2022 年 7 巻 論文ID: 20220063
2022 年 7 巻 論文ID: 20220063
Objectives: Hip fracture in the elderly involves two cases of invasive damage to the body within a short period of time: the fracture itself and subsequent surgery. This situation affects physical strength and presents a major challenge during convalescent rehabilitation. This study aimed to evaluate the effects of hochuekkito, a traditional Japanese herbal medicine, on physical activity, appetite, motivation, and quality of life (QOL) during inpatient rehabilitation treatment after hip surgery.
Methods: Thirty-eight patients with hip fracture who underwent postoperative convalescent rehabilitation were randomly assigned to either the hochuekkito group (n=20, daily hochuekkito administration from day 3 after surgery until discharge from hospital) or the control group (n=18). Physical activity was measured with a small tri-axial accelerometer worn by the patients; appetite was evaluated based on daily dietary calorie consumption; motivation was measured using the vitality index score; and QOL was measured using the European QOL 5-Dimensions 5-Levels questionnaire and its associated EQ-visual analog scale (EQ-VAS). All patients were assessed at day 3 (baseline) and 2, 4, 6, 8, and 10 weeks after surgery and at the time of discharge from hospital.
Results: The results for the hochuekkito group were significantly higher than the control group for walking exercise at 10 weeks, vigorous activity time at 8 weeks, dietary calorie consumption at 10 weeks and at discharge, and EQ-VAS score at 6 weeks.
Conclusions: In elderly hip fracture patients, a course of hochuekkito administration starting soon after surgery significantly improved QOL, physical activity, and appetite at 6 weeks after surgery.
The Japanese population has the highest proportion of elderly people worldwide. As of October 2020, the proportion of Japanese residents aged 65 years and over had reached 28.8%.1) In addition, elderly women account for an increasingly large proportion of the population, with 17.6% of the total population being women aged 75 years or older.1) This aging of the population has resulted in an increased incidence of hip fracture. In 2012, there were around 175,700 cases of hip fracture in Japan,2) whereas in 2020, the number of novel cases was estimated to be 240,000; this number is projected to rise to 290,000 by 2030 and 320,000 by 2040.3) A fall from a standing height is the cause of injury in approximately 80% of the cases, and hip fracture is one of the most important types of fragility fracture. The most common age group for hip fractures in Japanese women is 85–89 years,4) and most of them not only undergo surgery, such as osteosynthesis or hemiarthroplasty, but also require rehabilitation treatment to restore their physical activity. The Japanese government has introduced a system of public social medical care, and, in almost all cases, rehabilitation treatment after hip fracture surgery is conducted while patients are hospitalized. Because these elderly patients have experienced hip fracture followed by highly invasive surgery within a short time, there are many barriers to rehabilitation treatment to promote their postoperative recovery. A large number of elderly patients who suffer hip fracture already have multiple comorbidities prior to the hip fracture. For these patients, their general condition, gait function, ability to perform activities of daily living (ADL), and physical strength are often affected by decreased muscle strength in the form of frailty or sarcopenia, pain and joint contractures caused by bone and joint deformities, poor balance, cognitive impairment, malnutrition, and other disorders. This means that such patients with hip fracture tend to require a prolonged period of hospitalization while undergoing rehabilitation treatment to promote their postoperative recovery.
Hochuekkito (HET), a traditional Japanese herbal (Kampo) medicine, is indicated for patients with weakened digestive function, severe fatigability of the limbs, and a delicate constitution. In clinical use, it is effective for the treatment of conditions including wasting diseases, reinforcement of physical strength after illness, and improving anorexia, fatigue, and malaise. However, the effectiveness of HET is unclear in the treatment of elderly patients who suffer hip fracture and highly invasive surgery within a short time and then undergo rehabilitation treatment while their appetite and physical activity levels are diminished. If HET could improve appetite and physical activity levels during convalescent rehabilitation after hip fracture, patients may experience improved ADL and shorter hospital stays. The aim of this study was to explore the efficacy and safety of HET for patients with hip fracture undergoing postoperative convalescent rehabilitation treatment.
The study drug was “Tsumura hochuekkito extract granules for ethical use (TJ-41)”, manufactured by Tsumura & Co. (Tokyo, Japan). The dosing regimen was 7.5 g per day divided into three doses (2.5 g per dose, one sachet containing 2.5 g) taken orally before meals. HET is a spray-dried hot-water oil extract of a mixture of the following ten crude drugs: Astragalus root (16.7%), Atractylodes lancea rhizome (16.7%), Ginseng (16.7%), Japanese angelica root (12.5%), Bupleurum root (8.3%), Jujube (8.3%), Citrus unshiu peel (8.3%), Glycyrrhiza (6.3%), Cimicifuga rhizome (4.2%), and Ginger (2.0%).
Study DesignThis randomized controlled trial was conducted between May 2017 and March 2020 at Konan Hospital (Kumamoto, Japan). After hip surgery, patients were randomly divided into HET and control groups using the central registration method.
This study was approved by the Konan Hospital Institutional Review Board (No. 20170303K075) and the Kumamoto University Certified Review Board (No. CRB7180006). Written informed consent was obtained from the study subjects or their legal guardians. This study was registered in the University Hospital Medical Information Network Clinical Trials Registry (http://www.umin.ac.jp/ctr/; No. UMIN000027244) and the Japan Registry of Clinical Trials (https://jrct.niph.go.jp/; No. jRCTs071180027). This study was conducted in compliance with the Declaration of Helsinki.
PatientsAll patients who underwent hip fracture surgery (osteosynthesis or hemiarthroplasty) during the study period were invited to join the study if they met the following inclusion criteria: i) they would receive inpatient convalescent rehabilitation treatment in the same hospital without transferring to another hospital after surgery; ii) they were at least able to mobilize indoors independently before the fracture with or without walking aids; iii) they had Mini-Mental State Examination (MMSE)5) score of 10 points or higher; iv) they were aged 65 years or over; v) they were able to take the study drug by mouth. Patients were excluded if: i) they had serious comorbidity (including liver, kidney, heart, hematologic, autoimmune, and/or metabolic diseases); ii) they had malignancy or rheumatoid arthritis; iii) they were on hemodialysis; iv) they were going to have low-intensity pulsed ultrasound (LIPUS) or other adjuvant therapy to promote synostosis after surgery; v) they were taking any Kampo medicine during the study period; vi) they had previous allergy or adverse drug reaction to a Kampo medicine; vii) they used the study drug (HET) within 2 weeks prior to commencement of the study; or viii) they were considered unsuitable by a treating doctor for any other reason.
In all, 135 patients were assessed for eligibility after hip surgery. Of these, 39 patients were included into the study and randomized; 20 to the HET group and 19 to the control group. The study flowchart is presented in Fig. 1. One patient in the control group withdrew between randomization and baseline assessment (at postoperative day 3). The remaining 38 patients (20 in the HET group, 18 in the control group) completed the study.

Flowchart of hip fracture patients selected for this study.
Patients in the HET group received HET three times a day from postoperative day 3 until the day of discharge from the hospital. Patients in the control group did not have HET. Both HET and control groups underwent inpatient convalescent rehabilitation treatment. The allocation ratio was 1:1. The preparation of the allocation table and the operation of the central registration center were outsourced to IROM CS (Fukuoka, Japan). Both groups continued daily rehabilitation treatment involving muscle strengthening training, joint range-of-motion exercise, and weight-bearing from day 1 after the surgery until discharge.
Prohibited Concomitant DrugsThe concomitant use of Kampo medicines other than the study drugs was prohibited throughout the study period. In addition, osteoporosis treatment drugs, antipsychotics, antidepressants, mood stabilizers, anxiolytics, sleeping pills, and gastrointestinal prokinetic agents were not changed in dosage or newly used throughout the study period.
Outcome MeasurementsWe assessed physical activity level, appetite, motivation, ADL, quality of life (QOL), weight, pre-albumin level, number of days to achieve graded levels of walking ability, and postoperative length of hospital stay. Physical activity level was measured using a small tri-axial accelerometer (Active style Pro HJA-750C; Omron Healthcare, Kyoto, Japan). This accelerometer (40 × 52 × 12 mm, approximately 23 g including battery) was worn at all times from getting up to going to sleep, except during showering or bathing. The physical activity level was the amount of exercise (Ex) calculated by multiplying the metabolic equivalents (METs) by time. Ex (METs × minutes) is a unit that reflects the amount of exercise in terms of its intensity and duration. In this study, we compared activity levels during daily activities and walking, as well as the amount of time engaged in sedentary activity (<3.0 METs), moderate activity (3.0–5.9 METs), and vigorous activity (≥6.0 METs). The physical activity level at each assessment was recorded as the daily average of measurements over the previous 7 days. Appetite was assessed in terms of the daily dietary calorie consumption calculated from the amount of food left uneaten after meals. Baseline values were taken as the mean values measured on postoperative days 1 and 2, and the value at each time point was taken as the daily average of measurements over the previous 7 days. Motivation was assessed by the vitality index score,6) ADL by the Functional Independence Measure (FIM) score,7) QOL by the European QOL 5-Dimensions 5-Levels questionnaire (EQ-5D-5l)8) and its associated EQ-visual analog scale (EQ-VAS) score, and nutritional status by pre-albumin value. Gait function was assessed by the number of days required to reach each of the following graded goals for walking ability: walking within parallel bars, walking with a walker, walking with a cane, and pre-fracture walking ability. The examiner was not involved in the division of study groups and was not informed on which group the patients were assigned.
Observations were conducted from postoperative day 3 until the day of discharge. In the HET group, daily HET administration was started on postoperative day 3. Assessments were conducted on postoperative day 3 (baseline), in weeks 2, 4, 6, 8, and 10, and on the day of discharge (or the day of withdrawal) (Fig. 2).

Study design.
The discharge criteria included stable walking ability (including with a cane or walker) or stable mobility by other means (such as a wheelchair) and the point at which the progress of rehabilitation treatment had reached equilibrium.
Safety MeasurementsFor safety, all adverse events were recorded. Of these, adverse events for which a causal relationship with the study drug could not be ruled out were defined as “adverse drug reactions”. Adverse event assessments were also conducted on postoperative day 3 (baseline), in weeks 2, 4, 6, 8, and 10, and on the day of discharge (or the day of withdrawal) (Fig. 2). Liver function (aspartate transaminase, alanine transaminase, alkaline phosphatase, γ-glutamyl transpeptidase, and total bilirubin), kidney function (creatinine and blood urea nitrogen), and potassium were assessed from blood tests. If an adverse event occurred, treatment or appropriate measures were provided. If the study was considered too difficult to continue with observations, administration of the study drug was discontinued.
Sample SizeThe sample size was calculated based on the number of hip fracture patients per year at research facilities and was set as the number of cases considered to be practicable in daily medical practice within the registration period.
Statistical AnalysisDescriptive statistics summarizing the attributes of the study population and efficacy evaluations were conducted using the full analysis set, and safety evaluations were conducted using the safety analysis set. The results were expressed as means ± standard deviations. Changes in the physical activity levels of the two groups between postoperative week 2 and the date of discharge (or the date of withdrawal) were compared using Student’s t-test. Changes in the motivation, ADL, and QOL of the two groups between postoperative day 3 and the date of discharge (or the date of withdrawal) were compared using a Wilcoxon rank sum test and changes in appetite, weight, and pre-albumin were compared using a linear mixed-effects model. The number of days required to reach each grade of walking ability and postoperative length of hospital stay were compared using a Log-rank test, and the proportions of patients who returned home were compared using Fisher’s exact test. In all cases, statistical significance was set at P<0.05. All statistical analysis was outsourced to the third-party organization Icross (Fukuoka, Japan).
There were no significant differences between the control and HET groups in terms of sex, age, height, pre-fracture living circumstances (living at home, other residences, care home paid for by long-term care insurance, nursing home paid for by health insurance), pre-fracture walking ability (walking independently, walking with a cane, walking with a walker, walking by holding onto furniture), fracture site, surgical procedure, MMSE score, previous hip fracture, osteoporosis treatment, comorbidities, concomitant drugs, and cohabitants (Table 1). One patient with femoral neck fracture in the HET group was 65 years old and was highly active both at home and at work and was therefore treated with total hip arthroplasty rather than femoral head replacement.
| Characteristic | Control group (n=18) | HET group (n=20) | P value | |
| Age (years) | 85.1±8.8 | 84.4±8.9 | 0.793 | |
| Sex | Male | 0 (0.0) | 2 (10.0) | 0.488 |
| Female | 18 (100.0) | 18 (90.0) | ||
| Height (cm) | 148.6±6.4 | 150.1±7.9 | 0.526 | |
| MMSE score | 19.5±5.3 | 19.8±6.3 | 0.875 | |
| Fracture site | Neck | 9 (50.0) | 13 (65.0) | 0.512 |
| Trochanter | 9 (50.0) | 7 (35.0) | ||
| Surgical procedure | Osteosynthesis | 12 (66.7) | 10 (50.0) | 0.342 |
| Hemiarthroplasty | 6 (33.3) | 10 (50.0) | ||
| Pre-fracture living | Living at home | 9 (50.0) | 10 (50.0) | 1.000 |
| circumstances | Other residences | 6 (33.3) | 6 (30.0) | |
| Care home paid for by long-term care insurance | 1 (5.6) | 1 (5.0) | ||
| Nursing home paid for by health insurance | 2 (11.1) | 3 (15.0) | ||
| Pre-fracture walking ability | Walking independently | 7 (38.9) | 9 (45.0) | 0.214 |
| Walking with a cane | 6 (33.3) | 4 (20.0) | ||
| Walking with a walker | 5 (27.8) | 3 (15.0) | ||
| Walking by holding onto furniture | 0 (0.0) | 4 (20.0) | ||
| Previous hip fracture | Yes | 2 (11.1) | 2 (10.0) | 1.000 |
| No | 16 (88.9) | 18 (90.0) | ||
| Osteoporosis treatment | Yes | 1 (5.6) | 4 (20.0) | 0.344 |
| No | 17 (94.4) | 16 (80.0) | ||
| Comorbidities | Yes | 4 (22.2) | 5 (25.0) | 1.000 |
| No | 14 (77.8) | 15 (75.0) | ||
| Concomitant drugs | Yes | 17 (94.4) | 17 (85.0) | 0.606 |
| No | 1 (5.6) | 3 (15.0) | ||
| Cohabitant | Yes | 10 (55.6) | 7 (35.0) | 0.328 |
| No | 8 (44.4) | 13 (65.0) | ||
Values are expressed as mean ± standard deviation or numbers (percentage).
P values were calculated using the two-sample t-test (age, height, MMSE score) and Fisher's exact test (other parameters).
There was no significant difference between the two groups in terms of the amount of exercise during daily activity (Fig. 3A), but the level was significantly higher in the HET group (0.03±0.01 Ex) than in the control group (0.02±0.01 Ex) in terms of the amount of exercise during walking in postoperative week 10 (P=0.036, Fig. 3B). There was no significant difference between the two groups in the amounts of time engaged in sedentary activity (<3.0 METs) and moderate activity (3–5.9 METs) in terms of the duration of activity at each intensity level (Fig. 4A,B), but the time engaged in vigorous activity (≥6.0 METs) was significantly longer in the HET group (1.2±0.7 min) than in the control group (0.6±0.4 min) in postoperative week 8 (P=0.026, Fig. 4C). Appetite, assessed in terms of dietary calorie consumption, was significantly higher in the HET group (postoperative week 10: 1374±152 kcal/day, discharge: 1352±175 kcal/day) than in the control group (postoperative week 10: 1165±233 kcal/day, discharge: 1204±253 kcal/day) in postoperative week 10 and upon discharge (P=0.016 for postoperative week 10, P=0.035 at discharge, Fig. 5). There was no significant difference between the two groups in terms of QOL assessed by the EQ-5D-5l (Fig. 6A), but the EQ-VAS score was significantly higher in the HET group (80.4±15.0) than in the control group (64.7±23.9) in postoperative week 6 (P=0.038, Fig. 6B). There was no difference between the two groups in the time taken in achieving the ability to walk using parallel bars or a walker or in recovering pre-fracture walking ability (Fig. 7A,B,D). The time taken to achieve the ability to walk with a cane was significantly shorter in the HET group than in the control group (P=0.042, Fig. 7C). However, there was no significant difference between the two groups in terms of vitality index score, FIM total score, weight, pre-albumin levels, the proportion of patients who were able to return home (Table 2), and postoperative length of hospital stay (Fig. 8).

Effects of HET on the amount of exercise during (A) daily activity and (B) walking. Bars are expressed as mean. Error bars represent standard deviation. Number of patients at each time point is shown in parentheses. *P<0.05 (Student’s t-test).

Effects of HET on the amount of time engaged in (A) sedentary activity (<3.0 METs), (B) moderate activity (3–5.9 METs), and (C) vigorous activity (≥6.0 METs). Bars are expressed as mean. Error bars represent standard deviation. Number of patients at each time point is shown in parentheses. *P<0.05 (Student’s t-test).
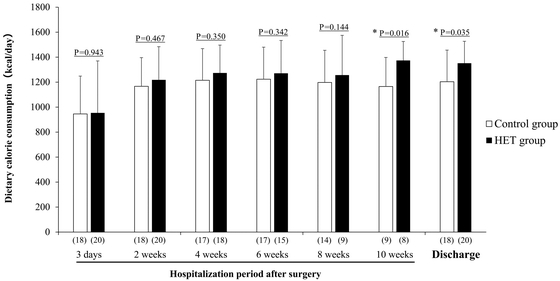
Effect of HET on dietary calorie consumption. Bars are expressed as mean. Error bars represent standard deviation. Number of patients at each time point is shown in parentheses. *P<0.05 (Linear mixed-effects model).
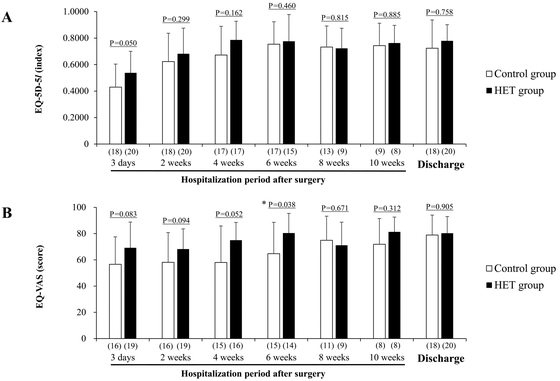
Effects of HET on (A) EQ-5D-5l and (B) EQ-VAS scores. Bars are expressed as mean. Error bars represent standard deviation. Number of patients at each time point is shown in parentheses. *P<0.05 (Wilcoxon rank sum test).

Effects of HET on the number of days required to achieve graded goals in walking ability: (A) walking within parallel bars, (B) walking with a walker, (C) walking with a cane, and (D) pre-fracture walking ability.
| Measurement | Postoperative period | Control group | HET group | P value |
| Vitality index score | 3 days | 8.3±1.7 (18) | 8.6±1.6 (20) | 0.671 |
| 2 weeks | 9.2±1.0 (18) | 8.9±1.5 (20) | 0.662 | |
| 4 weeks | 9.0±0.9 (17) | 8.9±1.1 (17) | 0.986 | |
| 6 weeks | 9.4±1.0 (17) | 8.9±1.4 (15) | 0.432 | |
| 8 weeks | 8.9±1.0 (13) | 8.4±1.7 (9) | 0.651 | |
| 10 weeks | 9.2±0.8 (9) | 9.0±1.2 (8) | 0.797 | |
| Discharge | 9.4±0.7 (18) | 8.7±1.5 (20) | 0.132 | |
| FIM total score | 3 days | 54.7±14.3 (18) | 50.6±20.1 (20) | 0.306 |
| 2 weeks | 70.3±18.8 (18) | 63.9±24.8 (20) | 0.349 | |
| 4 weeks | 80.0±19.2 (17) | 76.4±29.5 (17) | 0.743 | |
| 6 weeks | 85.1±19.6 (17) | 82.0±29.0 (15) | 0.623 | |
| 8 weeks | 81.5±14.8 (13) | 73.1±25.7 (9) | 0.367 | |
| 10 weeks | 81.1±16.6 (9) | 74.9±26.9 (8) | 0.596 | |
| Discharge | 89.1±20.1 (18) | 85.1±28.0 (20) | 0.715 | |
| Body weight (kg) | 3 days | 47.4±6.0 (18) | 48.2±5.6 (20) | 0.683 |
| 2 weeks | 46.2±5.5 (18) | 47.1±5.5 (20) | 0.761 | |
| 4 weeks | 45.3±5.6 (16) | 47.1±5.8 (16) | 0.538 | |
| 6 weeks | 44.8±5.4 (16) | 46.4±6.1 (15) | 0.394 | |
| 8 weeks | 44.1±5.6 (13) | 46.1±7.6 (9) | 0.761 | |
| 10 weeks | 44.6±6.3 (9) | 47.2±7.7 (7) | 0.911 | |
| Discharge | 45.4±5.6 (18) | 46.3±5.6 (19) | 0.799 | |
| Pre-albumin level (mg/dL) | 3 days | 10.4±3.1 (18) | 12.0±4.5 (20) | 0.212 |
| 2 weeks | 18.1±3.8 (17) | 18.6±4.2 (19) | 0.395 | |
| 4 weeks | 16.9±4.2 (17) | 17.4±4.0 (16) | 0.389 | |
| 6 weeks | 16.3±5.3 (14) | 17.4±5.1 (11) | 0.156 | |
| 8 weeks | 15.2±5.2 (13) | 17.1±5.2 (9) | 0.407 | |
| 10 weeks | 14.7±4.1 (5) | 18.0±5.8 (5) | 0.678 | |
| Discharge | 16.5±4.9 (18) | 18.4±4.1 (19) | 0.539 | |
| Home return | Yes | 36.8 (14) | 44.7 (17) | 0.687 |
| No | 10.5 (4) | 7.9 (3) |
Values are expressed as mean ± standard deviation (number) or percentage (numbers).
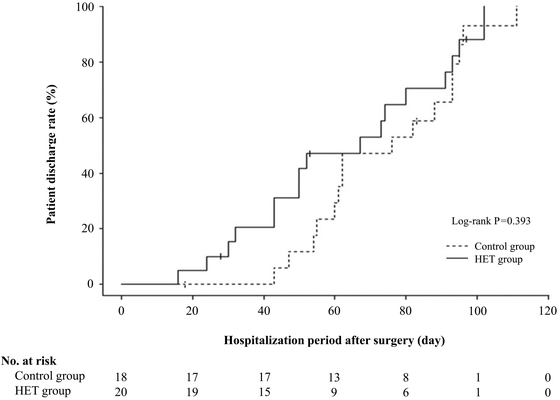
Changes in length of postoperative hospital stay for HET treatment and control groups.
Adverse events occurred in five patients in the control group (five events: hyperkalemia, hypokalemia, anorexia, hypoxemia, and displacement of the fracture) and in seven patients in the HET group (ten events: three cases of hypokalemia and one case each of elevated γ-GTP, dysuria, hypertension, constipation, dry mouth, and proximal humeral fracture and subtrochanteric femoral fracture because of a fall). Adverse drug reactions also occurred in four patients in the HET group (five events: two cases of hypokalemia and one case each of dysuria, constipation, and dry mouth).
In Japan, hip fracture occurs more commonly in women than in men, and its incidence in both sexes peaks in the 85–89 years age group. Surgical treatment is performed in 95% of cases.4) The mortality rate for patients who do not undergo surgery is significantly higher and is lower when patients undergo surgery within a few days of admission.9,10) The Japanese clinical practice guideline on the management of hip fractures state that unless surgery must be delayed because of a medical comorbidity, it should be performed as early as possible.3) The most important characteristic of hip fracture is that surgery must be conducted within a few days of a fracture to the femur, the largest of the limb bones, even in elderly patients who are already frail. This causes further decline in their physical strength postoperatively, but they must still undergo convalescent rehabilitation treatment, involving ambulation, weight-bearing, and exercises for early recovery to their pre-fracture level of ADL. However, elderly women, the group with the highest incidence of hip fracture, are susceptible to nutritional deficiencies, and should they lose weight, they may also experience muscle fatigue, cognitive impairment, and reduced QOL.11) Many patients with hip fracture have low food consumption before their injury, and their nutritional status is often poor. They also tend to eat less during postoperative rehabilitation treatment, making them even more vulnerable to malnutrition. Patients with hip fracture with nutritional deficiencies have reduced function12) and often struggle with postoperative rehabilitation treatment. Therefore, there is significant need for a drug that helps with recovery during postoperative convalescent rehabilitation of elderly female patients (aged ≥80 years) with hip fracture, particularly those with low appetite.
Hip fracture is more common in individuals with low food consumption,13) and poor nutrition caused by loss of appetite is a factor that contributes to its occurrence.14) Women who are already thin show further loss of appetite after a hip fracture, and their energy consumption diminishes.15) Improving the appetite of patients with hip fracture is important for the postoperative recovery of physical strength and function. HET is a Kampo medicine that is widely used to increase physical strength and improve anorexia in elderly people,16) which is an effective approach in increasing the vitality of patients with diminished appetite.17) In a study of cachexia model mice, Yae et al.18) showed that HET prevented decreases in food and water consumption and weight loss. Although no previous study has addressed the efficacy of HET following hip fracture surgery, the results in the present study showed that early postoperative administration of HET improved dietary calorie consumption after hip fracture surgery from postoperative week 10 until discharge. In this study, there was no evidence that HET had any effect on weight or pre-albumin levels, both of which reflect nutritional status. However, we found that HET helps to increase appetite in elderly patients who underwent hip fracture surgery. Our results suggested that increased dietary calorie consumption increases physical strength, which in turn increases physical activity levels in rehabilitation treatment.
Hip fracture is common in infirm elderly people.19) van de Ree et al.20) estimated that 53.3% of patients with hip fracture had been frail prior to the fracture. It is considered that physical activity level may have been already low in many elderly patients with hip fractures because the risk of hip fracture is proportional to the level of physical activity.21,22) Because physical activity levels decline further after hip fracture,23) the degree to which they can be increased in postoperative rehabilitation treatment after hip fracture is crucial. Several studies on the effect of HET on physical activity levels have been reported. In a study of senescent mice using a murine model of malnutrition, Nahata et al.24) showed that HET increased physical activity levels by enhancing amino acid metabolism. Wang et al.25) conducted a study using chronic fatigue syndrome (CFS) model mice and reported that 4 weeks of HET administration improved spontaneous activity. In another study of CFS model mice, Chen et al.26) also showed that spontaneous activity was increased by HET administration. In the present study, we found that vigorous physical activity of 6.0 METs or higher was more common with increased in dietary calorie intake. Therefore, HET may increase physical activity levels by improving appetite.
Elderly patients with low activity levels are considered to have poor QOL before hip fracture,27) and this is further reduced after hip fracture.28,29,30,31) Pre-fracture frailty20) and preoperative anemia32) are associated with diminished post-fracture QOL. The effects of hip fracture on elderly patients, both physically and mentally, are severe.29) Improving QOL must also be considered during postoperative convalescent rehabilitation. Although few studies have addressed the effect of HET on the QOL of frail elderly people, a randomized double-blind placebo-controlled trial by Satoh et al.33) showed that HET administration for two 6-week periods separated by a 2-week washout period improved the QOL of this population. From our results in the present study, daily HET administration from postoperative day 3 increased the EQ-VAS score in postoperative week 6, indicating that it improved the QOL of elderly patients with hip fracture. Our results showed that improvement in the QOL because of HET administration occurred 2 weeks before appetite and physical activity levels improved. Given that some patients were discharged from the hospital during this 2-week period, the populations at each time point were not identical and comparisons could not be made. However, it is considered that improvements in QOL were related to improvements in appetite and physical activity levels. Therefore, it is likely that early improvement in QOL is important in the postoperative convalescent rehabilitation treatment of elderly patients with hip fracture.
Osteoporosis frequently occurs in elderly women and may be the underlying condition behind hip fracture. Bone mass decreases in post-menopausal women because of the activation of osteoclasts. Progressive osteopenia increases the risk of fragility fractures, such as hip fracture. Secondary fracture prevention is required for hip fracture patients soon after the initial fracture,19) and bisphosphonates and other osteoporosis treatments are widely used to prevent osteopenia. Recent studies have shown that HET suppresses bone mass loss. In a study of model mice with ovaries removed, Ochiai et al.34) showed that HET suppresses osteopenia by inhibiting osteoclast activation. Although further clinical studies are required, these findings suggest that HET may be useful against osteoporosis.
Further investigation is required regarding the improvement in activity levels that preceded the improvement in appetite. In this study, with an observation period of less than 2 months, we did not observe any clear effect of HET on ADL. However, HET administration in the early postoperative period was effective in improving QOL, physical activity level, and appetite for hip fracture patients with reduced appetite and physical strength caused by the high invasiveness of fracture and surgery over a short period. It is important to note that the effects of HET were only observed from postoperative week 6 until discharge, which was more than 1 month after the start of HET administration. Nakada et al.35) reported that HET administration for a 2-week period had no apparent effects, although the effects were evident after a 4-week administration period, indicating that long-term administration is necessary. Although it is unclear why it takes time for the effects of HET to appear after the start of the administration, our results also suggested that an administration period of at least 1 month is required for its effects to become evident.
Hypokalemia because of HET was evident in 2 of the 20 patients (10%). Therefore, potassium levels must be monitored regularly during HET treatment after hip fracture surgery.
This study has some limitations. First, the study had a small sample size, with only 38 patients (28%) included in the analysis after 135 patients were initially assessed. The most frequent reason for exclusion was cognitive impairment (MMSE score <10). Many hip fracture patients are cognitively impaired, and Alzheimer’s disease increases the risk for hip fracture by 2.5 times.36) This study required patients to have a certain level of understanding of the study and the ability to respond to questions. The requirement for an MMSE score higher than 10 reduced the sample size.37) Second, this was an open-label study without the use of a placebo. Kampo medicines contain multiple crude drugs, and their taste and smell make placebos difficult to prepare. Third, to recruit a wide range of patients in this study, patients with low walking ability prior to fracture were also enrolled. Based on our observed results, it is possible that clearer results may have been obtained if the study had been conducted on patients with a high level of independent activity before the fracture.
Patients with low walking ability prior to fracture are less active and may be discharged from the hospital relatively early. Therefore, we considered that the effects of HET could not be fully demonstrated. However, if a patient with some high level of independent activity becomes less active because of surgery, more effective and rapid improvement in activity can be expected with HET treatment. Therefore, it is suggested some patients will receive benefit from HET administration at the 6-week point. Hip fracture in Japan occurs most frequently in women aged 85–89 years,4) but in the not-too-distant future, after 2040, the main age group is expected to be people aged over 90 years.2,3) The number of hip fracture patients is expected to increase further in the future, and an increasing number of patients will exhibit reduced physical strength, decreased appetite, and shortened life expectancy. For such patients, surgery should be performed within a few days after the fracture injury, and even if physical strength and appetite are further reduced by the surgery, rehabilitation should be performed early after surgery to help them regain their pre-injury lifestyle and activities. Given that hip fracture patients are elderly, they have very little spare capacity in terms of physical strength and appetite. In our results, walking exercise, vigorous activity time, and EQ-VAS each showed one instance of statistical significance over the entire monitoring period. While these results suggest that the benefits of HET treatment were marginal, it is apparent that elderly patients with hip fractures received an overall benefit. Taken together, the results of this study suggest that HET can be used to help elderly hip fracture patients to safely increase their physical strength and appetite during the postoperative recovery period.
Early postoperative HET administration to elderly hip fracture patients improves QOL, physical activity level, and appetite during convalescent rehabilitation treatment from postoperative week 6. With electrolyte monitoring by regular blood tests, HET may be a safe, effective medication for use in convalescent rehabilitation treatment of frail elderly patients with hip fracture.
The authors acknowledge the significant technical contributions by Ryohei Kobayashi, Mitsuto Fukushige, and Toshitaka Kido from Tsumura & Co. The authors also thank the study participants and the staff of Konan Hospital who assisted in the study.
This study was supported by funding from Tsumura & Co.