2022 年 7 巻 論文ID: 20220022
2022 年 7 巻 論文ID: 20220022
Background: Advances in cancer treatment have led to an increase in the number of cancer survivors and, likewise, cancer patients in convalescent rehabilitation wards. It is difficult for patients with bone metastases to recover their motor functions and be discharged. However, cancer treatments, such as anti-cancer drug therapy and radiation therapy, are not generally provided in convalescent rehabilitation wards.
Cases: This study retrospectively reviewed six cases of bone metastases in our convalescent rehabilitation ward from April 2018 to October 2019. The ages of the patients ranged from 58 to 85 years, and all patients were male. The primary cancers were lung cancer (two cases), renal cancer (one case), esophageal cancer (one case), prostate cancer (one case), and double lung and kidney cancer (one case). Bone metastases were observed in the spine (six cases), pelvis (two cases), and femur (one case). All patients were admitted to our convalescent rehabilitation ward for postoperative management of imminent fracture risk and rehabilitation of pathological fracture or spinal cord compression caused by bone metastasis. None of the patients received treatment for primary cancer or bone metastases during their hospitalization. Two patients had new bone metastases in load-bearing bones. Five patients were transferred to acute care hospitals for the treatment of cancer or infection.
Discussion: Before transferring patients with bone metastases to convalescent rehabilitation wards, clinicians should assess the risk of skeletal-related events and the rate of progression of their cancer. Indications for hospitalization should be carefully determined in cooperation with acute care hospitals.
Recent advances in cancer treatment have led to increased survival rates, highlighting the importance of rehabilitation for cancer patients. In Japan, rehabilitation is recommended for cancer patients regardless of cancer type.1) As a result, the number of cancer patients admitted to convalescent rehabilitation wards is also increasing.
For patients with bone metastases, disabling factors such as load limitation or pain make it difficult to recover sufficient motor function for discharge. However, under the Japanese medical insurance system, anti-cancer treatments, such as drug therapy and radiation therapy, cannot be provided in convalescent rehabilitation wards in general because the drug fee is included in the hospitalization fee. At the time of writing, there are no other reports regarding rehabilitation of patients with bone metastases in convalescent rehabilitation wards.
We retrospectively reviewed the cases of six patients with bone metastases who were admitted to our hospital from April 2018 to October 2019. A summary of these cases is presented in Table 1. All patients were admitted to the convalescent rehabilitation ward for postoperative management of imminent fracture risk and rehabilitation of pathological fracture or spinal cord compression caused by bone metastases. None of the patients received treatment for primary cancer or bone metastases throughout admission. Prior to admission, three patients (cases 3, 4, and 6) had factors inhibiting rehabilitation such as load limitation, pain, and general fatigue. Active rehabilitation to regain walking ability could not be performed in two cases (cases 2 and 3) because of the diagnosis of new bone metastases in load-bearing bones during hospitalization. Five patients (cases 2–6) required transfer to acute care hospitals for the treatment of cancer or infection. All patients temporarily improved their activities of daily living (ADL) during hospitalization, but it eventually decreased for some patients (cases 5 and 6) because of deterioration in their general condition (Fig. 1, Table 2). This retrospective study was performed at the Nishi Memorial Port Island Rehabilitation Hospital, Kobe, Japan. This study was approved by the Institutional Review Board (IRB) of the hospital (approval number 18). Informed consent was obtained using the opt-out method.
| Case | 1 | 2 | 3 | 4 | 5 | 6 |
| Age (years)/sex | 85/male | 75/male | 58/male | 85/male | 62/male | 66/male |
| Primary cancer | Renal cancer | Renal cancer Lung cancer | Lung cancer | Lung cancer | Prostate cancer | Esophageal cancer |
| Bone metastases | Left femoral neck Vertebra | Vertebrae Right acetabulum d | Vertebrae Pelvis Right tibia d | Vertebrae Pelvis | Vertebrae | Vertebrae |
| Treatment for primary cancer a | Nephrectomy Pazopanib (discontinued) | Nephrectomy | Chemotherapy | None | Bilateral orchiectomy | Chemotherapy |
| Treatment for bone metastases a | Left artificial femoral head replacement | Radiotherapy (vertebrae) Thoracolumbar laminectomy and fusion surgery | Radiotherapy (vertebrae) Bone tumor embolization Thoracic laminectomy and fusion surgery | Osteosynthesis | Bilateral orchiectomy | Radiotherapy (vertebrae) Denosumab (once) Thoracic laminectomy and fusion surgery |
| Katagiri score b | 7 | 7 | 9 | 7 | 3 | 7 |
| Mirels’ score c | 11 | ND | 9 | 8 | ND | ND |
| SINS c | 5 | 14 | 9 | 13 | 3 | 12 |
| Days of hospitalization | 90 | 70 | 29 | 72 | 71 | 16 |
| Outcome | Returned home | Hospital transfer | Hospital transfer | Hospital transfer | Hospital transfer | Hospital transfer |
a Before admission to rehabilitation ward. b On admission to rehabilitation ward. c Mirels score and SINS of operated region were evaluated preoperatively, and those of non-operated region were evaluated on admission. d New bone metastases found after admission to our hospital.
ND, not determined.
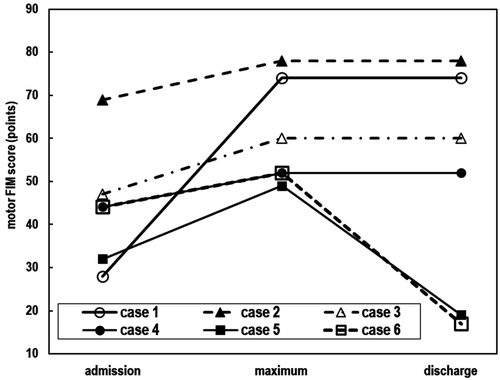
Changes in motor FIM score during hospitalization.
| Case | 1 | 2 | 3 | 4 | 5 | 6 | ||||||||||||
| Adm | Max | Dis | Adm | Max | Dis | Adm | Max | Dis | Adm | Max | Dis | Adm | Max | Dis | Adm | Max | Dis | |
| Self-care | ||||||||||||||||||
| Eating | 6 | 7 | 7 | 7 | 7 | 7 | 5 | 5 | 5 | 5 | 7 | 7 | 5 | 7 | 1 | 5 | 5 | 1 |
| Grooming | 4 | 7 | 7 | 7 | 7 | 7 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 7 | 3 | 5 | 5 | 1 |
| Bathing | 1 | 5 | 5 | 1 | 7 | 7 | 1 | 3 | 3 | 1 | 3 | 3 | 1 | 4 | 2 | 1 | 3 | 1 |
| Dressing upper body | 4 | 7 | 7 | 7 | 7 | 7 | 1 | 7 | 7 | 4 | 4 | 4 | 5 | 5 | 2 | 5 | 5 | 1 |
| Dressing lower body | 1 | 6 | 6 | 6 | 6 | 6 | 1 | 6 | 6 | 3 | 4 | 4 | 5 | 5 | 1 | 5 | 5 | 1 |
| Toileting | 1 | 6 | 6 | 6 | 6 | 6 | 6 | 6 | 6 | 4 | 5 | 5 | 4 | 4 | 1 | 5 | 5 | 1 |
| Sphincter control | ||||||||||||||||||
| Bladder management | 1 | 4 | 4 | 7 | 7 | 7 | 7 | 7 | 7 | 5 | 5 | 5 | 1 | 5 | 2 | 4 | 5 | 4 |
| Bowel management | 1 | 6 | 6 | 6 | 6 | 6 | 6 | 6 | 6 | 6 | 6 | 6 | 1 | 4 | 2 | 2 | 6 | 2 |
| Transfers | ||||||||||||||||||
| Bed/chair/wheelchair | 3 | 6 | 6 | 7 | 6 | 6 | 6 | 6 | 6 | 4 | 5 | 5 | 1 | 4 | 1 | 4 | 5 | 1 |
| Toilet | 3 | 6 | 6 | 7 | 6 | 6 | 6 | 6 | 6 | 4 | 5 | 5 | 1 | 1 | 1 | 5 | 5 | 1 |
| Bath/shower | 1 | 4 | 4 | 1 | 6 | 6 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Locomotion | ||||||||||||||||||
| Walking/wheelchair | 1 | 6 | 6 | 6 | 6 | 6 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Stairs | 1 | 4 | 4 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Total | 28 | 74 | 74 | 69 | 78 | 78 | 47 | 60 | 60 | 44 | 52 | 52 | 32 | 49 | 19 | 44 | 52 | 17 |
Adm, score on admission; Max, maximum score; Dis, score on discharge.
An 85-year-old man was diagnosed with right renal cancer, lung metastasis, and multiple bone metastases in the left femoral neck and the 11th thoracic vertebra 4 months prior to admission to our hospital. He underwent right nephrectomy 2 months prior to admission. Adjuvant pazopanib therapy was started 2 weeks after nephrectomy but was stopped because of left femur surgery. One month prior to admission, he underwent left artificial femoral head replacement for an imminent fracture. The patient was transferred to our hospital for postoperative rehabilitation.
As rehabilitation progressed, the patient’s leg strength and performance in ADL gradually improved. Although the metastasis in the 11th thoracic vertebra increased during hospitalization (Fig. 2), he had no pain or paralysis. On day 90, the patient was discharged home under the care of his family and a nursing care service. On discharge, he was able to walk with slight assistance or supervision. His motor functional independence measure (FIM) score increased from 28 points at admission to 74 points at discharge because of improvement in function and environmental settings (Table 2).
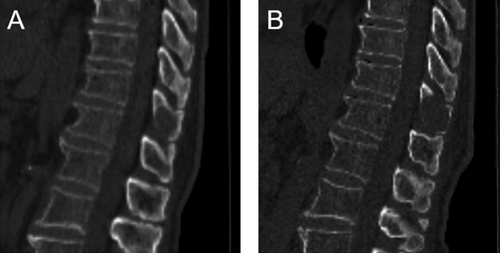
CT of case 1. (A) On admission. (B) On day 63. The osteolytic metastasis in the spinous process of the 11th thoracic vertebra became larger.
A 75-year-old man with a medical history of postoperative renal cancer had low back pain and was diagnosed with lung cancer and 11th and 12th thoracic vertebral metastases 2 months prior to admission to our hospital. The patient was treated with radiotherapy for bone metastases. However, he developed paralysis of the left leg because of a compression fracture in the 11th thoracic vertebra and malignant spinal cord compression (MSCC), leading to thoracolumbar laminectomy and fusion surgery 1 month prior to admission (Fig. 3A,B). The patient was transferred to our hospital for postoperative rehabilitation.
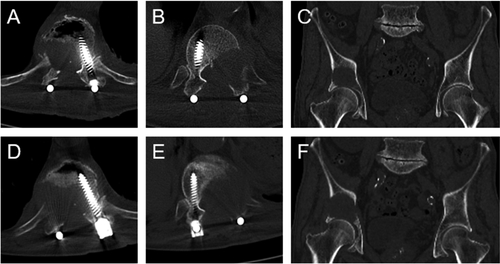
CT of case 2. (A) CT of 11th thoracic vertebra (Th11) on admission. (B) CT of 12th thoracic vertebra (Th12) on admission. (C) CT of pelvis on day 38. (D) CT of Th11 on day 58. (E) CT of Th12 on day 58. (F) CT of pelvis on day 58. CT on day 58 showed that the bone metastases on the right acetabulum and vertebrae had increased in size.
On admission to our hospital, the paralysis in the patient’s left leg improved, and he was able to walk with a cane. As rehabilitation progressed, he was able to walk independently. However, on day 20, he experienced back pain and numbness and pain in his right thigh. On day 38, a new bone metastasis in the right acetabulum was detected by computed tomography (CT) (Fig. 3C). Considering that it was difficult to unload the area with braces, we ordered the patient to use a wheelchair to avoid pathological fractures. On day 57, during follow-up for the primary cancer at the acute care hospital, he was diagnosed with hypercalcemia. Therefore, we took the unusual step of treating the patient with zoledronic acid in our hospital. A CT scan on day 58 showed that the bone metastases on the right acetabulum and vertebrae had increased (Fig. 3D,E,F). On day 70, we decided that it was difficult for the patient to continue rehabilitation and transferred him to the acute care hospital for treatment for the cancer. His motor FIM score had increased from 69 points on admission to 78 points at discharge because of appropriate movement instruction and environmental settings (Table 2).
Case 3A 58-year-old man was diagnosed with sixth and eighth thoracic vertebral metastases during chemotherapy for lung cancer, and radiotherapy was initiated for metastases 3 months prior to admission to our hospital. However, the following month, the patient suffered a fall at home, and he was admitted to the acute care hospital. During this time, he had paralysis and decreased sensation in both legs and was diagnosed with MSCC. He underwent semi-emergent bone tumor embolization, thoracic laminectomy, and fusion surgery. Later, a new bone metastasis was found in the right iliac bone (Fig. 4A), but it was followed up. The patient was transferred to our hospital for postoperative rehabilitation.
CT of case 3. (A) CT of pelvis on admission. (B) CT of right tibia on day 22 (sagittal CT). (C) CT of pelvis on day 22. A new tumor was found in the tibia, and the pelvic tumor had become larger.
On day 3, the patient experienced right hip pain during exercise. Despite the application of transdermal narcotics, he experienced increased pain in his back and left anterior chest because of bone metastases and extensive left pleural dissemination. The pain prevented him from undergoing active rehabilitation. On day 19, the patient developed new pain in his right lower leg. A CT scan on day 22 showed a new bone metastasis in his right tibia (Fig. 4B) and growth of other bone metastases (Fig. 4C). On day 29, the patient was transferred to an acute care hospital for radiation therapy for right tibial metastasis. His motor FIM score had increased from 47 points on admission to 60 points at discharge because of appropriate movement instruction and environmental settings (Table 2).
Case 4An 85-year-old man fractured his left femoral neck in a fall 2 months prior to admission to our hospital. Lung cancer and multiple bone metastases were detected preoperatively. However, the patient and his family declined further intensive examination and treatment for cancer. He underwent osteosynthesis 1 month prior to admission and was transferred to our hospital for postoperative rehabilitation.
CT at admission showed multiple osteolytic bone metastases in the acetabulum and whole vertebrae, including the second and third cervical vertebrae (Fig. 5). However, we could not provide active rehabilitation because the patient refused to wear a lumbar corset or a cervical collar. In addition, he gradually became fatigued and experienced pain in his left shoulder. We had no choice but to provide rehabilitation on the bed. On day 70, he developed gross hematuria because of disseminated intravascular coagulation, which required his transfer to an acute care hospital 2 days later. His motor FIM score had increased from 44 points on admission to 52 points at discharge because of appropriate movement instruction and environmental settings (Table 2).

CT on admission of case 4. Multiple osteolytic bone metastases can be observed.
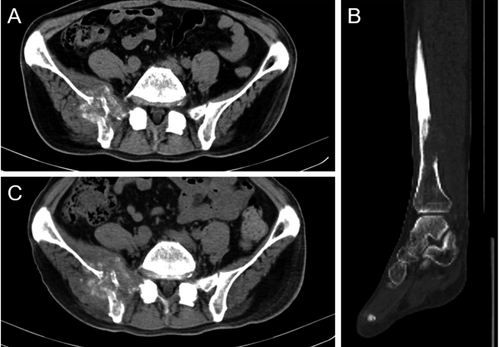
A 62-year-old man developed muscle weakness and numbness in both legs 1 month prior to admission to our hospital. A week later, he was unable to stand. This led to his admission to an acute care hospital, where he was diagnosed with prostate cancer with metastases in the sixth, eighth, and ninth thoracic vertebrae (Fig. 6) and the third and fifth lumbar vertebrae, MSCC with bladder and rectal disturbance, and paralysis in both legs. He underwent bilateral orchiectomy 2 weeks prior to admission to our hospital. A lumbar corset was created, and bone metastases were followed up. The patient was transferred to our hospital for postoperative rehabilitation.

Pre-operative magnetic resonance imaging of case 5. Bone metastases and spinal cord compression in the sixth, eighth, and ninth thoracic vertebrae are visible. (A) T1-weighted image. (B) T2-weighted image.
As rehabilitation progressed, strength in the patient’s leg muscles increased, and he was able to walk with a walker and bilateral long leg braces. His bladder and rectal disturbances also recovered, and he was able to urinate. Although his rehabilitation progressed well, he developed cholecystitis on day 67. In addition, his serum levels of inflammatory markers remained significantly elevated despite the use of antibacterial drugs. On day 71, we decided to transfer the patient to the acute care hospital for cholecystectomy. His motor FIM score had temporarily improved from 32 points on admission to 49 points because of improvement in function, appropriate movement instruction, and environmental settings, but his score had decreased to 19 points at discharge (Table 2).
Case 6A 66-year-old man was diagnosed with advanced esophageal cancer and underwent palliative chemoradiotherapy for esophageal stenosis 7 months prior to admission to our hospital. He was admitted to an acute care hospital for chemotherapy 1 month prior to admission and thoracic vertebral metastases were detected (Fig. 7A). Because of severe pain from the metastases, treatment with radiation therapy and denosumab was given priority. However, 2 weeks prior to admission, he developed numbness in both legs because of MSCC and underwent emergency thoracic laminectomy and fusion surgery (Fig. 7B). The patient was transferred to our hospital for postoperative rehabilitation.
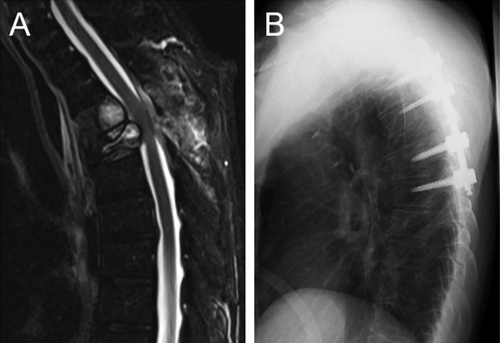
(A) Pre-operative magnetic resonance imaging of case 6. T2-weighted image shows bone metastases and spinal cord compression in the 11th and 12th thoracic vertebrae. (B) X-Ray of case 6 after thoracic laminectomy and fusion surgery.
Because the patient experienced severe back pain and general fatigue from the time of admission, we could not provide active rehabilitation. On day 15, the patient developed fever and chills with abnormally high serum levels of inflammatory markers. He was transferred to an acute care hospital the following day to treat the infection. His motor FIM score had temporarily improved from 44 points on admission to 52 points because of appropriate movement instruction and environmental settings, but his score had decreased to 17 points at discharge (Table 2).
This study revealed two major problems regarding convalescent rehabilitation for patients with bone metastases. In five of the six cases described here, rehabilitation was discontinued because of cancer progression or complications associated with cancer that led to transfer of the patient to an acute care hospital.
The patients in cases 2 and 3 were transferred to an acute care hospital for treatment of cancer. As explained previously, under the Japanese medical insurance system, cancer treatment cannot be provided during hospitalization in convalescent rehabilitation wards. Given that the length of hospitalization in a convalescent rehabilitation ward is often several months, patients should be admitted only when their cancers are expected to be under control without cancer treatment for several months after discharge from acute care hospitals. The patients in cases 4, 5, and 6 were transferred to acute care hospitals for treatment of complications. In cases of progressive cancer, complications caused by immunocompromise and coagulation disorders are likely to occur. Katagiri,2) Tomita,3) and Tokuhashi4) scores can be used to predict the life prognosis of patients with bone metastases. In this study, Katagiri scores demonstrated short-term prognoses for all cases except case 5 (Table 1). Patients with a poor prognosis or rapidly progressing cancer should not be admitted to a convalescent rehabilitation ward. If cancer is not controlled, disabling factors are more likely to occur, such as growth of bone metastases (cases 2 and 3) and complications associated with the cancer (cases 4, 5, and 6). Although there are some reports on the rehabilitation of patients with bone metastases and their improvements in motor function, ADL, and quality of life,5,6,7) these reports are about rehabilitation of patients during cancer treatment. There are no reports on the efficacy of rehabilitation in patients with bone metastases without cancer treatment.
The patients in cases 2, 3, and 4 were considered to be at risk of pathological fracture after hospitalization, which prevented us from providing active rehabilitation. Skeletal-related events (SREs), especially pathological fractures, are important in the rehabilitation of patients with bone metastases. During the acute care hospital stay, a whole-body scan should be performed to detect bone metastases and assess the risk of SREs. Otherwise, new bone metastases may be detected after transfer to a convalescent rehabilitation ward, making rehabilitation difficult. In addition, routine follow-up imaging is necessary to check for bone metastases growth while the patient is in the convalescent rehabilitation ward, and the risk of long bone pathological fractures or spinal instability can be assessed through scoring systems such as Mirels’ score8) or the Spinal Instability Neoplastic Score (SINS).9) The risk of SREs increases with a high number of bone metastases, high pain score, poor ECOG performance status (3–4), and prior history of SREs.10,11,12) However, rehabilitation with proper risk assessment does not increase the risk of pathological fractures.13) Therefore, rehabilitation should be offered to patients with bone metastases. To maintain ADL status as much as possible, even in patients with unstable bone metastases, clinicians must provide appropriate movement instruction, consider the use of orthoses, and consult with orthopedic surgeons regarding surgical indications.
In the current study, although five patients were forced to transfer to acute care hospitals, we temporarily improved their ADL status during hospitalization. For patients with bone metastases, ADL status should be improved according to their functional prognosis through strategies based on improving function, appropriate movement instruction, use of compensatory measures, and environmental settings. Poor rehabilitation outcomes of patients with bone metastases have been associated with hypercalcemia and administration of parenteral narcotics.14) Conversely, a good prognosis in MSCC patients is associated with good ambulatory status before treatment, no visceral metastasis, and slow progression of neurologic impairment after 14 days.15,16) For MSCC patients with a poor functional or life prognosis, the importance of short-term rehabilitation, with goals expected to be achieved within a month (e.g., managing transfers, reducing pain, and achieving urinary continence), has been emphasized.17) Although these reports are also about rehabilitation during cancer treatment, they could help in predicting functional prognosis and developing rehabilitation programs in convalescent rehabilitation wards. In case 1 in the present study, despite the patient showing bone metastasis growth, there was no pain or paralysis, which enabled the patient to return home. In contrast, the other patients were forced to transfer to acute care hospitals and had symptoms such as severe pain and fatigue that were suggestive of cancer progression at the time of admission or shortly afterward. This also inhibited active rehabilitation in these cases. The results of the current study suggest that when there is bone metastases growth in load-bearing bones (cases 2 and 3) or a complication associated with cancer (cases 4, 5, and 6), it may be difficult to improve motor function with convalescent rehabilitation.
We consider that intensive rehabilitation in a convalescent rehabilitation ward can improve ADL status in patients with bone metastases if they receive proper assessment of the risk of SREs and cancer status. However, if patients are admitted to convalescent rehabilitation wards without cancer control, they miss the opportunity to treat their cancer. This may result in a deterioration of their general condition because of cancer progression or complications associated with cancer.
In conclusion, for patients with bone metastases, the risk of SREs and the speed of cancer progression should be assessed before admission to convalescent rehabilitation wards. Indications for hospitalization should be carefully determined in cooperation with acute care hospitals.
The authors thank Kosuke Miyamoto, MD, Yoko (Haraguchi) Kenmotsu, MD, and Masaru Kobayashi, MD, for providing their assistance with data collection. They were affiliated with the Nishi Memorial Port Island Rehabilitation Hospital.
The authors report no conflicts of interest.