the functional recovery of actions. Therefore, this case study aimed to use perceptive exploration activities in the occupational therapy (OT) of patients with USN to explain the course of egocentric spatial neglect and allocentric neglect.
A 70-year-old man was diagnosed with cerebral infarction with the main symptoms of left hemiparesis and USN. Upon admission, magnetic resonance imaging (MRI) showed infarction in a narrow area of the watershed caused by occlusion of the right middle cerebral artery (MCA) (Fig. 1). Diffusion-weighted imaging showed right corona radiata infarction and right temporal white matter infarction. MRI using fluid-attenuated inversion recovery showed infarction in the internal border zone of the right MCA. In addition, arterial spin labeling showed decreased blood flow in a wide range of areas in the frontotemporoparietal region. The internal carotid artery was visualized by magnetic resonance angiography, and occlusion of the right distal MCA M1 was observed (Fig. 2).
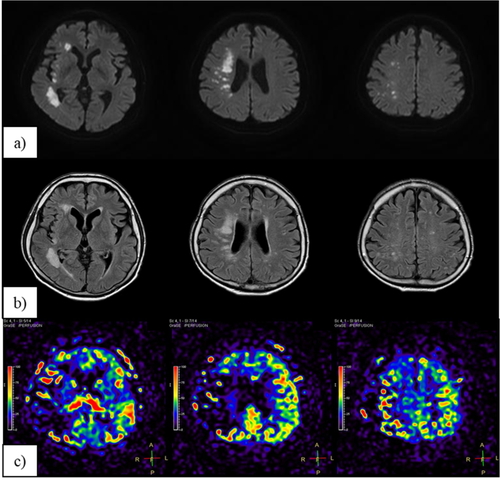
Head magnetic resonance imaging at onset. (a) Diffusion weighted images; (b) Fluid-attenuated inversion recovery; (c) Arterial spin labeling.

Head magnetic resonance angiography at onset. (a) Internal carotid artery stenosis is not observed; (b) Single occlusion of the right middle cerebral artery.
The patient developed left-side paralysis and was admitted to the acute neurosurgery ward. He was conservatively managed without any surgical intervention. OT and physiotherapy (PT) were initiated within 24 h after the onset of symptoms.
Neurological examination at admission showed left hemiparesis with the following Brunnstrom stages: left arm, IV (elements of selective movement close to V); fingers of left hand, V; left leg, VI. The posture was asymmetrically twisted to the left, whereas the line of sight and the head were directed to the right; all responses were biased to the right-side space. The motor function of the left arm was graded as mild paralysis based on a Fugl–Meyer Assessment (FMA) score of 55.18) Sensory impairment was observed in the superficial and deep sensations of the left arm and hand. Although the mobility of the left arm was good, the postural tone of the whole body increased during manipulation of an object with the left hand, and the manipulation was poor. Furthermore, face-to-face hand imitation overlooked the left side, and the movement by imitation was insufficient. In the manipulation of objects and tools by two-handed movements, the right hand was dominant and the subject had difficulty handling two or more objects at the same time. Regular use of the left hand was not observed. Cognitive function was assessed using the mini mental state examination (MMSE). The subject achieved a score of 24, with points lost in the areas of recall, language (naming), language (reading and writing), and drawing. The patient returned a frontal assessment battery (FAB) score of 8, with points deducted in the areas of sensitivity to interference and suppression control. Neuropsychological examination showed severe USN (Bisiach’s body neglect scale19) score of 3) and severe anosognosia (Bisiach’s anosognosia scale20) score of 3). The Behavioral Inattention Test (BIT) score was 44, with all BIT subitems well below the cutoff values indicating neglect. Left USN showed visual and tactile symptoms, and the subject was able to respond to the neglected space for auditory sensation. The patient had difficulty responding to the neglected space using memory as a cue because of interference stimulus. These neurological findings suggested right hemisphere syndrome and were consistent with MRI findings.
The patient needed assistance to perform ADL at admission because of neglect of the left body and left space and objects. Although the patient could walk, assistance was provided because his rapid movement presented a high risk of collision with stationary structures. The Functional Independence Measure (FIM) score was 76 (motor component, 45; cognitive component, 31). To evaluate the use of everyday items, we assessed the patient’s manipulation of tableware and a flip phone. At mealtime, the patient successfully used chopsticks with the right hand but could not hold tableware with the left hand. The patient had difficulty in using eating utensils in a coordinated manner with both hands. Tableware and food placed on the left side of the tray were overlooked. Although we considered placing a table on the right side of the patient, we found that spoken instruction was sufficient to prompt the patient to eat food that was otherwise overlooked. In manipulation of the flip phone, the buttons on the keypad were raised, and the contrast between the buttons and the background was clear; therefore, incoming calls and messages could be checked with the right hand. During manipulation, the flip phone could be held with the left hand on the paralyzed side. However, because the buttons on the keypad overlooked the part on the left side from the center, button manipulation was biased to the right side. It appeared that the patient could not see the screen while he stared at the buttons during manipulation and did not notice any mistakes in character input. Therefore, he found it difficult to make a phone call or compose an email. In addition, spoken instruction from others caused frustration and confusion, and it was difficult to input characters and to correct typographical errors.
The main problem was imposing posture contrary to the maintained asymmetry of twisting to the left while the active space was biased to the right. This was perceived as a reaction that seemed to promote the tendency of egocentric spatial neglect on the left side of the body. Adaptation to daily tasks was lost in the biased activity space because of allocentric neglect. Furthermore, spoken instruction for movement guidance acted as an interference stimulus that caused confusion. Spoken instruction did not provide clues for corrective actions and the patient could not grasp the relationship between the target object and the use of tools. Therefore, the OT policy was to support postural tone and control to maintain an asymmetrical posture and facilitate a coordinated relationship between postural control and activity tasks and handling of target objects. Given that spoken instruction for movement guidance caused confusion, target objects were also used to perform perceptive exploration activities by handling so that its manipulation was associated with the tactile motor sensation. The protocol for perceptive exploration activity was approved by the ethics committee of our hospital (Hashimoto Municipal Hospital) (approval number: 2019–01). Informed consent was obtained in writing from the patient and his family. PT focused on gait and exercises related to ADL. This program included passive range-of-motion exercises for the affected side and muscle strength exercises for the unaffected side. Therefore, PT focused on motor function. Regarding USN, the PT regimen focused on egocentric spatial neglect through the use of verbal instruction during gait training.
Providing Perceptive Exploration Activity by OTTherapies were performed with supervision and observation by an occupational therapist. OT sessions (40 min, 5 days per week) consisted of selective movements of the paralyzed limbs and trunk and facilitation of gait and balance responses to improve postural-motor control. The patient was treated for 30 days before transfer to a convalescent rehabilitation hospital. This treatment provided perceptive exploration activities as the main therapy following preparatory therapy. The program was then modified following improvements in motor function and USN of the paralyzed area. Table 1 outlines the functional changes of the patient and his perceptive exploration activities in clinical situations.
| Day of illness | Basic therapeutic activities | Expanded activities | Generalized function |
| Day 1 | Postural tone and facilitation of postural response | ||
| Facilitation of selective movement in the arms and hands | |||
| Power grip: grasp, holding | Beanbag | ||
| Intensive finger treatment: performance of fundamental movement | Stick manipulation | Independent oral care | |
| Facilitation of postural response | Writing | Can make a practical sign | |
| Improvement of gait | |||
| Day 21 | Tactile perception: poking, pushing | Origami, cards | Improved USN symptoms in the table space |
| Bilateral arm and hand activity | Scissors manipulation | Independent use of scissors | |
| Can make a call using a flip phone | |||
| Day 27 | Facilitation of hand stance and reaching | Wrapping a box with paper | Can simultaneously grasp two or more things |
| Independent use of a calculator | |||
| Tactile perception: pulling, scooping | Can repair the tablecloth | ||
| Day 28 | Applied gait | Moving around a corner | Independent gait and toileting |
| Bilateral arm and hand activity | Enter characters on a flip phone | Can send an email using a flip phone | |
| Day 29 | Bilateral arm and hand activity | Independent eating action | |
| Day 30 | Applied gait | Use of stairs | Can go out with a caregiver |
Day 21: Origami activity. Folding origami requires the hand motor skills of poking and manipulation. The change in resistance received by the fingers during origami is captured through tactile motor sensation. Handling was performed while focusing on the direction of movement of the fingers and checking the movement of the line of sight to follow the trajectory that creates the creases in the origami. This task was chosen because the visual changes of the target object occurred simultaneously with finger manipulation based on the tactile motor sensation. Occupational therapists used handling to explore changes in elasticity on the finger pad and the axial reaction force of the fingers, assisting in postural-motor control to facilitate finger stance and reach (Fig. 3a). After completing this task, the neglect on the left side improved in the desk space, and manipulation of the target object was possible with each hand.

Perceptive exploration activity. (a) Origami activity; (b) Wrapping a box with paper.
Day 27: Wrapping a box with paper. This task recognizes the entire box and requires a manipulation process that sees the object wrapped using processes in a specific order. One hand is required to handle the object as the main movement in two-handed movements. The other hand needs to have a function of mutual conversion between the left and right hands, such as auxiliary adjustment. In handling, the roles of stability and mobility of the left and right hands were clarified so that direct contact with the target object was not interrupted. To avoid inducing hastiness of movement, we emphasized the completion of one manipulation from the tactile motor sensation and then moved to the next manipulation (Fig. 3b). After completing this task, the patient succeeded in handling the target object with both hands, and the activity space biased to the right changed toward the midline.
Clinical Evaluation of Neurological and Physical FunctionSeveral clinical assessments were applied to investigate the effects of the protocol on the neurological and physical function of the patient (Table 2). The FMA score of arm function was determined at the start and finish of each OT session. The FMA score is an indicator of specific dysfunction in stroke and is commonly used to explain the recovery of motor function and the response of stroke patients to therapy.21) We assessed cognitive function using the MMSE and FAB. Effects on USN were assessed using Bisiach’s body neglect scale, Bisiach’s anosognosia scale, and the BIT. The FIM score was also measured before and after treatment to comprehensively assess physical performance, including ADL levels.
| Assessment | On admission: day 1 | Transferred: day 30 | |
| FMA | Arm motor function | 55/66 | 66/66 |
| Arm sensory function | 0/12 | 10/12 | |
| Superficial sensation | 0/4 | 4/4 | |
| Position sense | 0/8 | 6/8 | |
| MMSE | 24/30 | 27/30 | |
| FAB | 8 | 10 | |
| Bisiach’s body neglect scale | 3 | 0 | |
| Bisiach’s anosognosia scale | 3 | 0 | |
| BIT | Total score | 44/146 a | 131/146 |
| Subitems | Line erasure test | 18/36 a | 36/36 |
| Character erasure test | 12/40 a | 33/40 a | |
| Star mark erasure test | 13/54 a | 50/54 | |
| Copy design test | 0/4 a | 2/4 a | |
| Line bisector test | 0/9 a | 9/9 | |
| Graphic depiction test | 1/3 a | 1/3 a | |
| FIM | Total score | 76/126 | 120/126 |
| Motor subscale | 45/91 | 85/91 | |
| Cognitive subscale | 31/35 | 35/35 | |
a Result below the cutoff value indicating neglect.
The patient successfully completed the 30-day protocol of perceptive exploration activities. Throughout the program, the patient reported no adverse events and showed no deterioration in neurological or physical function.
After completion of the 30-day treatment protocol, all clinical assessments of neurological and physical function showed improvement. The increased motor function and sensory function of the left arm were reflected by the FMA score. At the conclusion of the 30-day treatment period, the MMSE score had increased by 3 points and the FAB score had increased by 2 points. Point deductions were attributed to the sensitivity of graphic depiction and interference stimuli and agreed with the results for the BIT subitems. Neglect and agnosia on the left side of the body showed maximum scores on Bisiach’s scale and showed improvement after treatment. However, although the BIT score increased after treatment, the results showed that the subitems of the BIT were affected by allocentric neglect by graphic depiction and interference stimuli. In terms of ADL, patient locomotion became independent, and self-care activities were achieved without support. On completion of the treatment, all served meals were eaten by the patient without assistance and food was not overlooked. In the manipulation of tableware, the left hand held the tableware, and the two-handed activity that cooperated with the chopstick manipulation of the right hand was successful. The patient was also able to use a flip phone to make phone calls and to compose and send emails without any indication or spoken instruction from others. However, when typing characters for the email, the patient took time to extract the intended characters when there was an interference stimulus, and it was challenging for the patient to correct missing characters and typographical errors during input.
In our proposed protocol, we hypothesized that the perceptive exploration activity could be safely completed and lead to functional recovery in a patient with stroke-related USN. To the best of our knowledge, there are no reports on the use of perceptive exploration activity by USN patients after a stroke, and there is only one report on perceptive exploration activity in patients with motor dysfunction of the arms.16) The present study has demonstrated progress over the course of the therapy along with the immediate effects of the perceptive exploration activity. Therefore, the course of therapy that employs perceptive exploration activity in this report has never been reported before and can be regaarded as a hypothesis of therapy that leads to functional recovery of stroke patient.
At the initiation of therapy, the patient exhibited personal space neglect in which the paralyzed left arm did not participate in the activity space. Egocentric spatial neglect and allocentric neglect were observed in the peripersonal space. Ignoring personal space on the left side of the body often occurs in the presence of right hemisphere lesions, and lesions at the right temporo-parietal junction have been pointed out.22) Neglect of the peripersonal space is also known to be related to the network of the right frontal lobe and superior temporal gyrus,23) which is consistent with the patient’s MRI findings. The patient’s egocentric spatial neglect and allocentric neglect caused a bias in the active space and affected the perception of objects. When handling a target item, the patient was observed to use great care and attention. Therefore, it was inferred that despite the good mobility of the paralyzed hand, it was difficult for the patient to explore changes in the resistance received from the object. In use of the flip phone, the patient had difficulty seeing the screen and buttons simultaneously when using the keypad. The identification of characters and typographical errors was also challenging. It has been reported that the difficulty of seeing two or more objects or parts at the same time may indicate a decrease in the visuospatial image and visual working memory.24) Therefore, we inferred that these mechanisms affect the exploration process of visual and tactile motor sensations and limit the recognition of space and objects.
In the origami folding task, we observed that the line of sight coordinating with hand movement was based on the tactile motor sensation received at the fingertips. König et al.25) suggested that the input of self-motion and the accompanying sensory signals develop knowledge about new sensory movements after exercise and cause changes in perception. Therefore, it is possible that the processes that controlled the switching of hand movement direction based on the tactile motor sensation also facilitated the movement of the line of sight as a reaction to the movement of the whole body. The bias of the activity space was reduced in the box-wrapping task, and the handling of multiple target objects with both hands simultaneously was improved. However, before the task was completed, the manipulation of the target object did not spread from one part of the activity space to the whole space; rather, it tended to be biased to one part of the space. This is one of the symptoms of neglect in the somatosensory system and the visual modality and indicates that the hand cannot perform exploratory manipulations.26) Therefore, during therapy, we guided the relationship and order of the activity space and the target object by tactile motor sensation while clarifying the roles of the left and right hands. Polanowska et al.27) suggested that the provision of perceptual information combined with sensory modalities other than vision improves neglect symptoms. We consider that each therapy session was able to improve neglect symptoms by focusing on the relationship between the target object and self-manipulation in the active space based on tactile motor sensation.
Despite improvements in handling, we noticed that operation of the flip phone remained susceptible to interference stimuli. Although the patient noticed typographical errors in character input, he had difficulty in correcting them. It has been reported that the manipulation of electronic devices, such as flip phones, is affected by visuospatial function.28) However, in this patient, the FAB results showed that there was little improvement in sensitivity to interference stimuli and suppression control. Therefore, future studies on this topic must analyze electronic device manipulation in relation to frontal lobe function and visuospatial function.
Clinical evaluation of our patient after the 30-day course of therapy showed improvements in neurological and physical function. However, the underlying mechanism of functional recovery by perceptive exploration activity remains to be elucidated. USN has been found to be associated with the multisensory cortex,29) which is located in the superior temporal cortex, insula, and the temporo-parietal junction of the minor hemisphere. The role of the multisensory cortex is thought to be to converge vestibular sensation, auditory, cervical proprioceptive, and visual inputs, create higher-order spatial representations of the body’s position in the environment, and adapt the body to space. This suggests that perceptual information from different sensory modalities is effective in improving neglect symptoms. Therefore, we applied a perceptive exploration activity that mediates task performance based on tactile motor sensation to a USN patient. The results of this case study demonstrated the feasibility of a protocol for perceptive exploration activity based on tactile motor sensation. However, the content and frequency of perceptive exploration activities used in the therapy protocol for USN patients should be further refined in future studies.
This case study had several limitations. First, the effectiveness of the proposed therapy protocol in a patient with USN should be confirmed in a single case study or in a crossover study with multiple patients in a randomized controlled trial. Second, the optimal content of the perceptive exploration activity should be determined based on the severity of USN. Early introduction of the protocol may have resulted in further improvements in motor function of the paralyzed arm. Third, this study did not use high-technology neurophysiological studies, such as single-photon emission computed tomography, to investigate the relationship between USN and behavior. The patient may have shown good improvement in USN because the infarct lesion remained in a narrow watershed with collateral circulation despite the wide area of hypoperfusion. Therefore, future studies should examine the relationship between neurophysiological change and functional recovery caused by perceptive exploration activity based on tactile motor sensation.
This case study demonstrated the use of OT with perceptive exploration activities in a patient with USN. The proposed therapy protocol features the application of perceptive exploration activities based on tactile motor sensation. This treatment may emerge as a new neurorehabilitation therapy for patients showing USN after stroke. However, the suitability of this protocol needs to be confirmed using a larger sample size.
We thank the patient for his participation in this study.
The authors report no conflicts of interest.